ECG Case 123
A 78-year-old man presents following an episode of right axillary pain. Past history includes hypertension, T2DM and smoking. HR 66, BP 137/75, SpO2 95%.
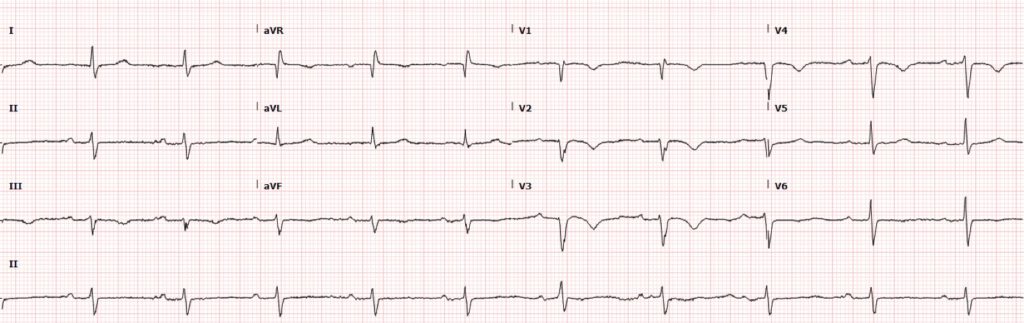
He is pain-free when the below ECG is taken:
His initial high sensitivity troponin returns elevated at 305ng/L.
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
- Normal sinus rhythm, rate 66 bpm
- Borderline left axis deviation
- 1st degree AV block
- Non-specific intraventricular conduction delay, with QRS > 100ms (not fulfilling criteria for left anterior fascicular block)
- No significant ST segment changes
- Symmetrical T-wave inversion in leads V1-V4
What is the diagnosis?
Reveal answer
In the context of self-resolved chest pain and cardiac risk factors, T-wave inversion seen here in V2-V3 may raise immediate suspicion for Wellens syndrome. The T-wave morphology however is not entirely characteristic of a type B Wellens pattern, which usually presents with deeper T-wave inversion.
Differentials for right precordial T-wave inversion in patients with symptoms of acute coronary syndrome (ACS) include:
- Ischaemia (including Wellens syndrome)
- Posterior myocardial infarction
- Right ventricular strain
There are other ECG features here suggestive of RV strain – can you spot them?
Reveal answer
T-wave inversion in lead III and V1
Right ventricular strain pattern can be difficult to differentiate from ischaemia on the basis of right precordial T-wave inversion alone. When there is associated T-wave inversion in leads facing the right ventricle, especially lead III, this becomes highly specific for pulmonary embolism (PE).
Clockwise rotation
There is a shift of the R/S transition point towards V6, with a dominant S wave in V6, implying rotation of the heart due to right ventricular dilatation.
CLINICAL PEARLS
Right precordial T-wave inversion: Differentiating ACS and PE
With increasing awareness of the ECG changes of Wellens syndrome in recent years, it is easy for premature closure to occur in the diagnostic process with the above presentation. In patients with symptoms of ACS and right precordial T-wave inversion, we must always consider acute RV strain as a differential in addition to ischaemia/infarction.
The finding of associated T-wave inversion in leads III and V1 has demonstrated a high specificity (99%) for differentiating PE from ACS. When right precordial T-wave inversion is present, the clinician should be prompted to look for other ECG features suggestive of RV dilatation, including clockwise rotation and right axis deviation. In patients where clinical suspicion for PE is high, right precordial T-wave inversion may be a useful marker of severity, associated with massive PE and high pulmonary pressures.
The type B pattern of Wellens syndrome typically presents with deep T-wave inversion. An episode of self-resolved chest pain and raised troponin implies infarction and reperfusion has occurred, and thus changes should be dynamic. Serial ECGs in this patient did not demonstrate change in T-wave morphology in right precordial leads, and the shallow nature of inversion seen is atypical for Wellens syndrome.
Understanding clockwise rotation
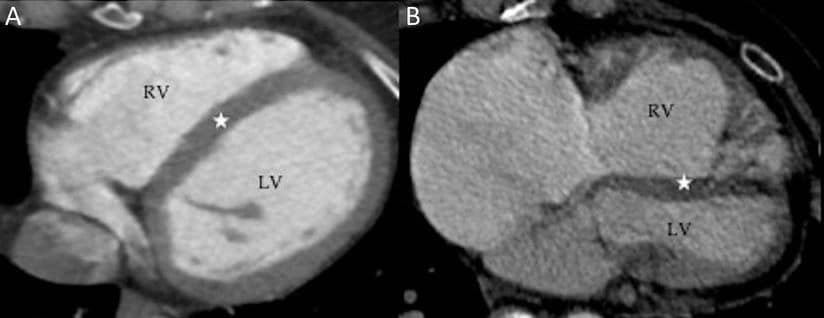
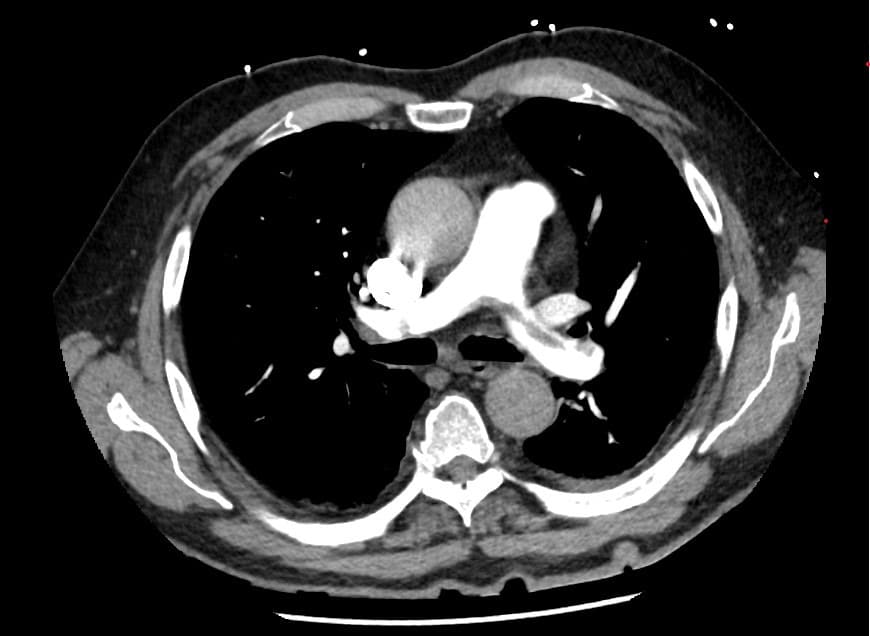
Right: RV dilatation and hypertrophy compressing the LV, creating “clockwise” rotation of the heart
The term “clockwise rotation” describes the apparent rotation of the heart as viewed from below in standard CT/MRI cross-sectional imaging views. High pulmonary pressures in PE cause acute RV pressure overload and dilatation, compressing the interventricular septum (IVS). Ensuing RV dysfunction and hypokinesis worsens these changes, particularly in the apical region. Leads V5-6, which usually face the LV wall and reflect LV depolarisation directly, are subsequently orientated over the IVS. The R/S transition point thus shifts rightwards towards V6.
What about SIQIIITIII?
The “classic” SIQIIITIII finding lacks supporting literature as a sensitive and/or specific marker for PE, but it’s individual components can serve as useful prompts to examine for other ECG features of PE.
A prominent S wave in lead I, as seen in this case, is simply a reflection of clockwise rotation and/or right axis deviation. T-wave inversion in lead III as an isolated finding can be a normal variant, but in the context of right precordial T-wave inversion is highly specific for PE. Similarly, Q waves in lead III may be a normal variant, or a reflection of regional RV ischaemia and/or infarction secondary to acute pressure overload.
Summary
- In patients with symptoms of ACS and right precordial T-wave inversion, associated T-wave inversion in leads facing the right ventricle (III and V1) is highly specific for PE
- Type B pattern of Wellens syndrome presents with deep, symmetrical T-wave inversion. In the context of chest pain and a raised troponin, ECG changes are usually dynamic
- ECG features of acute right heart strain simply reflect a sudden increase in pulmonary pressures, and can be seen in any cause of hypoxia due to pulmonary hypoxic vasoconstriction
FURTHER READING
Related topics
Expert Review
- Smith SW, Meyers P. A crashing patient with an abnormal ECG that you must recognize. Dr Smith’s ECG Blog. 2018 March
References
- McGinn S, White PD. Acute cor pulmonale resulting from pulmonary embolism its clinical recognition. JAMA. 1935;104(17):1473–80.
- Ferrari et al. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads–80 case reports. Chest. 1997 Mar;111(3):537-43
- Kosuge et al. Electrocardiographic differentiation between acute pulmonary embolism and acute coronary syndromes on the basis of negative T waves. Am J Cardiol. 2007 Mar 15;99(6):817-21
Image sources
- Mak et al. Right ventricle in adulthood: CT and MR assessment. Postgraduate Medical Journal. 2009, Volume 96, Issue 1138
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Interventional cardiologist, ECG and hemodynamics fan. MD, Assoc. Prof. at Marmara University, Pendik T&R Hospital, Assoc. Editor at Archives of TSC, ESC National Prevention Coordinator

![Evolution of T-wave inversion [A-D] after coronary reperfusion in STEMI reperfusion and in Wellens syndrome (NSTEMI)](https://litfl.com/wp-content/uploads/2018/08/Evolution-of-T-wave-inversion-A-D-after-coronary-reperfusion-in-STEMI-reperfusion-and-in-Wellens-syndrome-NSTEMI-1024x352.png)

