ECG Case 124
A 24-year-old female presents following a syncopal episode in the context of alcohol consumption. She describes a prodrome of 10-15 seconds of lightheadedness.
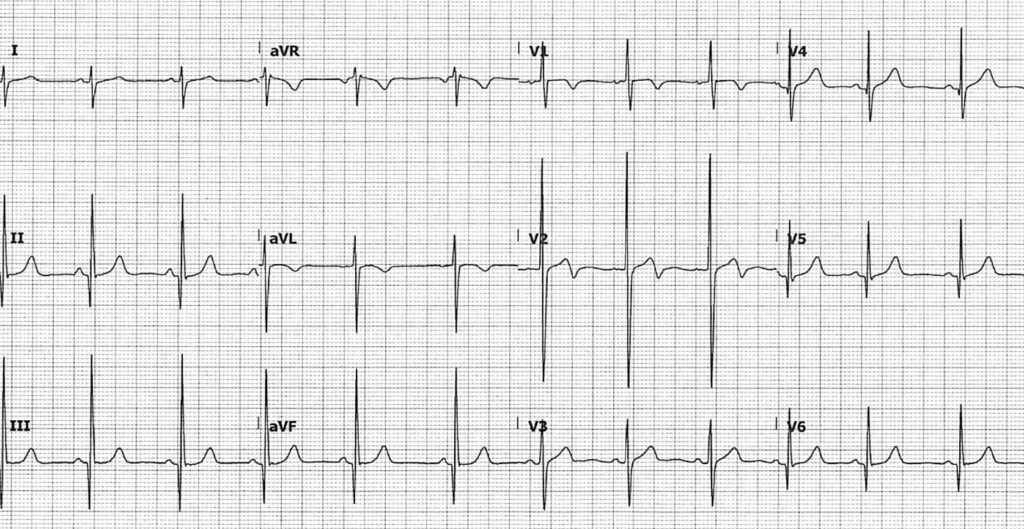
An ECG is performed at triage:
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
- Normal sinus rhythm, rate 72 bpm
- Normal PR interval
- Deep, narrow Q waves in inferior (II, III, aVF) and lateral (V5-V6) leads
- Large QRS complex in V2 with a biphasic T wave
- Voltage criteria for left ventricular hypertrophy (LVH)
- Normal QTc ~430ms
What is the diagnosis?
Reveal answer
The combination of these ECG features is concerning for septal hypertrophy, and in the context of syncope in a young adult, hypertrophic cardiomyopathy (HCM).
You perform a basic bedside echo to correlate with ECG findings:
Parasternal long axis (PLAX)
Parasternal short axis (PSAX)
Apical 4 chamber (A4C)
What is your interpretation?
Reveal answer
Parasternal long axis (PLAX) view
- LV function appears grossly normal
- No aortic root dilatation
- There is thickening of the interventricular septum (IVS) — this was measured at 15mm at end-diastole (normal range < 0.9mm in females)
Parasternal short axis (PSAX) view
- Thickening of the IVS is again noticeable
- There is no flattening of the IVS that would indicate high right-sided pressures
Apical four chamber (A4C) view
- RV systolic function and size appears grossly normal, with TAPSE > 16mm and RV:LV ratio < 2:3

TAPSE stands for Tricuspid Annular Plane Systolic Excursion. It is a measurement of RV longitudinal function. An M-mode measurement is taken through the tricuspid valve annulus. A shortening of > 16mm correlates with normal RV longitudinal function.
OUTCOME
The patient was admitted under cardiology for monitoring and workup for hypertrophic cardiomyopathy (HCM).
Formal inpatient echocardiography revealed similiar findings, demonstrating:
- Asymmetric thickening of the basal-mid anteroseptum
- Mild chordal systolic anterior motion (SAM) with obstruction
Cardiac MRI confirmed the diagnosis of HCM.
CLINICAL PEARLS
Patients with HCM can have a normal ECG
Echocardiography is more sensitive than the ECG in diagnosing HCM, and around 5% of patients with echocardiographic evidence of HCM will have a normal ECG. These patients generally have a less severe phenotypic expression of disease, but early diagnosis is important to ensure close monitoring and prevention of complications. Patients with a normal ECG but clinical and echocardiography features concerning for HCM should undergo further investigation with cardiac MRI.
HCM presents with a wide spectrum of disease
Formerly known as hypertrophic obstructive cardiomyopathy, the majority (75%) of HCM cases are mild and are not associated with LVOT obstruction. Patients with HCM present with a broad spectrum of disease and symptomatology — they may remain asymptomatic until diagnosis or sudden cardiac death, or present with progressive symptoms of exertional chest pain or shortness of breath. Exertional syncope is the most concerning symptom and suggests dynamic left ventricular outflow tract (LVOT) obstruction +/- ventricular dysrhythmia.
The clinical diagnosis of HCM is based on the presence of left ventricular hypertrophy (LVH), typically defined by an end-diastolic ventricular septal thickness ≥ 13mm in adults, occurring in the absence of any inciting stimulus such as hypertension or aortic stenosis. The most commonly observed pattern is asymmetrical thickening of the interventricular septum. However, the degree and distribution of hypertrophy is variable, ranging from mild hypertrophy (13-15mm) to extreme myocardial thickening (30-60mm).
Adolescents and adults that are competitive athletes may demonstrate significant physiological left ventricular hypertrophy (≥ 13mm) which can mimic HCM. In these patients, an enlarged LV cavity, and symmetrical LV hypertrophy, favours a physiological cause of changes seen. Cardiac MRI is required to definitively differentiate between the two causes.
Q waves: differentiating HCM versus MI
Deep Q waves seen in HCM are the result of depolarisation through a hypertrophied septum. Although thickened, conduction through this tissue is normal. This produces deep, narrow Q waves with a different morphology to those of myocardial infarction:
- Infarction Q waves are typically > 40 ms duration
- Septal Q waves in HCM are < 40 ms
- HCM presents with a wide spectrum of disease, ranging from mild septal hypertrophy with no symptoms, to severe myocardial thickening causing progressive symptoms of heart failure
- Patients with HCM can have a normal ECG. Bedside echocardiography may assist in identifying sinister pathology in the patient presenting with syncope
Further reading
Related topics
Expert Review
- Smith SW. Hypertrophic Cardiomyopathy or Normal Variant?. Dr Smith’s ECG Blog. 2019 January
References
- McLeod et al. Outcome of Patients With Hypertrophic Cardiomyopathy and a Normal Electrocardiogram. J Am Coll Cardiol. 2009 Jul, 54(3):229-233
- Elliott et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The task force for the diagnosis and management of hypertrophic cardiomyopathy of the ESC. European Heart Journal. 2014;35:2733–2779
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Interventional cardiologist, ECG and hemodynamics fan. MD, Assoc. Prof. at Marmara University, Pendik T&R Hospital, Assoc. Editor at Archives of TSC, ESC National Prevention Coordinator



Thank you for the great case. Especially appreciate the combining of echo loops with the ecg findings. Well done.