ECG changes in Pulmonary Embolism
The ECG changes associated with acute pulmonary embolism may be seen in any condition that causes acute pulmonary hypertension, including hypoxia causing pulmonary hypoxic vasoconstriction.
ECG Features:
- Sinus tachycardia – the most common abnormality (seen in 44% of patients with PE)
- Complete or incomplete RBBB (18%)
- Right ventricular strain pattern – T wave inversions in the right precordial leads (V1-4) ± the inferior leads (II, III, aVF). This pattern is associated with high pulmonary artery pressures (34%)
- Right axis deviation (16%). Extreme right axis deviation may occur, with axis between zero and -90 degrees, giving the appearance of left axis deviation (“pseudo left axis”)
- Dominant R wave in V1 – a manifestation of acute right ventricular dilatation
- Right atrial enlargement (P pulmonale) – peaked P wave in lead II > 2.5 mm in height (9%)
- SI QIII TIII pattern – deep S wave in lead I, Q wave in III, inverted T wave in III (20%). This “classic” finding is neither sensitive nor specific for PE
- Clockwise rotation – shift of the R/S transition point towards V6 with a persistent S wave in V6 (“pulmonary disease pattern”), implying rotation of the heart due to right ventricular dilatation
- Atrial tachyarrhythmias – AF, flutter, atrial tachycardia (8%)
- Non-specific ST segment and T wave changes, including ST elevation and depression (50%)
Simultaneous T wave inversions in the inferior (II, III, aVF) and right precordial leads (V1-4) is the most specific finding in favour of PE, with reported specificities of up to 99% in one study.
ECG findings compared to Acute Coronary Syndrome
T-wave inversion is commonly associated with acute coronary syndrome (ACS). Both ACS and PE can present with elevated troponin, but several findings can assist in differentiating between the two:
- ACS is rarely associated with tachycardia
- Bedside echo may be useful in differentiating the two, demonstrating features of RV dilatation and pulmonary arterial hypertension
- Kosuge et al have shown that simultaneous inversion in III and V1 are diagnostically significant:
Negative T waves in leads III and V1 were observed in only 1% of patients with ACS compared with 88% of patients with Acute PE (p less than 0.001). The sensitivity, specificity, positive predictive value, and negative predictive value of this finding for the diagnosis of PE were 88%, 99%, 97%, and 95%, respectively. In conclusion, the presence of negative T waves in both leads III and V1 allows PE to be differentiated simply but accurately from ACS in patients with negative T waves in the precordial leads.
Kosuge et al 2007
Pathophysiology
ECG changes in PE are related to:
- Dilation of the right atrium and right ventricle with consequent shift in the position of the heart
- Right ventricular ischaemia
- Increased stimulation of the sympathetic nervous system due to pain, anxiety and hypoxia
Clinical Usefulness
- The ECG is neither sensitive nor specific enough to diagnose or exclude PE
- Around 18% of patients with PE will have a completely normal ECG.
- However, with a compatible clinical picture (sudden onset pleuritic chest pain, hypoxia), an ECG showing new RAD, RBBB or T-wave inversions may raise the suspicion of PE and prompt further diagnostic testing
- In patients with radiologically confirmed PE, there is evidence to suggest that ECG changes of right heart strain and RBBB are predictive of more severe pulmonary hypertension; while the resolution of anterior T-wave inversion has been identified as a possible marker of pulmonary reperfusion following thrombolysis
Differential Diagnosis
The ECG changes described above are not unique to PE. A similar spectrum of ECG changes may be seen with any cause of acute or chronic cor pulmonale (i.e. any disease that causes right ventricular strain / hypertrophy due to hypoxic pulmonary vasoconstriction).
Acute cor pulmonale:
- Severe pneumonia
- Exacerbation of COPD / asthma
- Pneumothorax
- Recent pneumonectomy
- Upper airway obstruction
Chronic cor pulmonale:
- Chronic obstructive pulmonary disease
- Recurrent small PEs
- Cystic fibrosis
- Interstitial lung disease
- Severe kyphoscoliosis
- Obstructive sleep apnoea
ECG Examples
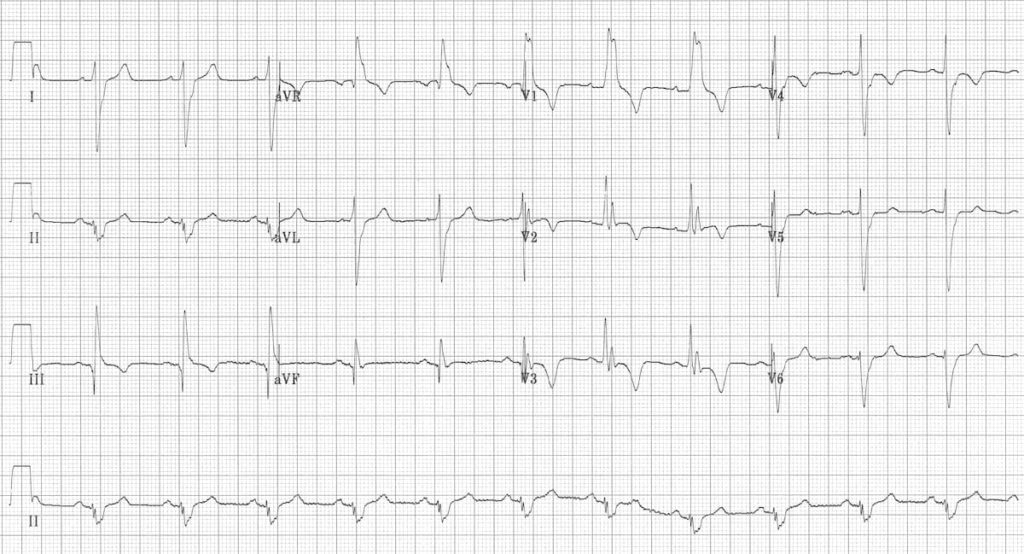
Example 1

Massive bilateral pulmonary embolus
- Sinus tachycardia
- RBBB
- T-wave inversions in the right precordial leads (V1-3) as well as lead III
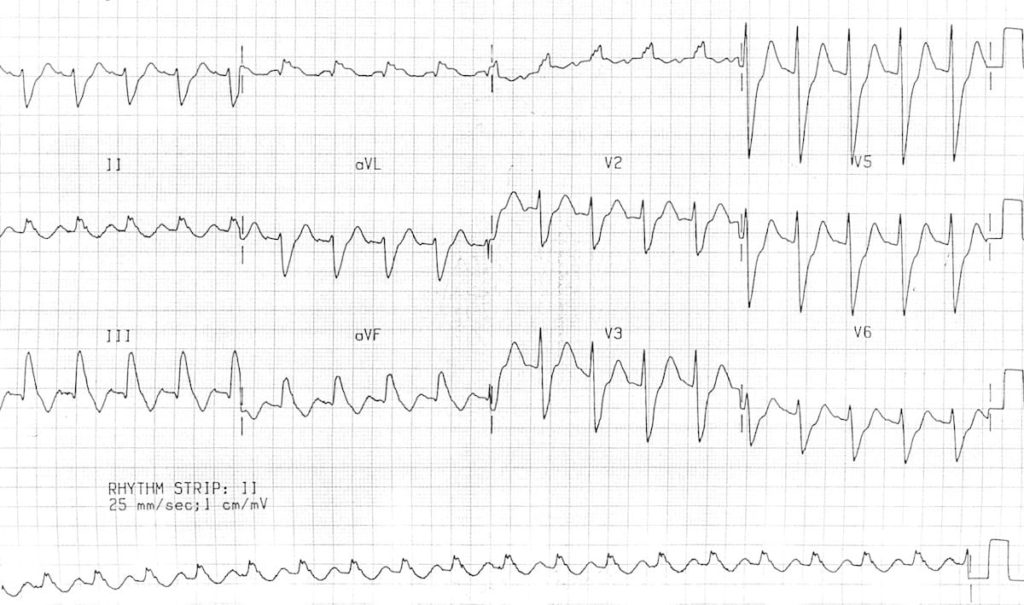
Example 2
Massive bilateral pulmonary embolus
- RBBB
- Extreme right axis deviation (+180 degrees)
- S1 Q3 T3
- T-wave inversions in V1-4 and lead III
- Clockwise rotation with persistent S wave in V6
Example 3

Massive pulmonary embolus
- Sinus tachycardia.
- Simultaneous T-wave inversions in the anterior (V1-4) and inferior leads (II, III, aVF).
- Non-specific ST changes – slight ST elevation in III and aVF.
Example 4

This patient has bilateral PEs confirmed on CTPA.
- Sinus tachycardia.
- Terminal T-wave inversion in V1-3 (this morphology is commonly seen in PE). There is also T-wave inversion in lead III.
Example 5

- Right axis deviation.
- T-wave inversions in V1-4 (extending to V5).
- Clockwise rotation with persistent S wave in V6.
Note: This patient had confirmed pulmonary hypertension on echocardiography with dilation of the RA and RV.
Example 6

- Sinus tachycardia.
- RBBB.
- Simultaneous T-wave inversions in precordial leads V1-3 plus inferior leads III and aVF.
Example 7
Saddle embolus confirmed on CTPA
- Sinus tachycardia.
- Right axis deviation.
- Marked interventricular conduction delay – most likely RBBB given the RSR’ pattern in V1
- Persistent S waves in V6.
Related Topics
- Right atrial enlargement
- Right axis deviation
- Right bundle branch block
- Right ventricular hypertrophy
- Right ventricular strain
- “An Electrocardiographic Exigency” — a case of fatal PE
Literature
- Ferrari E, Imbert A, Chevalier T, Mihoubi A, Morand P, Baudouy M. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads–80 case reports. Chest. 1997 Mar;111(3):537-43
- Rodger M, Makropoulos D, Turek M, Quevillon J, Raymond F, Rasuli P, Wells PS. Diagnostic value of the electrocardiogram in suspected pulmonary embolism. Am J Cardiol. 2000 Oct 1;86(7):807-9
- Ullman E, Brady WJ, Perron AD, Chan T, Mattu A. Electrocardiographic manifestations of pulmonary embolism. Am J Emerg Med. 2001 Oct;19(6):514-9
- Kosuge M, Kimura K, Ishikawa T, Ebina T, Hibi K, Kusama I, Nakachi T, Endo M, Komura N, Umemura S. Electrocardiographic differentiation between acute pulmonary embolism and acute coronary syndromes on the basis of negative T waves. Am J Cardiol. 2007 Mar 15;99(6):817-21
- Co I, Eilbert W, Chiganos T. New Electrocardiographic Changes in Patients Diagnosed with Pulmonary Embolism. J Emerg Med. 2017 Mar;52(3):280-285
Learn from the experts
- ECG Top 100 – Case 104
- Pulmonary Embolus pondering
- CCC – Pulmonary Embolism
- Dr Smith’s ECG Blog: Pulmonary embolism cases
- PulmCrit: Two EKG patterns of pulmonary embolism which mimic MI
- Bhamidipati A. Pulmonary embolism: Why do we miss it, and how do we get better? emDocs 2021
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Hi Dr. Burns, can you list the studies that you use for the above percentages / findings? Thanks!
Ferrari E, Imbert A, Chevalier T, Mihoubi A, Morand P, Baudouy M. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads–80 case reports. Chest. 1997 Mar;111(3):537-43
Ullman E, Brady WJ, Perron AD, Chan T, Mattu A. Electrocardiographic manifestations of pulmonary embolism. Am J Emerg Med. 2001 Oct;19(6):514-9
Kosuge M, Kimura K, Ishikawa T, Ebina T, Hibi K, Kusama I, Nakachi T, Endo M, Komura N, Umemura S. Electrocardiographic differentiation between acute pulmonary embolism and acute coronary syndromes on the basis of negative T waves. Am J Cardiol. 2007 Mar 15;99(6):817-21
I need that data too. I can’t find it in any journal. thank you.