Trifascicular Block
Diagnostic criteria
True trifascicular block refers to the presence of conduction delay in all three fascicles below the AV node (RBBB, LAFB, LPFB), manifesting as bifascicular block and 3rd degree AV block. One of two ECG patterns is present:
- 3rd degree AV block + RBBB + LAFB or;
- 3rd degree AV block + RBBB + LPFB
The ventricular escape rhythm usually arises from the region of either the left anterior or left posterior fascicle (distal to the site of block), producing QRS complexes with the appearance of RBBB plus either LPFB or LAFB respectively.
Impending trifascicular block
Other rare indicators of trifascicular block include:
- Normal sinus rhythm with alternating LBBB/RBBB
- RBBB with alternating fascicular blocks on a beat-to-beat basis
These herald impending failure of all three fascicles and associated 3rd degree AV block.
A clinical misnomer
The term “trifascicular block” is most commonly used clinically to describe bifascicular block associated with 1st degree AV block or 2nd degree AV block.
- This term is inaccurate, as the conduction delay resulting in PR interval prolongation usually occurs in the AV node, not in the third remaining fascicle
- There is no difference in progression to complete heart block in patients with bifascicular block versus those with bifascicular block and associated 1st degree AV block or 2nd degree Mobitz I block (1% risk per year)
- The American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society (AHA/ACCF/HRS) recommends against the use of the term “trifascicular block”, as it does not have a unique anatomical association and does not accurately reflect the underlying anatomical disease process
Clinical Implications
- Patients with true trifascicular block (associated third degree AV block) will require pacemaker insertion
- Patients with bifascicular block and syncope or presyncope should be admitted for monitoring and likely pacemaker insertion (class II)
- Asymptomatic bifascicular block with first degree AV block is not an indication for pacing (class III)
Main Causes
Causes are similiar to those of bifascicular block, related to degeneration or conduction impairment in fascicles below the AV node:
- Ischaemic heart disease (40-60%)
- Structural heart disease (50-80% association)
- Aortic stenosis
- Anterior MI
- Lenègre-Lev disease
- Congenital heart disease
- Hyperkalaemia (resolves with treatment)
- Digoxin toxicity
ECG Examples
Example 1
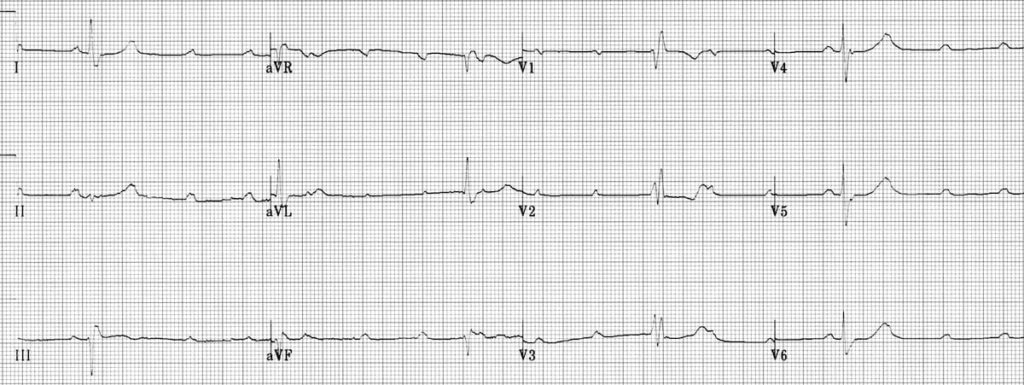
True Trifascicular Block:
- Right bundle branch block
- Left axis deviation (Left anterior fascicular block)
- Third degree heart block
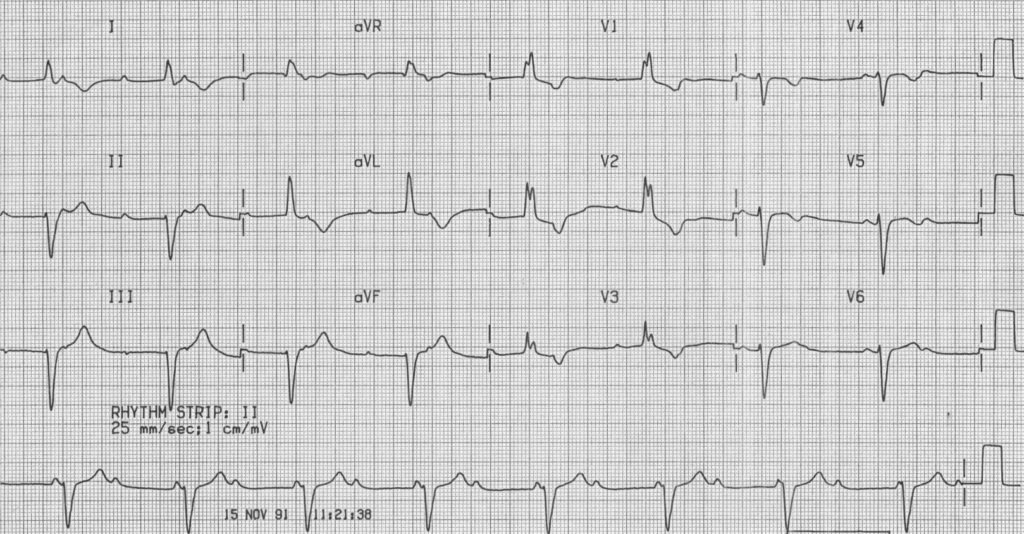
Example 2
Example 3 (previously termed “incomplete trifascicular block”)
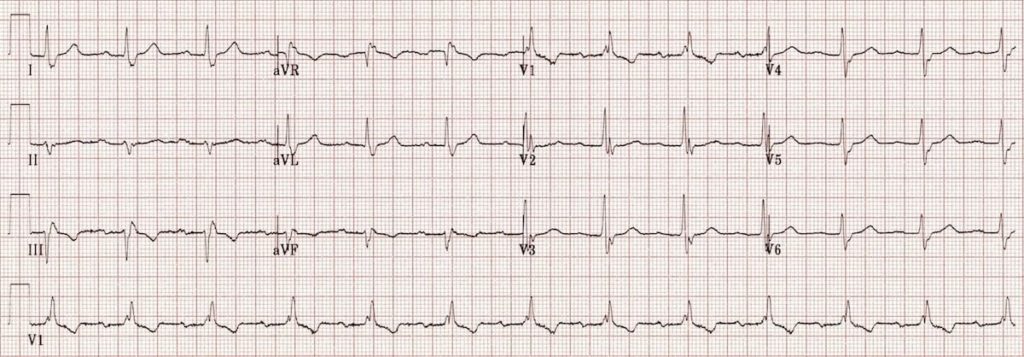
Bifascicular block + first degree AV block
- Right bundle branch block
- Left axis deviation (= left anterior fascicular block)
- First degree AV block
Commonly referred to clinically as “incomplete trifascicular block”, this represents conducting disease of two fascicles, with delayed conduction through either the AV node or the remaining third fascicle. It is not possible to differentiate between the two based on the ECG alone
Clinical Cases
- Top 100 ECG – Case 094
Related Topics
- Left bundle branch block LBBB
- Right Bundle Branch Block RBBB
- Left anterior fascicular block LAFB
- Left posterior fascicular block LPFB
- Interventricular Conduction Delay IVCD
- Bifascicular block
- AV block: 1st degree
- Complete Heart block CHB
Further reading
References
- AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):976-81.
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Emergency Medicine Specialist MBChB FRCEM FACEM. Medical Education, Cardiology and Web Based Resources | @jjlarkin78 | LinkedIn |


Braunwald’s Text book of Cardiology states:
“Bidivisional block in the presence of prolongation of the PR interval (first degree AV block) may indicate disease of the third subdivision rather than disease of the AV node and is associated with a greater risk of complete heart block than if first degree AV block is absent”
Hi Rehman
It is not possible to determine whether the conduction delay resulting in PR interval prolongation is occurring in the AV node or in the third remaining fascicle. Despite this, there is no difference in progression to complete heart block, or in incidence of symptomatic bradyarrhythmias, in patients with bifascicular block versus those with bifascicular block and associated 1st degree AV block (1% risk per year)