Beta-blocker toxicity
Isolated beta-blocker overdose is usually benign, but there a couple of beta-blockers that cause cardiac instability. Propranolol acts as a sodium channel blocker thereby widening the QRS and deplete the heart of energy source. Sotalol also blocks the metabolic pathways but also causes potassium channel blockade resulting in prolongation of the QT interval and torsades de pointes. And for a little bit of controversy we’ll explain why glucagon is out and high dose insulin is in.
Toxic Mechanism:
As predicted beta-blockers competitively block beta-1 and beta-2 receptors. This results in decreased production of intracellular cyclic adenosine monophosphate (cAMP) with a resultant blunting of multiple metabolic and cardiovascular effects of circulating catecholamines. In therapeutic doses this leads to a reduced heart rate and blood pressure. In overdose this causes the heart to enter a shock state. Utilising glucose instead of fatty acids which produce less ATP, perpetuating the cycle. Propranolol has the added effect of causing sodium channel blockade, widening the QRS and promoting ventricular dysrhythmias and entering the CNS to exert direct toxicity. Sotalol blocked the cardiac potassium channels causing QT prolongation and the risk of torsades de pointes.
Toxicokinetics:
- Rapid absorption
- Peak serum concentration 1 – 3 hours
- Propranolol is extremely lipophilic
- Elimination half lives vary and are extended in overdose. Propanol is normal 12 hours.
Resuscitation:
- CNS depression (even GCS 12) requires prompt intubation and hyperventilation (aiming for pH 7.5-7.55)
- Pre-intubation and on arrival it is vital to get an ECG looking for signs of toxicity (widening of the QRS, large terminal R wave in aVR increased R/S ratio (>0.7) in aVR and QT prolongation). If present give sodium bicarbonate 1-2mmol/kg until effect is seen. Even during the quickest of intubations you will cause a state of acidosis which will exacerbate sodium channel toxicity.
- Ventricular dysrhythmias:
- Sodium bicarbonate 2 mmol/kg IV repeated every 1-2 minutes to restore a perfusing rhythm, multiple doses maybe required.
- It is unlikely that defibrillation will work.
- Lignocaine 1.5 mg/kg IV is third line when the pH is >7.5.
- If requiring the kitchen sink approach some people have used intralipid but this is not standard therapy and expert advice should be sought.
- Type Ia antidysrhythmic agents (e.g. procainamide) and amiodarone are contraindicated
- Hypotension:
- 20ml/kg crystalloid bolus, sodium bicarbonate 2 mmol/kg may restore a MAP >65.
- Failing this adrenaline and noradrenaline infusions can be used (peripherally at first until able to insert a central line when higher doses can be used, of note the risks of extravasation i.e. tissue necrosis is the same as for push dose pressures and using meteraminol/aramine. Make sure you have a big flowing peripheral line).
- Noradrenaline dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min).
- Adrenaline dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min).
- Bradycardia:
- Atropine 0.6 mg (0.02 mg/kg children, up to 0.6 mg) IV bolus and repeat 15 minutely up to 1.8 mg
- Isoprenaline 1 – 10 micrograms/min IV infusion (0.05-1.0 microgram/kg/min in children)
- Adrenaline infusion
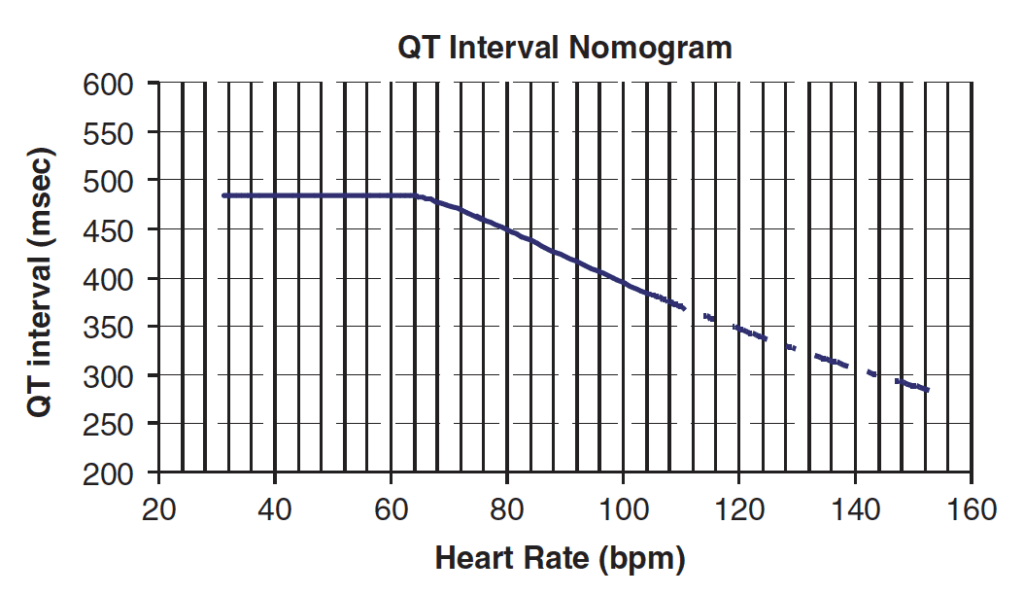
- Torsades de pointes (Sotalol):
- Administer magnesium sulfate 10 mmol (0.05 mmol/kg in children) IV over 15 minutes.
- Correct hypoxia, hypokalaemia and hypocalcaemia
- If heart rate is <100 beats/minute commence an isoprenaline infusion IV at 1-10 microgram/min (0.05-2.0 microgram/kg/min in children) or overdrive pacing to maintain heart rate at 100-120 beats/minute.
Risk Assessment
- Toxicity does not correspond well with ingested dose, but increased risk is associated with:
- Propranolol or Sotalol
- Underlying heart of lung disease
- Co-ingestion with other cardiac depressants or antiarrythmics
- Advanced Age
- Propranolol can cause severe toxicity in doses as low as 1 gram
- Toxicity manifests within 4 hours unless control-released preparations are consumed
- The earliest sign of toxicity is PR-prolongation
- Children: Any ingestion of propranolol or sotalol can be toxic. Ingestion of 1 or 2 tablets of other beta-blockers are benign.
- Clinical effects:
- Cardiovascular (hypotension, bradycardia an bradydysrhythmias, QRS widening with propranolol and QT prolongation with sotalol)
- CNS (Delirium, coma and seizures with propranolol)
- Bronchospasm
- Hyperkalaemia
- Hypo/hyperglycaemia
Supportive Care
- If hypotensive or bradycardic, invasive monitoring and central access maybe required.
- Monitor blood sugar levels and electrolytes
- If intubated see FASTHUGSINBED for further supportive care.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- Serial ECGs and cardiac monitoring for at least 4 hours
- EUC
QT Nomogram
[/DDET]
Decontamination:
- 50g of activated charcoal maybe given to the alert and cooperative patient who present within 2 hours, Caution is advised for those patients who have ingested propanolol due to the high risk of seizures, if they are showing any signs of toxicity charcoal should be avoided until they are intubated.
Enhanced Elimination
- Not clinical useful
Antidote
- High-dose insulin therapy (not truly an antidote in the setting of beta-blocker toxicity – but may be used as an adjunctive inotrope, e.g. in combination with adrenaline).
Why is glucagon out?
- “Nearly all studies examining glucagon in CCB toxicity were conducted prior to the availability of recombinant glucagon and used Eli Lilly’s standard glucagon preparations instead… The standard preparation of glucagon, made from mammalian pancreatic extract, contained insulin (also from pancreatic cells) until recombinant glucagon was available in 1998. Some vials of glucagon, when analyzed by this study group at Carolinas Medical Center, contained 100 units of insulin. This was demonstrated in the study on HIE therapy in verapamil poisoning Kline et al (1995).”
- Thus, there is a possibility that any benefit seen from using these glucagon preparations may have been due to the insulin that was also present.
- See the full story here: glucagon as an antidote
Disposition
- Patients who are asymptomatic and have a normal ECG at 6 hours are medically cleared
- Patients with clinical or ECG manifestations require admission to HDU or ICU.
References and Additional Resources:
Additional Resources:
- CCC – High dose insulin euglycaemic therapy
- CCC – Beta Blocker overdose
- CCC – Sympatholytic toxidrome
- Tox conundrum – Propranolol
- ECG Library – Beta-blocker and Calcium-channel blocker toxicity
Video
Zeff – Cardiac Toxicty aka Master Chef
Sodium channel blockade and the ECG video
References:
- Murray L et al. Toxicology Handbook 3rd Edition. Elsevier Australia 2015. ISBN 9780729542241
- Love J, Howell JM, Litovitz TL, Klein-Schwartz W. Acute beta-blocker overdose: Factors associated with the development of cardiovascular morbidity. Journal of Toxicology Clinical Toxicology 2000; 38:275-281.
- Reith DM, Dawson AH, Epid D et al. Relative toxicity of beta-blockers in overdose. Journal of Toxicology Clinical Toxicology 1996; 34:273-278.
- Taboulet P, Cariou A, Berdeaux A et al. Pathophysiology and management of self-poisoning with beta-blockers. Journal of Toxicology Clinical Toxicology 1993; 31:531-551
Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.
