Little Wound, Long Knife
aka Trauma Tribulation 022
A 43 year-old man had an alcohol-fueled altercation with his better half. He was consequently stabbed with a knife of uncertain length. There was a single stab wound, less than 2 cm long just inferior to the lateral third of his right clavicle. The wound was not actively bleeding, there was no haematoma, and no subcutaneous emphysema or bruits.
His vitals were pulse rate 90/min, blood pressure 120/75 mmHg, respiratory rate 22/min, SpO2 98% OA and he was GCS 15. He had a central trachea, normal chest expansion and resonance on percussion, and normal alveolar breath sounds. His right upper limb was neurovascularly intact. Further head and neck exam was unremarkable.
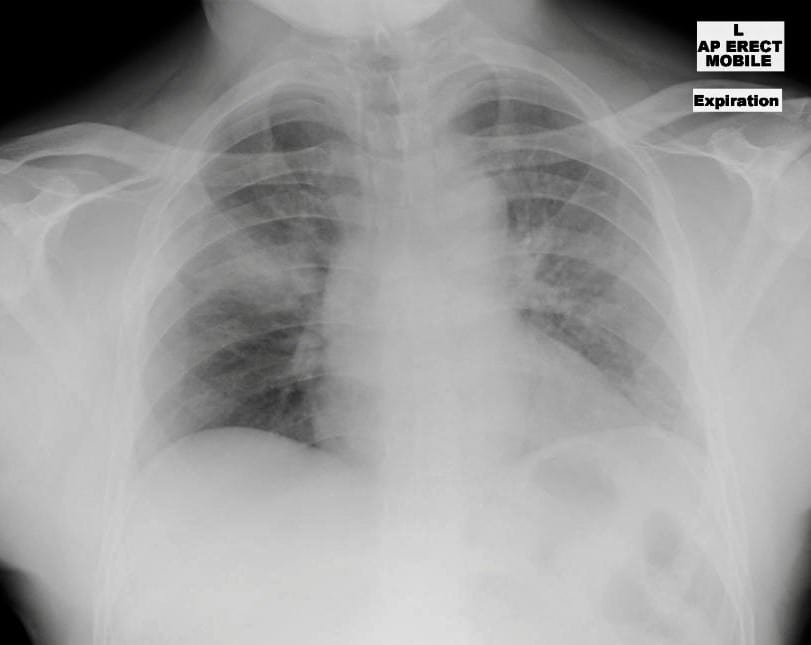
This is his chest x-ray:
Questions
Q1. Describe and interpret the above chest x-ray.
Answer and interpretation
There is a right upper midzone opacity extending from the hilum to the periphery of the right hemithorax between the second and third ribs.
Other chest x-ray findings:
- AP view in expiration (so expansion is poor!)
- Cardiomedistinal contours and mediastinal width are normal (even with the AP view).
- No pneumothroax or hemothorax can be seen.
- There is no visible subcutaneous emphysema.
This opacity could be pre-existing (e.g. pneumonia) but in this context it is traumatic in origin until proven otherwise (i.e. pulmonary hemorrhage or contusion from a stab wound).
Q2. How would you proceed?
Answer and interpretation
Make your ATLS instructor proud:
- Concurrent assessment and management by a trauma team in a fully staffed and equipped resuscitation setting.
- Complete primary survey using the ABCDE approach and attend to resuscitation issues as needed.
- Obtain 2 x large bore IV access (e.g. 16G IV catheters in each antecubital fossa) and send bloods for FBC, UEC, LFTs, coagulation profile, group and hold and a venous blood gas.
- Obtain a more detailed history, including AMPLE (see Trauma Tribulation 014 Q9).
- Complete a detailed secondary survey (always check the back for additional wounds!)
- AAA therapy: ADT (update tetanus immunisation if needed), analgesia (e.g. IV morphine) and antibiotics (e.g. cephazolin 1g IV prophylaxis for penetrating chest trauma)
- Consult the surgeon on call for trauma and arrange further imaging (see Q3)
- Close observation and monitoring for signs of deterioration (especially respiratory or haemodynamic compromise).
An intercostal catheter isn’t needed at this stage.
See Trauma Tribulation 014 for the general approach to major trauma.
Q3. What further imaging is required?
Answer and interpretation
CT chest with contrast and bedside ultrasound.
Bedside ultrasound is useful for early identification of pneumothorax, haemothorax and pericardial effusion.
CT with contrast is the definitive imaging modality used to identify the wound tract and the structures involved. As the trajectory of the stabbing was uncertain, both the chest and neck were imaged. CT angiography allows identification of injuries to major vessels in the chest and neck (e.g. aortic arch, subclavians, carotids and pulmonary vessels).
Suspected penetrating injury to the bronchi and/or esophagus also requires bronchoscopy and/or esophagoscopy.
Although not applicable to this case, remember that chest wounds that extend below the nipples (or the scapulae posteriorly) may enter the abdominal cavity. Unless there is an indication for urgent laparotomy (see Trauma Tribulation 024 Q9), FAST scan and CT abdomen are often needed as well as laparoscopy to identify diaphragmatic injury.
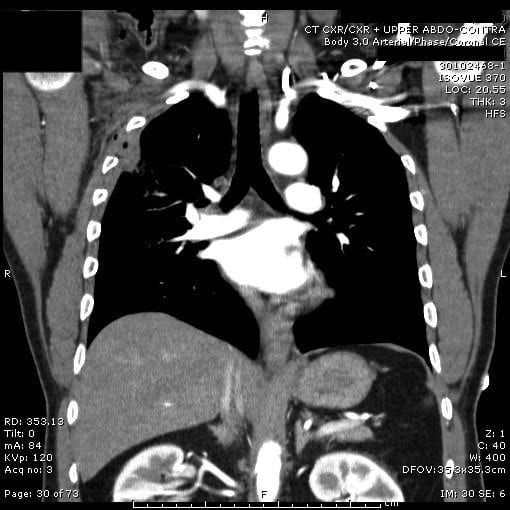
CT Chest was performed
Q4. Describe and interpret the images shown
Answer and interpretation
Reading only one or two slices of a CT scan is a mug’s game — however you may be asked to do this in an exam… 🙁
These are the findings:
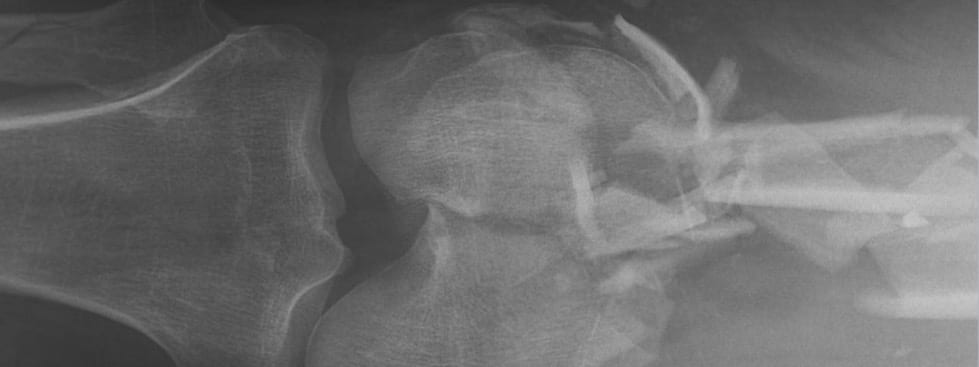
- right-sided penetrating stab wound that enters the thoracic cavity between the 2nd and 3rd ribs and extends for 5.5cm towards the right hilum.
- the wound tract extends down to the confluence of the oblique and horizontal fissure, and there is blood within the fissures (not clearly evident on these images)
- there is pulmonary contusion associated with the wound tract
- there are small locules of gas in the pleural space but no significant pneumothorax
- there are indurated soft tissues in the right axilla as well as some surigcal emphysema
The wound passed anterior and inferior to the subclavian vessels and fell just short of injuring any major hilar vessels. The mediastinum and great vessels were also uninjured.
Q5. How should wounds such as this be appropriately explored?
Answer and interpretation
In this case, with an abnormal chest x-ray (and CT) any wound exploration should take place in the operating theatre and be performed by a doctor with appropriate surgical training.
The management of patients with stab wounds to the chest but otherwise normal vital signs, physical examination and chest x-ray is more controversial. A few case series suggest that if:
- a repeat chest x-ray after as little as 3 hours is normal
- and the patient continues to have normal vital signs and physical examination
then discharge with close outpatient follow up is safe. More recently, studies have been published suggesting that if a CT chest is performed — and it is normal — then there is no need for a repeat chest x-ray after 3 hours.
However, even if the chest x-ray is normal, inappropriate exploration of a wound that passes close to the pleural cavity could inadvertently extend it with nasty consequences. Unless the wound is clearly superficial, a surgical consult is a wise option.
Discretion, as always, is the better part of valor. Follow your institution’s guidelines.
References
Textbooks and Journal Articles
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Kiev J, Kerstein MD. Role of three hour roentgenogram of the chest in penetrating and nonpenetrating injuries of the chest. Surg Gynecol Obstet. 1992 Sep;175(3):249-53. PubMed PMID: 1514160.
- Kerr TM, Sood R, Buckman RF Jr, Gelman J, Grosh J. Prospective trial of the six hour rule in stab wounds of the chest. Surg Gynecol Obstet. 1989 Sep;169(3):223-5. PubMed PMID: 2772791.
- Kiev J, Kerstein MD. Role of three hour roentgenogram of the chest in penetrating and nonpenetrating injuries of the chest. Surg Gynecol Obstet. 1992 Sep;175(3):249-53. PubMed PMID: 1514160.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Magnotti LJ, Weinberg JA, Schroeppel TJ, Savage SA, Fischer PE, Bee TK, Maish GO 3rd, Minard G, Zarzaur BL, Croce MA, Fabian TC. Initial chest CT obviates the need for repeat chest radiograph after penetrating thoracic trauma. Am Surg. 2007 Jun;73(6):569-72; discussion 572-3. PubMed PMID: 17658093.
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- Ordog GJ, Wasserberger J, Balasubramanium S, Shoemaker W. Asymptomatic stab wounds of the chest. J Trauma. 1994 May;36(5):680-4. PubMed PMID: 8189470.
- Seamon MJ, Medina CR, Pieri PG, Fisher CA, Gaughan JP, Bradley KM, McNamara RM, Goldberg AJ. Follow-up after asymptomatic penetrating thoracic injury: 3 hours is enough. J Trauma. 2008 Sep;65(3):549-53. PubMed PMID: 18784567.
- Shatz DV, de la Pedraja J, Erbella J, Hameed M, Vail SJ. Efficacy of follow-up evaluation in penetrating thoracic injuries: 3- vs. 6-hour radiographs of the chest. J Emerg Med. 2001 Apr;20(3):281-4. PubMed PMID: 11267818.
FOAMed resources
- Trauma Professional’s Blog — When can you close that stab wound?
- Trauma Professional’s Blog — How to read a stab wound
- Trauma! Are you prepared?
- Trauma! Initial Assessment and Management
- Trauma! Chest Injuries I and Trauma! Chest Injuries II
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC