Headache and imaging
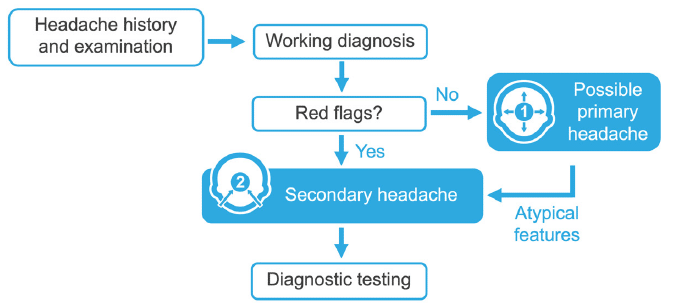
Here is an example algorithm in headache diagnosis
- Take a detailed history and perform a neurologic examination.
- Generate a preliminary diagnosis.
- Analyse for red flags.
- If there are no red flags, consider the criteria for a primary headache disorder
- If there are red flags present or the presentation does not satisfy the criteria for a primary headache, consider a diagnosis of secondary headache.
- Order appropriate diagnostic testing
Most headache patients you will encounter have normal neurological examination and a primary headache disorder. These patients do not need further testing to establish a diagnosis.
However, sometimes there is a pressure for further testing that is created by the expectation of reassurance beyond your word or expertise, as expressed by the patient, family, or your community of colleagues. It is important to avoid unnecessary testing! Therefore, it is important to understand when certain tests are indicated, and when they are not.
When to perform diagnostic imaging
Additional diagnostic evaluation is needed in cases that do not meet the criteria for a primary headache disorder, or which are associated with unusual or worrisome features, such as the red flag symptoms. These are the top ten reasons for ordering diagnostic imaging for your patient with headache:
- Headache characteristics are different from usual.
- Headaches occur with increasing severity or frequency.
- Headache differs from the typical International Headache Society diagnostic criteria for that headache type.
- Abnormality on the neurological examination.
- Patient experiences seizures.
- Headache is sudden or severe (thunderclap headache) or radiates to the neck and you need to rule out subarachnoid haemorrhage.
- Patient is suffering from refractory headaches.
- The headaches always occur ipsilaterally.
- Patient has a co-existing medical condition, such as the human immunodeficiency virus (HIV).
- Patient presents with red flags (remember SNOOPP).
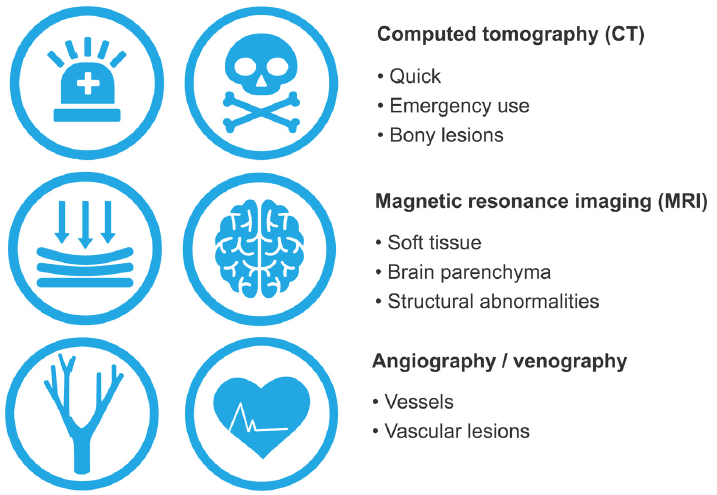
Choice of imaging modality
Computed tomography (CT)
CT is faster, more readily available, and is used often in emergent situations. Emergent imaging, perhaps with a thunderclap headache, trauma, or when determining safety before lumbar puncture can be accomplished with a CT. CT is also superior for assessing bony lesions.
Magnetic resonance imaging (MRI)
MRI is preferred for looking at soft tissue and brain parenchymal structures, and ruling out structural abnormalities. These include tumours, vascular lesions, infections, Arnold-Chiari malformations, pituitary masses, intracranial hypotension, or hydrocephalus.
Angiography / venography
CT / magnetic resonance angiography (MRA) or venography might be needed to further assess vessels and vascular lesions.
When not to order diagnostic imaging for a patient with a headache
While there are no hard and fast rules about when to not image a patient, it is well documented that without focal neurologic examination abnormalities, the yield of imaging decreases.
When a patient has an established headache pattern for years, for instance a typical migraine, and has not had significant changes, they can often be treated without imaging. Many studies have looked for patterns in migraine and tension headache patients using imaging and there are generally no differentiating factors when the neurologic examination is normal.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Donohoe CD. The role of laboratory testing in the evaluation of headache. Med Clin North Am. 2013 Mar;97(2):217-24.
- Lester MS, Liu BP. Imaging in the evaluation of headache. Med Clin North Am. 2013 Mar;97(2):243-65.
- Rizzoli P, Mullally WJ. Headache. Am J Med. 2018 Jan;131(1):17-24.
Neurology Library: Headache – History, Examination and Investigation
- Coni R. Characterising headache. LITFL
- Coni R. Headache history. LITFL
- Coni R. The headache diary. LITFL
- Coni R. Headache triggers. LITFL
- Coni R. Physical examination. LITFL
- Coni R. Neurological examination. LITFL
- Coni R. Headache and imaging. LITFL
- Coni R. Headache and laboratory tests. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


