Abdominal CT: Flank pain
Addressing flank pain or renal masses
Reviewing the alternative CT imaging strategies for the genitourinary system and a stepwise approach to evaluating the CT KUB
Kidney stones
When evaluating for kidney stones, we look at the non-contrast series, scanning the kidneys, ureters, and bladder for renal stones.
One of the hallmarks indicating that a renal stone is causing obstruction is hydronephrosis – where the renal pelvis and calyces become dilated. So, when you’re looking at the non-contrast image series, start by looking for hydronephrosis and stones.
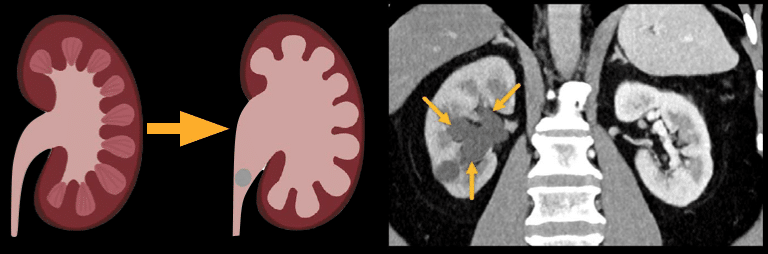
Example 1: Right hydronephrosis
In the example below, you can compare the dilated collecting system and calyces in the right kidney to the normal left kidney, where you can barely see the calyces. This indicates obstruction of the right ureter
Example 2: Right hydronephrosis
The right kidney is enlarged. If we follow the right ureter downward, we can identify the obstructive stone in the distal ureter.
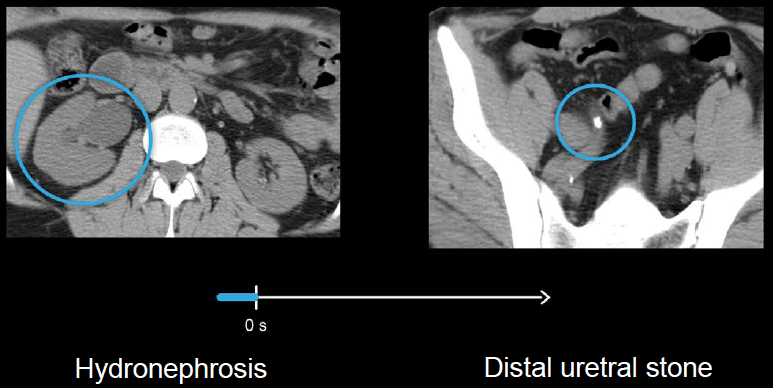
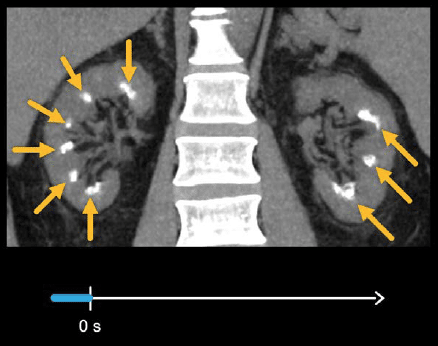
Example 3: medullary nephrocalcinosis
You will also encounter non-obstructive stones and metabolic stone disease. The example below shows medullary nephrocalcinosis, with numerous small, bright stones forming on the renal pyramids in both kidneys.
Kidney masses
Review the nephrographic images, focusing on the kidneys and being on the lookout for abnormal enhancement and renal masses.
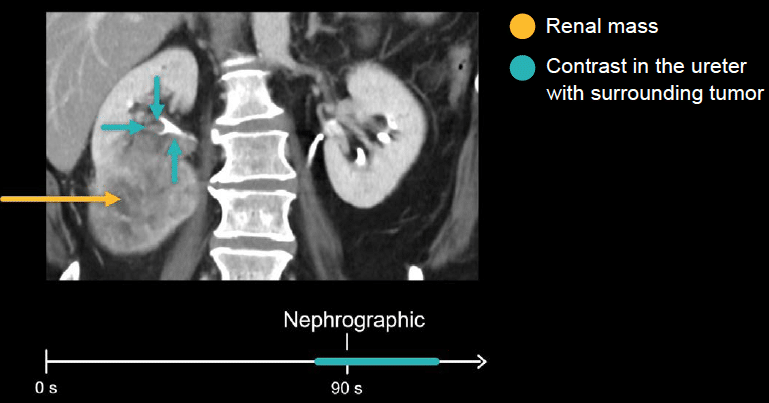
Example 3: renal mass
There is a large renal mass in the patient’s right kidney. The mass is invading the collecting system and causing haematuria.
Notice the contrast in the ureter with a tumour surrounding it. It is important to remember to screen for renal and urothelial cancers with a CT urogram if the patient presents with blood in the urine.
Collecting system, ureters, and bladder
We finish our checklist with the collecting system, ureters, and bladder. Here, we’re looking for abnormal thickening and enhancement in the nephrographic phase and filling defects in the excretory phase. Filling defects can indicate a urothelial tumour, but it can also indicate blood, debris, or pus.
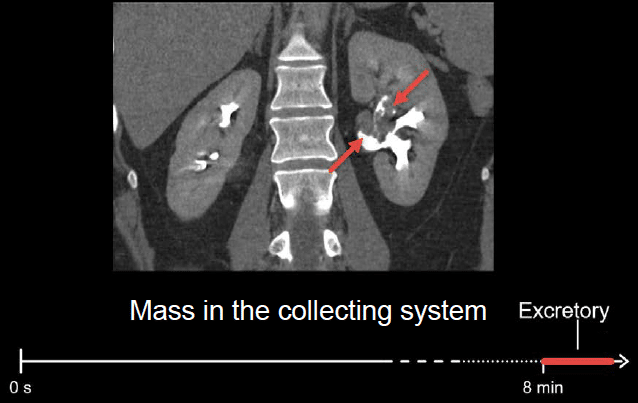
Example 4: collecting system
There is an irregularly shaped mass filling the collecting system and causing it to be slightly dilated. Because it is surrounded by contrast-opacified urine, we are able to see the mass
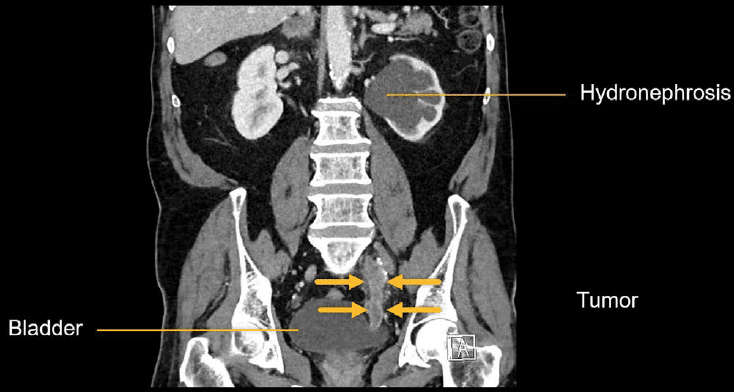
Example 5: distal ureter obstruction
There is severe left hydronephrosis, indicating obstruction of the left kidney. If we follow the left ureter downward, there is a large obstructive tumour filling the distal ureter just before the bladder.
While filling defects are often best seen on the excretory phase images, the nephrographic phase is better for detecting abnormal wall thickening and enhancing masses of the ureters.
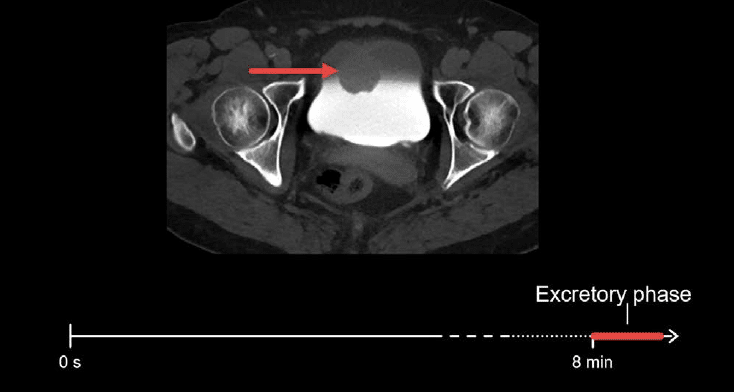
Example 6: bladder mass
There is a rounded mass projecting into the bladder. Notice how only part of the bladder is filled with contrast. This layering is due to the increased density of contrast-opacified urine which layers below the non-enhanced urine.
Remember the checklist approach when reviewing CT urograms as it will remind you to look for all important abnormalities in the kidneys, ureters, and bladder that may be causing blood in the urine.
This is an edited excerpt from the Medmastery course Abdominal CT Essentials by Michael P. Hartung, MD. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Hartung MP. Abdominal CT: Common Pathologies. Medmastery
- Hartung MP. Abdominal CT: Essentials. Medmastery
- Hartung MP. Abdomen CT: Trauma. Medmastery
References
- Top 100 CT scan quiz. LITFL
Radiology Library: Abdominal CT Basics
- Hartung MP. Abdominal CT: Phases. LITFL
- Hartung MP. Abdominal CT: Cancer staging. LITFL
- Hartung MP. Abdominal CT: GU imaging. LITFL
- Hartung MP. Abdominal CT: Urogram. LITFL
- Hartung MP. Abdominal CT: Cystogram. LITFL
- Hartung MP. Abdominal CT: Flank pain imaging. LITFL
Abdominal CT interpretation
Assistant Professor of Abdominal Imaging and Intervention at the University of Wisconsin Madison School of Medicine and Public Health. Interests include resident and medical student education, incorporating the latest technology for teaching radiology. I am also active as a volunteer teleradiologist for hospitals in Peru and Kenya. | Medmastery | Radiopaedia | Website | Twitter | LinkedIn | Scopus

