ECG Case 108
59yr old male who presented to the Emergency Department following 2 episodes of syncope. He had a long history of infrequent unexplained syncope over the prior 15 years.
His only past medical history is diet controlled T2DM and he was taking no regular medications.
ECG on presentation
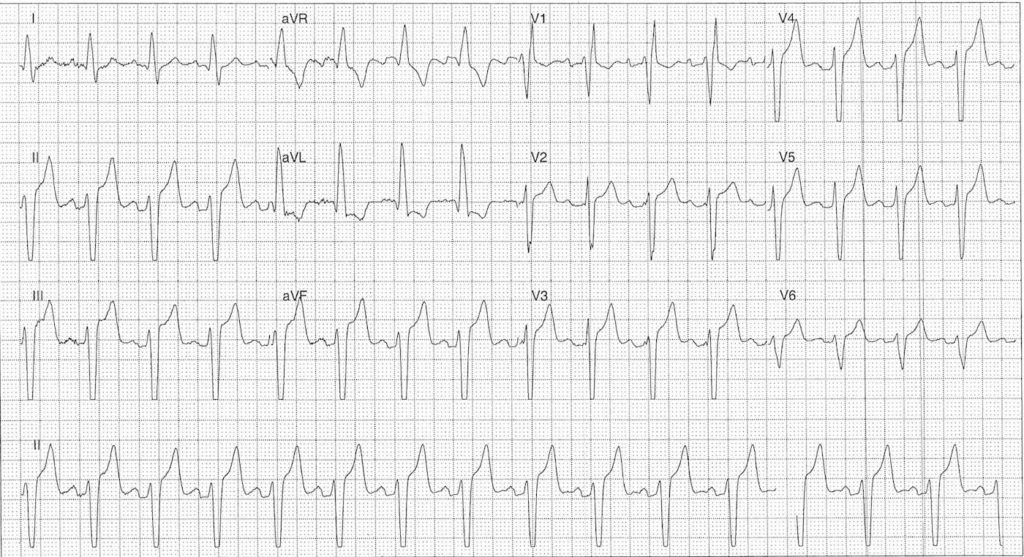
** NOTE this is a non-diagnostic ECG recording as it was generated retrospectively from the rhythm telemetry unit
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
Key features:
- Sinus rhythm rate ~90 bpm
- Left axis deviation
- RBBB Morphology
- Prominent T waves and ST elevation in leads II, III, aVF, V2-5 with high voltage complexes
- This ECG was generated using the monitor (non-diagnostic) algorithm. The filter applied in this mode is 0.5 to 40 Hz which can over- or under-estimate low frequency portions of the ECG including the ST segment.
- The diagnostic algorithm filter performs at 0.05 to 150 Hz.
- For a somewhat complicated overview of ECG filtering check out:
- Borderline 1st degree AV block
Interpretation:
- Bifascicular Block
- Borderline PR prolongation
- Requires cardiology referral for monitoring and consideration of PPM insertion given history of syncope
- ST / T wave changes without chest pain or electrolyte abnormality – related to ECG filtering algorithm
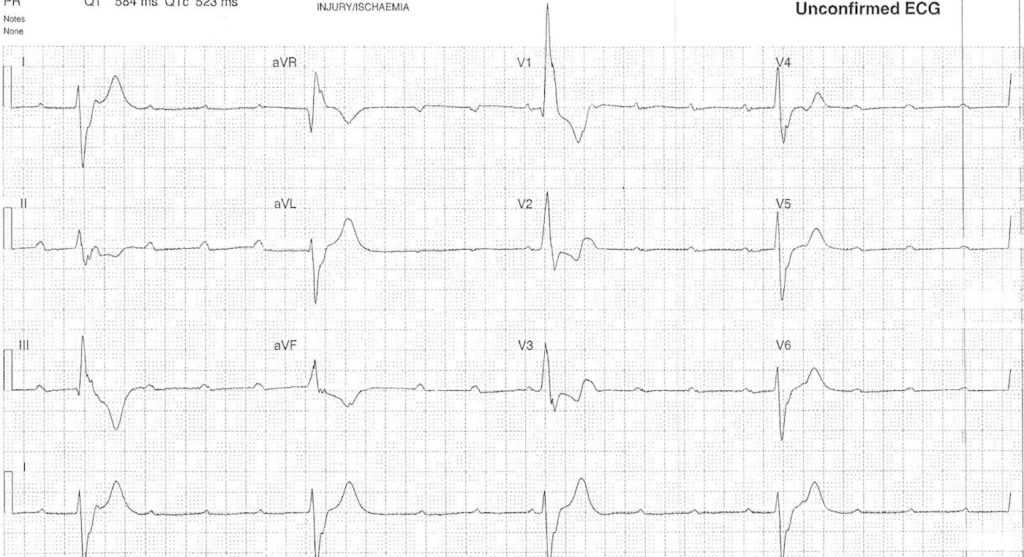
ECG with palpitations
The patient complained of palpitations. Due to rate and rhythm change a rhythm strip was automatically generated
ECG ANSWER and INTERPRETATION
Key features:
- Atrial rate 136 bpm
- Ventricular rate 27 bpm
- AV Dissociation
- Broad Complex QRS
Impression:
- Complete heart block
- Ventricular escape rhythm
Interpretation:
- Compared with rhythm strip above
- Complete heart block
- AV Dissociate with ventricular escape rhythm, rate 24 bpm
- Slowing of atrial rate now ~115 bpm
CLINICAL OUTCOME
What happened next?
The patient was treated with atropine followed by isoprenaline infusion.
The next day he underwent an uneventful dual chamber PPM insertion. A subsequent echo showed was normal with an ejection fraction of 64%.
On review of his medical records prior ECG’s had shown alternating left and right bundle branch blocks confirming progressive conducting system disease.
Further reading:
- ECG Library – Complete heart block
- ECG Library – Right bundle branch block
- ECG Library – Anterior / Posterior left fascicular block
- ECG Library – Trifascicular block
TOP 150 ECG Series
Emergency Medicine Specialist MBChB FRCEM FACEM. Medical Education, Cardiology and Web Based Resources | @jjlarkin78 | LinkedIn |


Dear G’ time
The 2nd ECG shows atrial to ventricular complexes 4 to 1 in a regular fashion which it can be seen in atrial tachycardia while in complete Av block not ? Best regards
Dr. Mortadha Saadedden Phd
The second ECG shows 4:1 conduction block— ventr rate is around 25 and constant PR interval ( arnd 0.4 s)— s this should be a case of Type 2 Mobitz block and not 3 rd degree AV block
Do you know if in this case, did the atropine help the patient? If they are in CHB would atropine work? Or is it being paired with isoprenaline create a more desired effect?