Tricyclic Overdose
The ECG is a vital tool in the prompt diagnosis of poisoning with sodium-channel blocking medications such as tricyclic antidepressants (TCA), which cause CNS and cardiovascular toxicity in overdose in the form of seizures and ventricular dysrhythmias.
An ECG should be taken in all patients who present with a deliberate self-poisoning (or altered GCS of unknown aetiology) to screen for TCA overdose.
ECG Features of Sodium-Channel Blockade
- Intraventricular conduction delay: QRS > 100 ms in lead II
- Terminal R wave > 3 mm in aVR or R/S ratio > 0.7 in aVR
- Patients with tricyclic overdose will also usually demonstrate sinus tachycardia secondary to muscarinic (M1) receptor blockade
- QT prolongation
The right-sided intraventricular conducting system is more susceptible to the effects of sodium channel blockade — this causes terminal right axis deviation of the QRS complex, which manifests as a dominant R’ wave in aVR.
Sodium Channel Blocking Medications
- Tricyclic antidepressants (= most common)
- Type Ia antiarrhythmics (quinidine, procainamide)
- Type Ic antiarrhythmics (flecainide, encainide)
- Local anaesthetics (bupivacaine, ropivacaine)
- Antimalarials (chloroquine, hydroxychloroquine)
- Dextropropoxyphene
- Propranolol
- Carbamazepine
- Quinine
Clinical Features of Tricyclic Overdose
In overdose, the tricyclics produce rapid onset (within 1-2 hours) of:
- Sedation and coma
- Seizures
- Hypotension
- Tachycardia
- Broad complex dysrhythmias
- Anticholinergic syndrome (tachycardia, mydriasis, dry mouth)
Tricyclics mediate their cardiotoxic effects via blockade of myocardial fast sodium channels (QRS prolongation, tall R wave in aVR), inhibition of potassium channels (QTc prolongation) and direct myocardial depression.
Other toxic effects are produced by blockade at muscarinic (M1), histamine (H1) and α1-adenergic receptors.
The degree of QRS broadening on ECG is correlated with adverse events:
- QRS > 100 ms is predictive of seizures
- QRS > 160 ms is predictive of ventricular arrhythmias (e.g. VT)
Management of Significant Tricyclic Overdose
Overdose >10mg/kg with signs of cardiotoxicity (ECG changes) requires resuscitative management:
- Patients need to be managed in a monitored area equipped for airway management
- Secure IV access, administer high flow oxygen and attach monitoring equipment
- Administer IV sodium bicarbonate. See our antidote post on the correct administration of sodium bicarbonate as excess can cause iatrogenic death.
- Intubate as soon as possible
- Hyperventilate to maintain a pH of 7.50 – 7.55.
- Once the airway is secure, place a nasogastric tube and give 50g (1g/kg) of activated charcoal.
- Treat seizures with IV benzodiazepines (e.g. midazolam 1-2mg)
- Treat hypotension with a crystalloid bolus (10-20 mL/kg). If this is unsuccessful in restoring BP then consider starting vasopressors (e.g. noradrenaline infusion)
- If arrhythmias occur, the first step is to give more sodium bicarbonate. Lidocaine (1.5mg/kg) IV is a third-line agent (after bicarbonate and hyperventilation) once pH is > 7.5
- Avoid Ia (procainamide) and Ic (flecainide) antiarrhythmics, beta-blockers and amiodarone as they may worsen hypotension and conduction abnormalities
- Admit the patient to the intensive care unit for ongoing management
ECG Examples
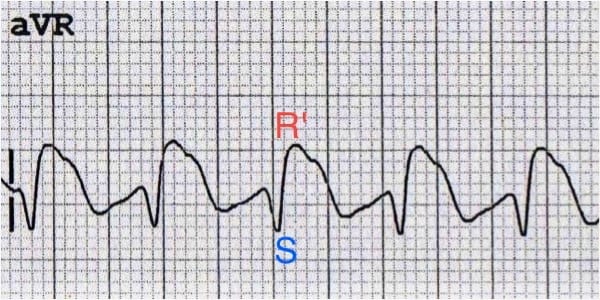
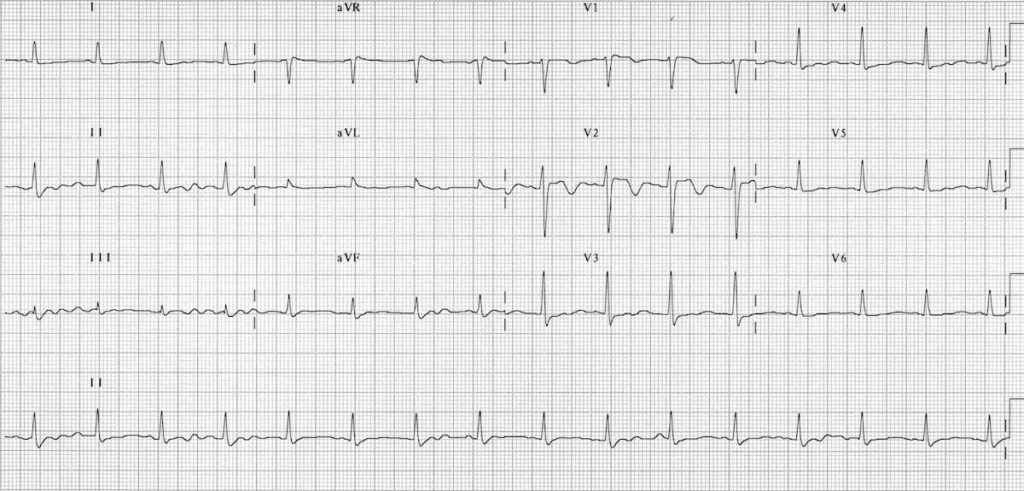
Example 1a
Typical ECG of TCA toxicity demonstrating:
- Sinus tachycardia with first-degree AV block (P waves hidden in the T waves, best seen in V1-2)
- Broad QRS complexes
- Positive R’ wave in aVR
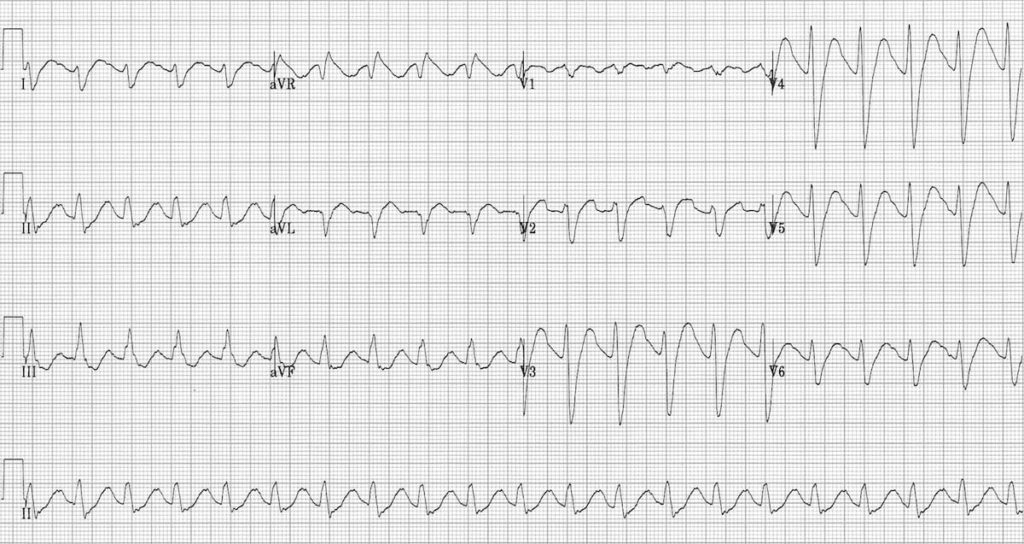
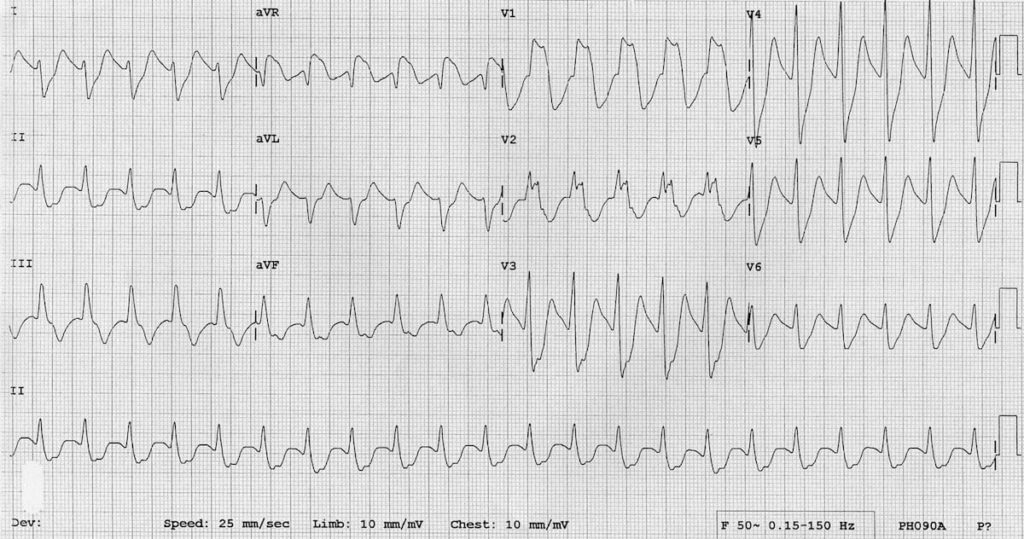
Example 1b
Delayed ECG with worsening TCA toxicity:
A second ECG of the same patient showing worsening TCA cardiotoxicity with marked QRS broadening producing a sine wave appearance reminiscent of hyperkalaemia.
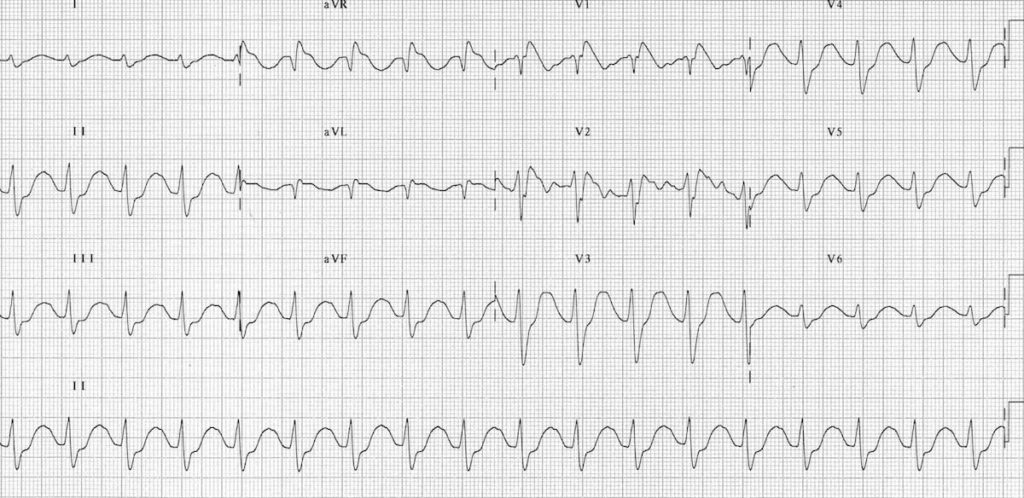
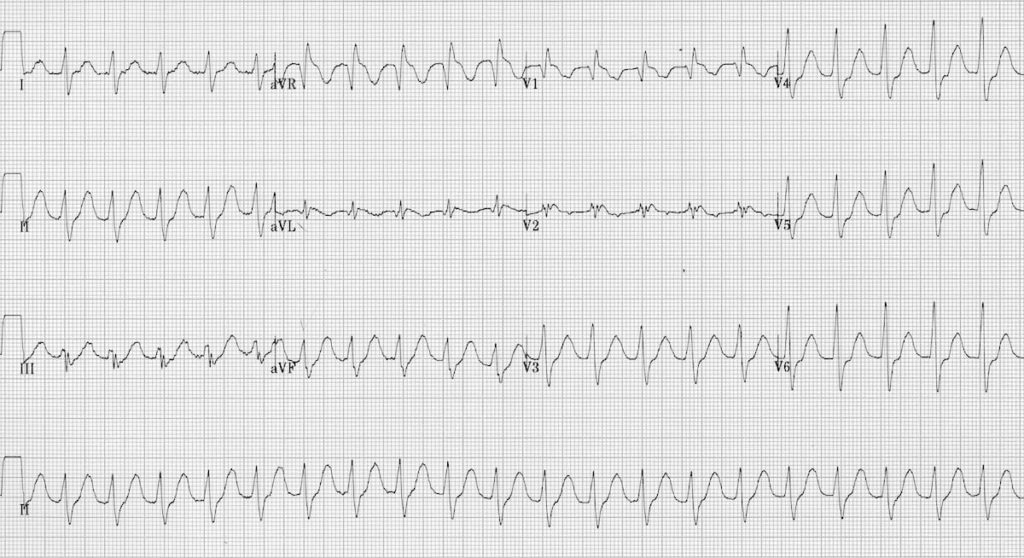
Example 1c
Resolution of TCA toxicity with treatment (bicarbonate and hyperventilation):
- Third ECG of the same patient after serum alkalinisation with sodium bicarbonate, intubation and hyperventilation
- The QRS duration has narrowed back to normal, and the R’ wave in aVR has disappeared
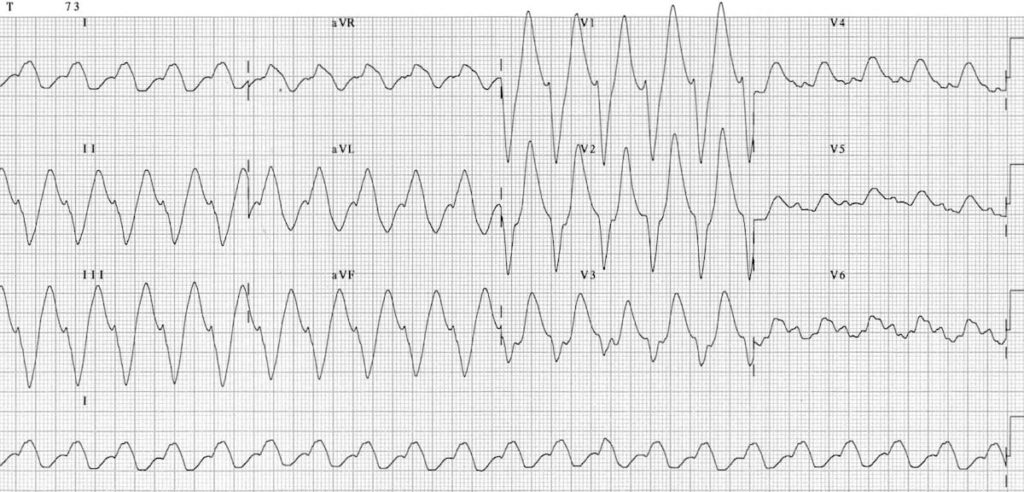
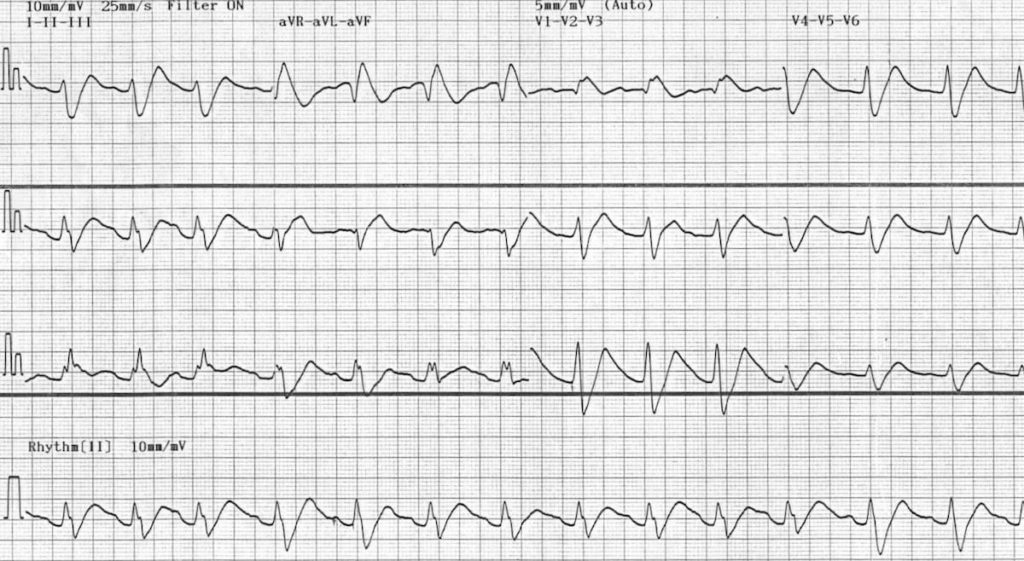
Example 2
Massive TCA overdose
- Another example of severe TCA cardiotoxicity after ingestion of 35 mg/kg doxepin
- There is marked QRS widening with tachycardia and a positive R’ wave in aVR
Example 3
Flecainide overdose:
- Similar ECG changes are seen with other sodium-channel blocking agents
- This ECG demonstrates QRS widening and positive R’ wave in aVR consistent with sodium-channel blockade in a patient with flecainide poisoning
Example 4
Another example of flecainide cardiotoxicity.
Related Topics
- LITFL Tricyclic Antidepressant TCA Overview – TOX Library
- LITFL Toxicology Conundrum 022
- LITFL Toxicology Conundrum 050
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Hi Ed, fellow readers
Great post! Thanks Ed & litfl!
May I ask if there’s a rationale for diazepam over alternatives here?
“Treat seizures with IV benzodiazepines (e.g. diazepam 5-10mg)”
Midaz is more commonly used for seizure termination I’d have thought and my understanding is it had been shown to provide a longer ” seizure free” period vs. diazepam? I know a relatively recent trial showed IV lorazepam was best but I haven’t see this used in Australia.
Just curious if suggesting diaz uses a rationale that the patient is already tubed and on M&M and thus try diazepam if still seizing? Or if they’re on propofol for sedation / regardless of sedation / when seizing occurs you suggest diazepam first line?
Cheers,
Alan