FFS: Lateral medullary syndrome
Lateral medullary syndrome (also known as Wallenberg syndrome) is is a stroke syndrome, which develops as a result of infarction in the region of the brainstem supplied by the posterior inferior cerebellar artery (PICA), which is a branch of the vertebral artery.
Affected structures include:
- Lateral aspect of the medulla oblongata
- Inferior cerebellar peduncle
- Infero-lateral cerebellum.
It is an uncommon syndrome.
The diagnosis is often missed, (even by experienced neurologists), but it is important to understand the syndrome in order to fully appreciate the potential extent of disability that can be suffered by the patient, (over and above the most obvious feature of ataxia)
Thrombolysis is an option in the astute setting, however, it has a high degree of risk within this region. Hemorrhagic complications within the brainstem will carry a significant risk of death.
The risk -versus benefit of this intervention must be carefully assessed by expert neurologist experienced in stroke neurointervention
History
Adolf Wallenberg (1862-1949), a German neurologist, described the syndrome in 1895 and published a precise anatomical description in 1901. However, the first recorded case was by Gaspard Vieusseux (1746-1814), who described his own symptoms at a medical meeting in Geneva in 1808.
Epidemiology
Lateral medullary syndrome is the most common and important syndrome related to intracranial vertebral artery occlusion.
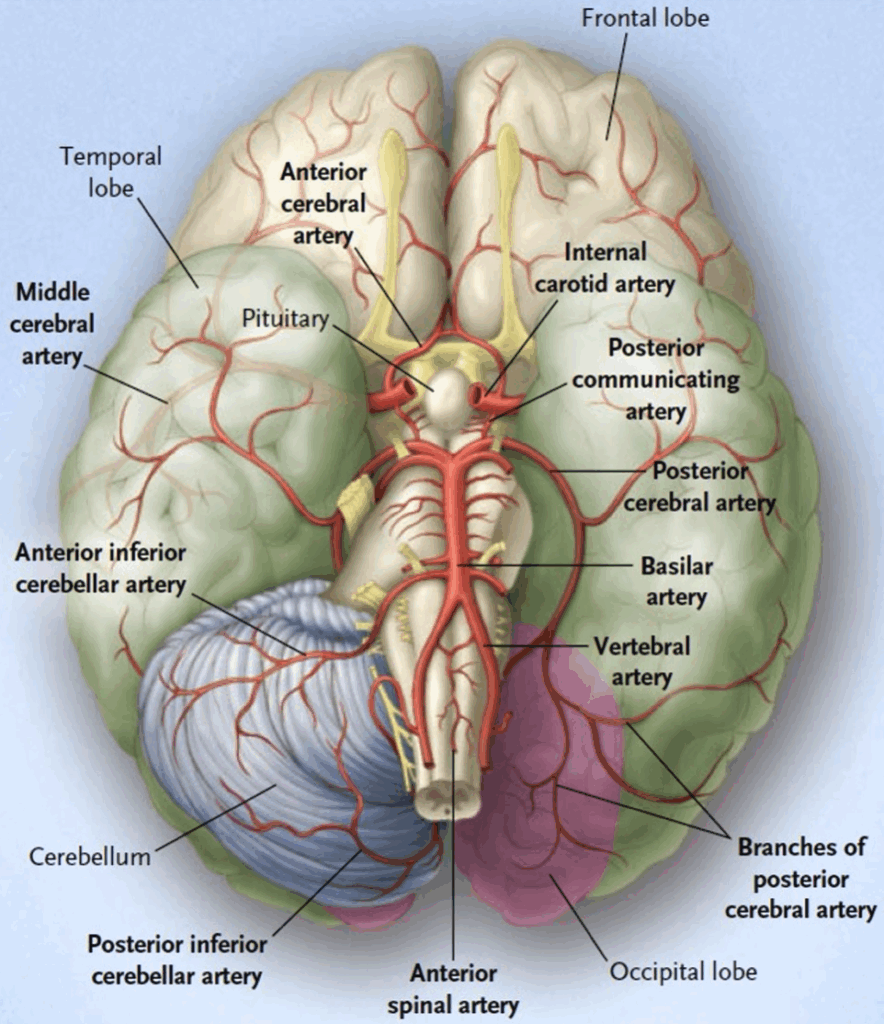
Anatomy
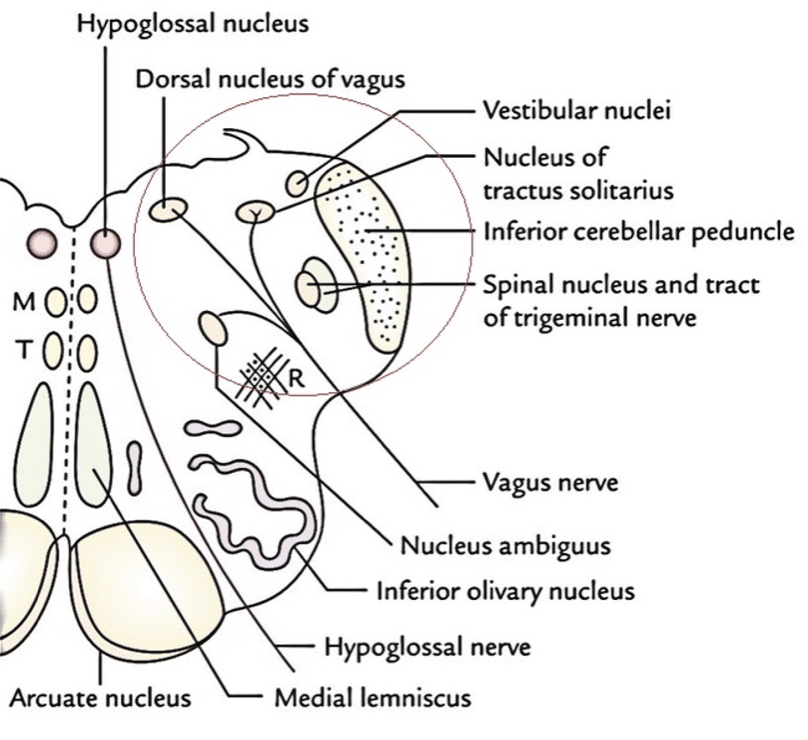
The lateral medulla contains:
- Motor nuclei for cranial nerves IX, X, and XI.
- Sensory nucleus (nucleus solitarius) for cranial nerves VII, IX, and X.
- Trigeminal sensory nucleus, mainly in the pons but extending through the brainstem.
Note: The hypoglossal and dorsal vagal nuclei are in the medial medulla.
Pathophysiology
The syndrome results from occlusion—commonly thrombosis or embolism, rarely dissection—of vessels supplying the lateral medulla and infero-lateral cerebellum.
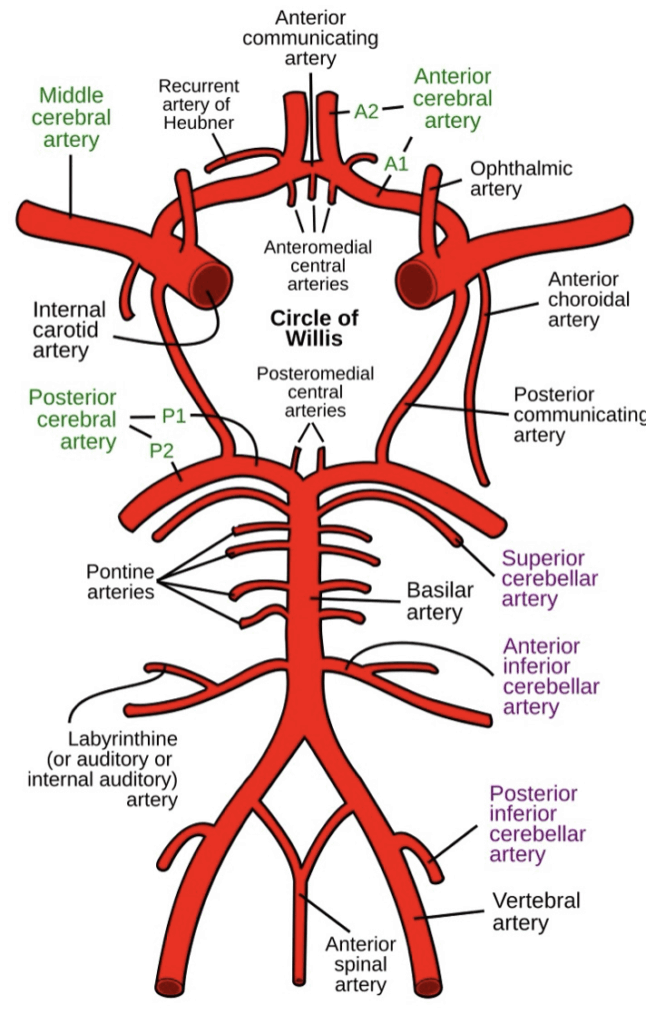
Arterial supply includes:
- Vertebral artery branches
- Posterior inferior cerebellar artery (PICA) — supplies the dorsal lateral medulla and posterior medial cerebellum
Most cases are due to vertebral artery occlusion; less often due to PICA occlusion.
Clinical features
Symptoms
Typically acute onset of:
- Vertigo
- Vomiting
- Dysphagia
- Dysarthria
- Ataxia
Signs
| Ipsilateral findings | Contralateral findings |
|---|---|
| Horner syndrome (ptosis, miosis, hypohidrosis or anhidrosis, enophthalmos, due to damage to descending sympathetic fibers) | Spinothalamic loss (pain/temp) in limbs |
| Cerebellar signs, nystagmus | |
| Cranial nerves IX, X palsy (palatal paralysis, loss of taste posterior 1/3 tongue) | |
| Trigeminal spinothalamic loss in the face |
Investigations
Blood tests:
- FBC
- CRP (potential arteritis)
- U&Es / glucose
- Coagulation profile
- Others as clinically indicated
ECG — assess for atrial fibrillation
CT scan / CT angiogram / CT perfusion scan — per stroke protocols
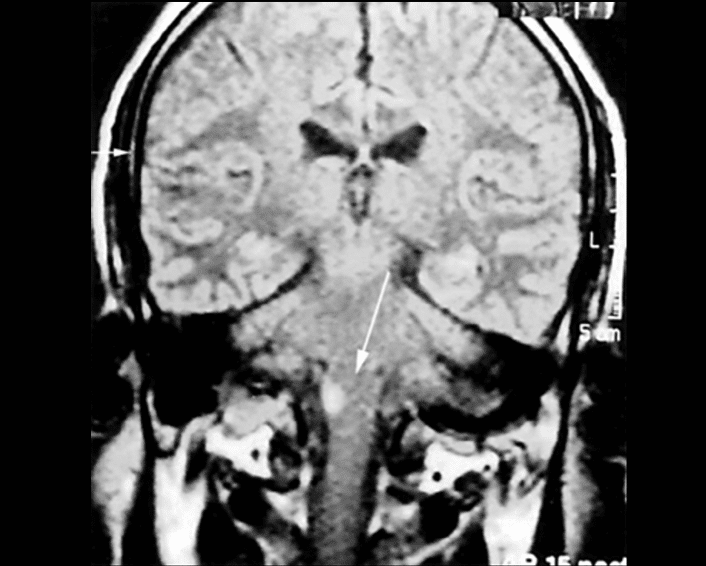
MRI — best imaging for infarct definition. MRI with diffusion‐weighted imaging (DWI) is the best diagnostic test to confirm the infarct in the lateral medulla. The infarcted area has a high DWI signal and a low signal on apparent diffusion coefficient (ADC) mapping images.
Echocardiography and carotid Doppler — if embolic source suspected
Management
- ABC support
- Initiate local CODE STROKE protocols as for any suspected stroke syndrome
- Standard ischaemic stroke protocols should be initiated
- Neurointervention with thrombolysis and/ or endovascular clot retrieval may be appropriate in selected cases for patients who present <24 hours.
- Neurointervention has a high degree of risk within this region. Haemorrhagic complications within the brainstem will carry a significant risk of death
- The risk -versus benefit of this intervention must be carefully assessed by expert neurologist experienced in stroke neurointervention
- Nil orally (in the first instance).
- IV fluids
- Speech therapy referral
- Antiplatelet therapy in those not suitable for neurointervention therapies (e.g., aspirin via NGT if swallowing impaired)
- Speech therapy referral once stable
Prognosis
Prognosis varies based on infarct size and location and timing of intervention.
- Early deaths can result from aspiration or sleep apnoea.
- Many recover significantly over weeks to months.
- Some may have lasting neurological deficits.
Appendix 1
Appendix 1
Appendix 2
Appendix 3
References
Publications
- Kim JS, Lee JH, Suh DC, Lee MC. Spectrum of lateral medullary syndrome. Correlation between clinical findings and magnetic resonance imaging in 33 subjects. Stroke. 1994 Jul;25(7):1405-10.
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Lam Van Le. Lateral medullary syndrome. Radiopaedia
- Easton-Carr R, Lui F, Das JM. Lateral Medullary Syndrome (Wallenberg Syndrome). 2025 Aug 9. In: StatPearls
FOAMed
- Hong L. Wallenberg Syndrome. LITFL
- Cadogan M. Horner Syndrome. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Nickson C. Brainstem lesions. LITFL
- Nickson C. Stroke Thrombolysis. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


