Ultrasound Case 045
Presentation
A 55 year old woman with hepatitis C and known cirrhosis presents with right upper quadrant pain. You ultrasound her gallbladder.
View 3
Describe and interpret these scans
IMAGE INTERPRETATION
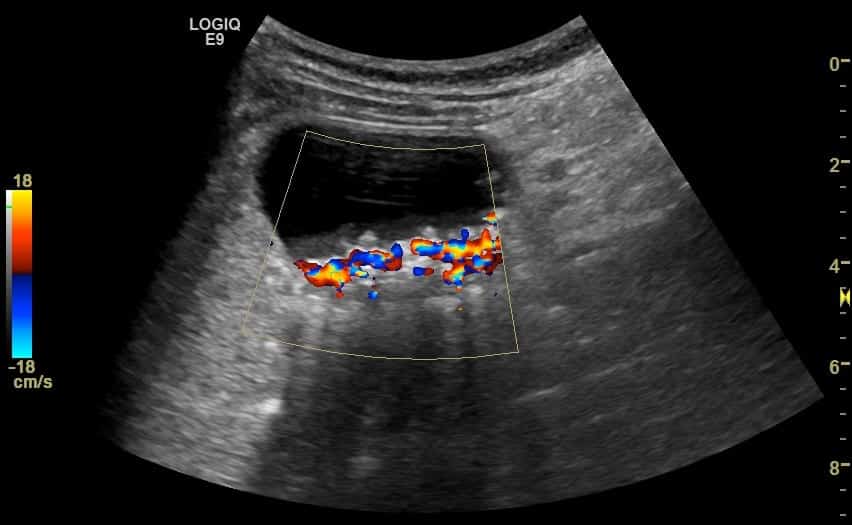
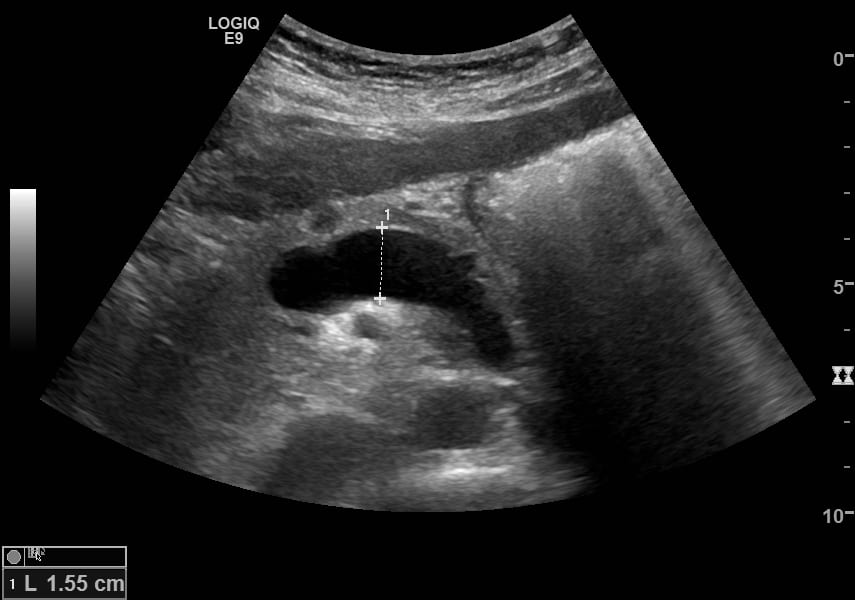
Image 1: Longitudinal then transverse fanning through the gallbladder. The distended gallbladder contains some small rather aesthetically pleasing stones layered dependently below a layer of sludge. The wall is slightly thickened and the patient has Sonographic Murphy’s sign. She has features of acute cholecystitis. You also notice a large hypoechoic tubular structure running through the liver adjacent to the gallbladder.
Image 2: Gallstones demonstrate twinkle artifact.
Image 3: Following the markedly dilated recanalised umbilical vein through the falciform ligament and along the anterior abdominal wall to the umbilicus, and then down to the left inferior epigastric vein which joins the left common femoral vein.
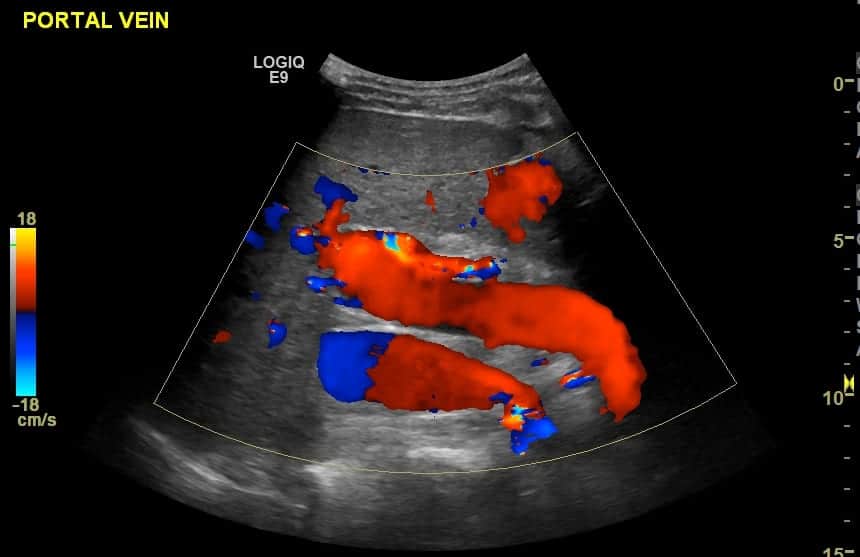
Image 4: Dilated portal vein at 17.5mm (≤13mm).
Image 5: Flow remains toward the liver (hepatopetal) as the recanalised umbilical vein allows maintenance of forward flow through the portal vein. If it had not recanalised flow would almost certainly have reversed, termed hepatofugal.
Image 6: Dilated splenic vein at 15.5mm (≤10mm).
Image 7: Panoramic image of the spleen showing splenomegaly at 20.7cm (≤14xm).
CLINICAL CORRELATION
Cholecystitis, liver cirrhosis, portal hypertension and splenomegaly
Portal venous pressure is usually 5-10mmHg. Causes of portal hypertension
- Prehepatic – where there is thrombosis or narrowing of the portal vein and subsequent hypertension in vessels supplying the portal vein.
- Hepatic – in cirrhosis there is fibrosis and destruction of the normal hepatic sinusoids preventing normal forward flow and resulting in raised pressures within the portal venous system
- Post hepatic where Budd Chiari syndrome or heart failure impede flow causing back up of pressures that are transmitted to the portal venous system.
Understanding the changes that occur with cirrhosis and portal hypertension is attempted through images 8-10.
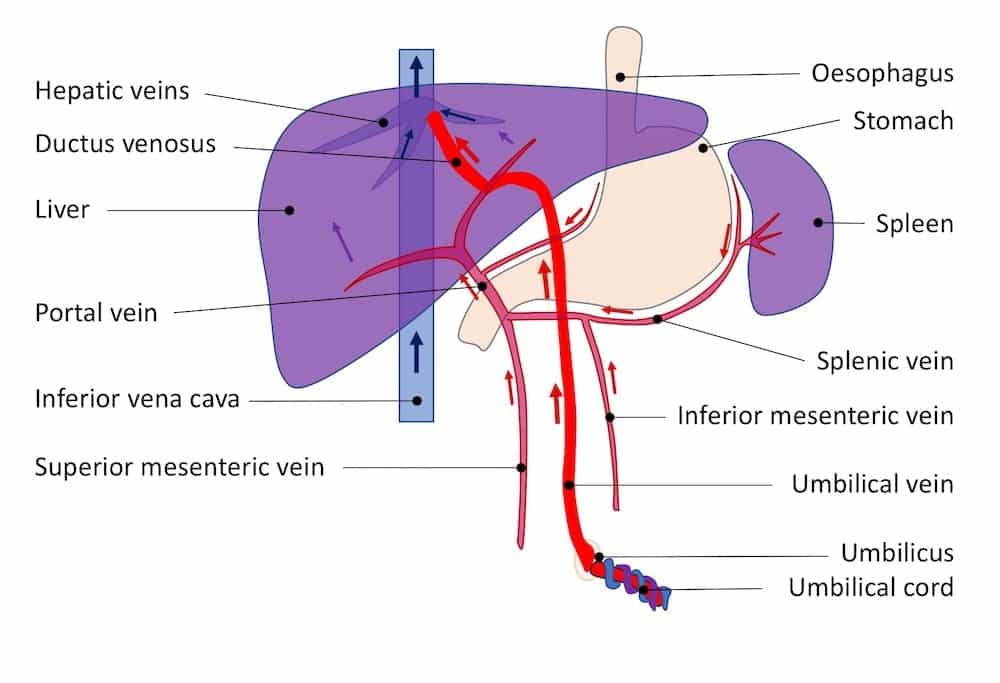
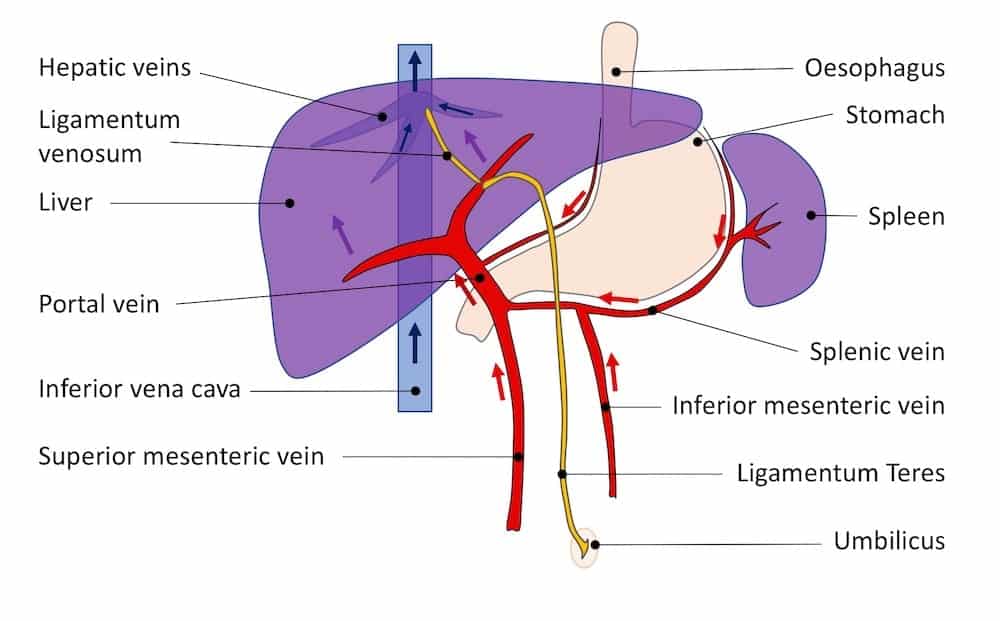
Image 8: Normal fetal splanchnic blood flow
In fetal circulation the placenta returns oxygenated, nutrient rich blood to the fetus via the umbilical vein. This travels through the anterior abdominal wall and dives into the liver, joining the portal vein and then going on as the ductus venosus to the IVC. The mesenteric vessels do not require large amounts of blood flow as the intestines are not required for digestive purposes in utero. Similarly the liver is still immature and does not need to provide all the functions of the adult liver. Blood essentially bypasses the hepatic sinusoids by passing through the ductus venosus.
Image 9: Normal adult splanchnic circulation.
After birth the umbilical vein and the ductus venosus contract, close and fibrose, becoming ligamentum teres and the ligamentum venosum. Flow increases through the mesenteric veins and portal vein, then flows through the hepatic sinusoids and on into the hepatic veins to join the systemic venous circulation.
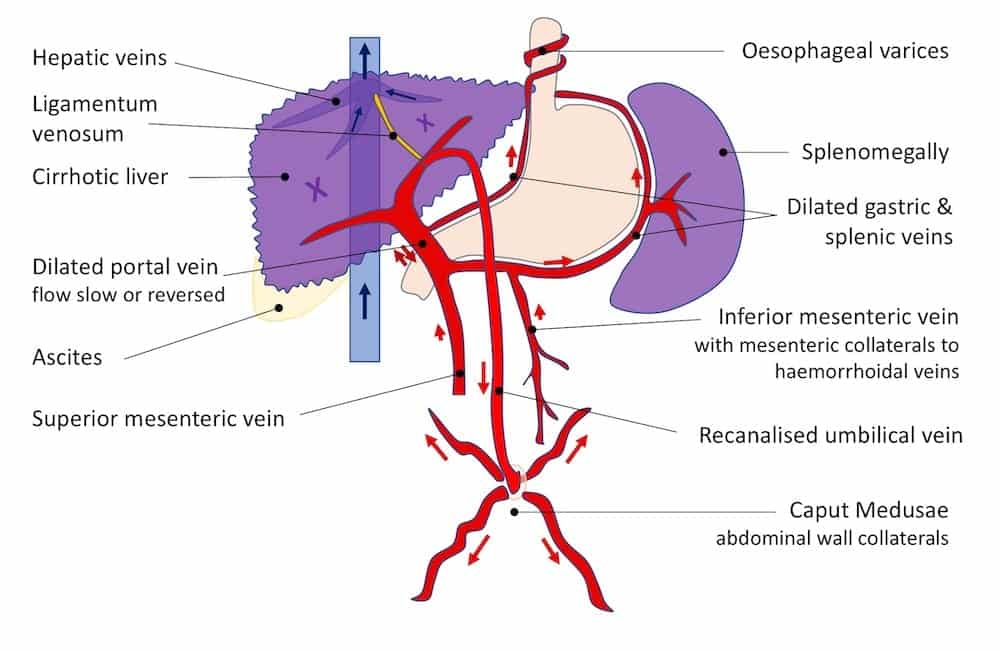
Image 10: Cirrhosis with portal hypertension and changes in splanchnic circulation
In cirrhosis hepatic sinusoidal flow is blunted. The pressure in the portal venous circulation rises, flow slows, and collaterals form.
The exact response varies from patient to patient but can include the following:
- Dilation and slowing or reversal of flow in the portal vein.
- Recanalisation of the umbilical vein which traverse the liver via the falciform ligament then enters the anterior abdominal wall. Once it reaches the umbilicus dilated collaterals in the anterior abdominal wall flow upward and downward to reach the systemic circulation – this creates the “caput Medusae” appearance. In addition raised portal venous pressures cause the splenic and gastric venous dilation and formation of collaterals around the oesophagus creating varices. Flow through the inferior mesenteric vein can connect with the systemic venous circulation via the haemorrhoidal veins resulting in haemorrhoids.
Ascites is common due to poor hepatic synthetic function of protein particularly albumin and hence reduced oncotic pressure, as well as raised venous pressures.
[cite]
TOP 100 ULTRASOUND CASES
An Emergency physician based in Perth, Western Australia. Professionally my passion lies in integrating advanced diagnostic and procedural ultrasound into clinical assessment and management of the undifferentiated patient. Sharing hard fought knowledge with innovative educational techniques to ensure knowledge translation and dissemination is my goal. Family, wild coastlines, native forests, and tinkering in the shed fills the rest of my contented time. | SonoCPD | Ultrasound library | Top 100 | @thesonocave |




I am currently an ultrasound tech student reviewing cases as a way to study. I have been deep diving into these top 100 cases and this has been my most favorite!! Dr. James Rippey, the way you broke down the pathologies in the clinical correlation was so beyond helpful. I am not sure if anyone can see these comments or replies, but if so, keep up the great work! These cases, alongside the diagrams and amazing interpretations, are helping so many students at my school. I truly appreciate it!