Eponymous Triads
Medical triads, tetrads, and pentads are shorthand diagnostic groupings which combine sets of three, four, or five characteristic clinical features. These clusters of signs, symptoms, or pathological findings serve as memorable patterns that help recognise, recall, and communicate specific conditions.
In medicine, a triad is a set of three clinical features that, when found together, strongly suggest a diagnosis; tetrad and pentad extend the idea to four and five linked features. These are teaching tools and memory aids rather than proofs. They can useful in pattern recognition, but are also historically slippery with credit rarely applied to the true originator, and many variants abound.
Etymology: triad from Greek triás (τριάς, “group of three”), tetrad from tetrás (τετράς), pentad from pentás (πεντάς).
TRIADS
Amyand’s triad
- Amyand’s hernia
- Appendicitis
- Undescended testis
Coined by Dhanasekarapandian et al in 2018 who published the case of a 35-day-old infant with an irreducible right inguinal hernia, inflamed appendix, and gangrenous undescended testis managed by appendicectomy, orchidectomy, and herniotomy.
- Claudius Amyand (c.1680-1740) was an French-born English surgeon
- Dhanasekarapandian V, Shanmugam V, Jagannathan M. Amyand’s Hernia, Appendicitis, and Undescended Testis: The Amyand’s Triad. J Indian Assoc Pediatr Surg. 2018 Jul-Sep;23(3):169-170.
Beck’s triad (1) acute cardiac compression triad
- Hypotension: Low blood pressure due to reduced cardiac output.
- Jugular Venous Distension (JVD): Bulging neck veins caused by backpressure because the heart cannot accept venous return.
- Muffled/Distant Heart Sounds: Sounds are dampened by fluid, blood, or air in the pericardial sa
In 1935, Claude Schaeffer Beck (1894-1971) described the cardiac compression triad of acute cardiac tamponade which consisted of:
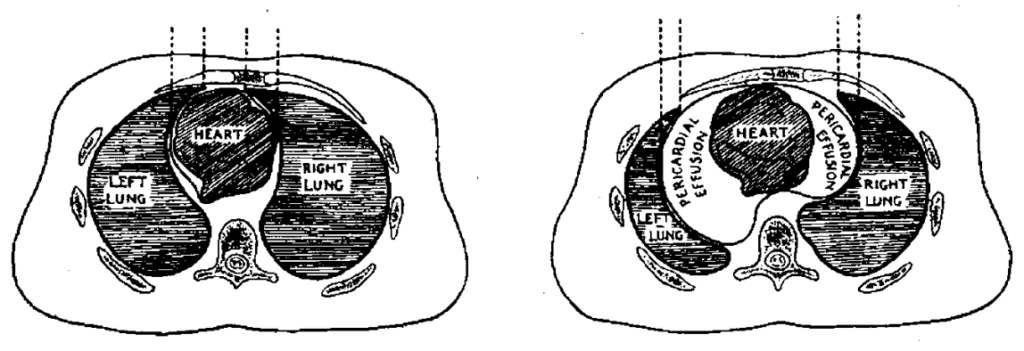
1) A falling arterial pressure, 2) a rising venous pressure and 3) a small, quiet heart. All other clinical manifestations of acute compression are secondary to this triad. The great venous gateway to the heart (the intrapericardial segments of the venae cavae and the right auricle) is partially or completely collapsed. The ventricles are also smaller than normal.
Beck 1935
Beck’s triad (2) chronic cardiac compression triad
In the same paper of 1935, Beck outlined the clinical picture of the chronic cardiac tamponade.
The chronic cardiac compression triad consists of 1) a high venous pressure, 2) ascites and 3) a small quiet heart. All other clinical manifestations of chronic compressions are secondary to this triad.
Beck 1935
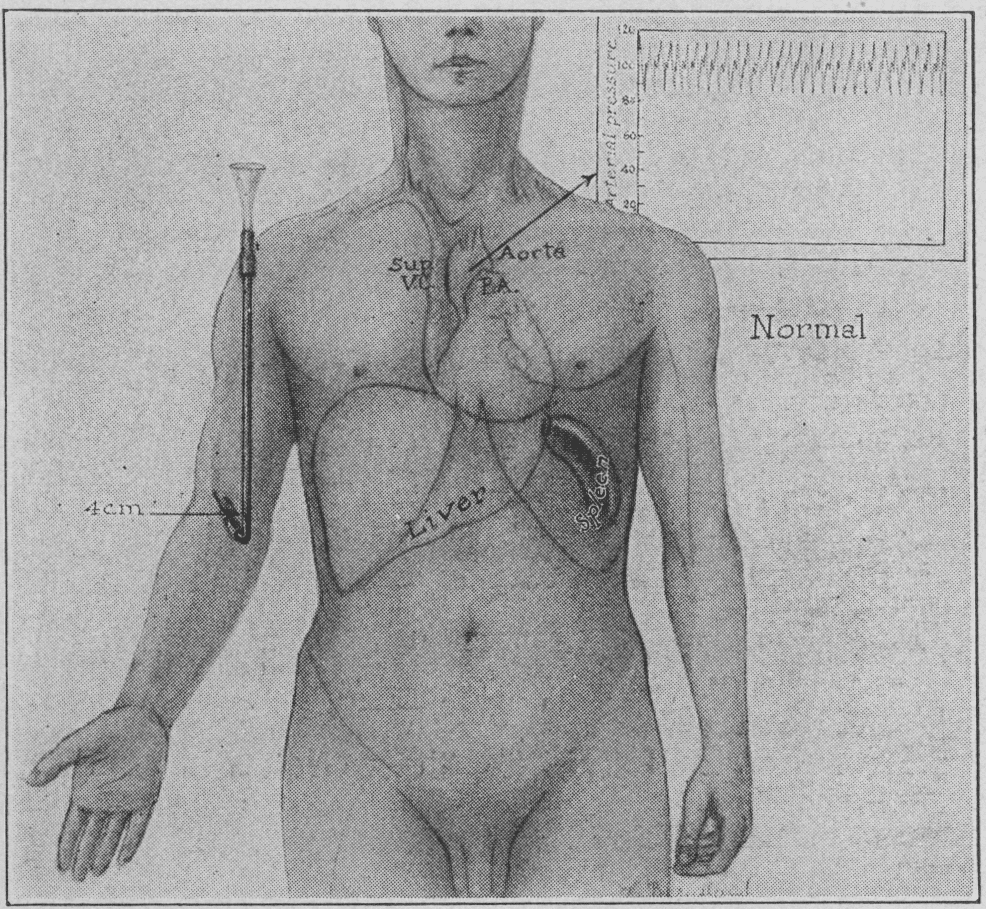

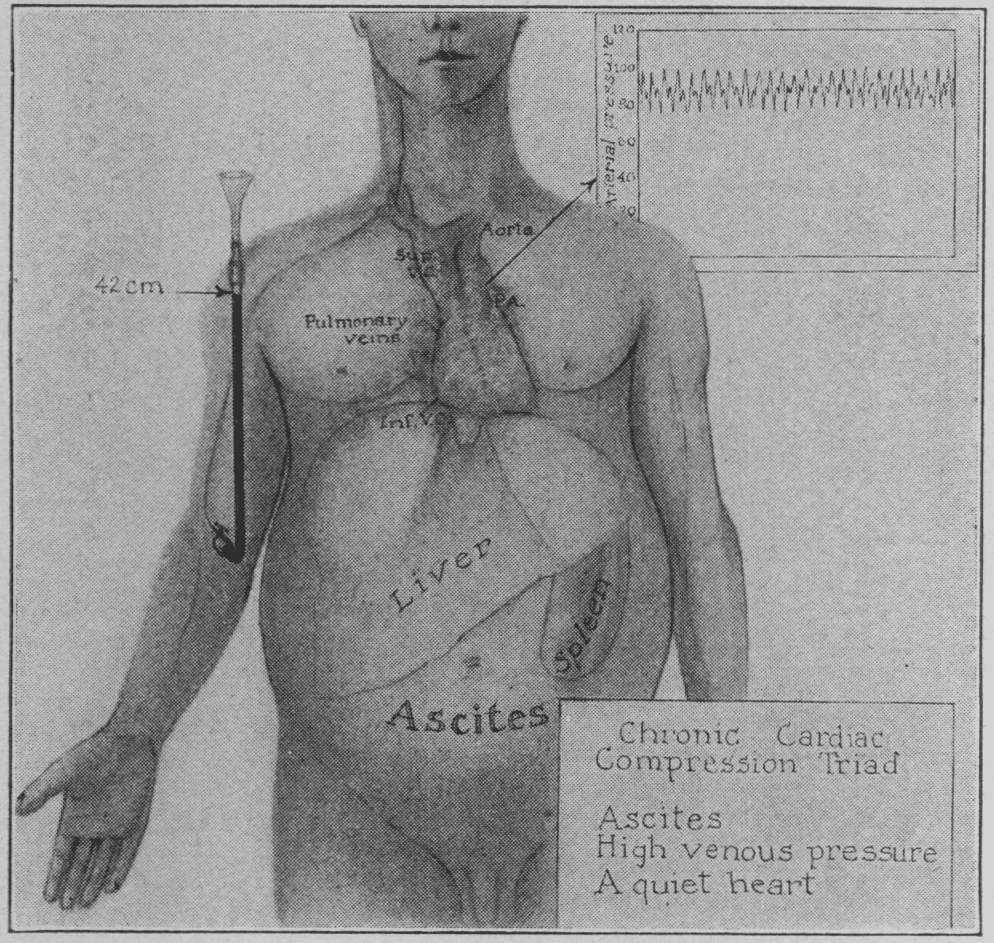
For comparison, normal (fig. 1), acute (fig. 2) and chronic (fig. 3): The acute compression is produced by fluid in the pericardial cavity. Note collapse of venous gateway and distention of veins outside the pericardium. The ventricles are shrunken and the heart per se is smaller than normal. The parietal pericardium has not had time to dilate, nor has there been sufficient time for the liver to enlarge and for ascites to form. In the illustration for chronic compression of the heart the compression is produced by scar tissue. The heart is a small shrunken organ in contradistinction to cardiac dilatation. The veins dilate in response to the high venous pressure. The liver and spleen enlarge and ascites develops. [Beck 1935]
- Claude Schaeffer Beck (1894-1971) was an American Cardiac Surgeon
- Beck CS. Two cardiac compression triads. JAMA. 1935; 104(9): 714-716
Charcot’s Triad
Dieulafoy’s Triad (Appendicitis) [Triade de Dieulafoy]
Triad of physical findings indicating acute appendicitis outlined by Dieulafoy to differentiate appendicitis from intestinal lithiasis and other causes of abdominal pain.
- Tenderness at McBurney’s point (douleur au point de Mac-Burney)
- Cutaneous hyperaesthesia (hyperesthésie cutanée)
- Involuntary muscular guarding (défense musculaire)
Au cas d’appendicite, le territoire abdominal cutané, qui correspond à la zone douloureuse sous-jacente, est le siège d’une hyperesthésie caractéristique et le plan musculaire abdominal est tendu, douloureux, contracturé au point de Mac-Burney…c’est à cette région que se localisent l’hyperesthésie cutanée et la défense musculaire, qui sont des éléments précieux de diagnostic.- Dieulafoy 1898
In cases of appendicitis, the abdominal cutaneous area, which corresponds to the underlying painful area, is the site of characteristic hyperaesthesia, and the abdominal muscles are tense, painful, and contracted at the MacBurney point…it is in this region that cutaneous hyperaesthesia and muscular guarding are located, which are valuable diagnostic elements. – Dieulafoy 1898
- Georges-Paul Dieulafoy (1839-1911) was a French Clinician
- Dieulafoy G. Lithiase intestinale et entéro-colite. Clinique médicale de l’Hôtel-Dieu de Paris, 1898: I: 296 [trois signes caractéristiques de l’appendicite]
Dieulafoy’s Triad (functional blindness)
Triad suggestive of functional/hysterical blindness described by Dieulafoy in his clinical lectures at Hôtel-Dieu de Paris.
- Sudden onset of blindness (cécité à début brusque)
- Preserved pupillary light reflexes (conservation des réflexes pupillaires)
- Normal fundoscopic exam (intégrité du fond de l’œil)
Cécité complète à début brusque, conservation du réflexe pupillaire à la lumière et intégrité du fond de l’œil… ces constatations répondaient au syndrome que je désigne du nom de ‘triade symptomatique de la cécité hystérique.’ – Dieulafoy 1904
Complete blindness with sudden onset, preservation of the pupillary light reflex, and integrity of the fundus… these findings corresponded to the syndrome that I call the ‘symptomatic triad of hysterical blindness.’ – Dieulafoy 1904
Confirmed and cited by Crouzon (1915) in wartime neuropsychiatric observations of sudden blindness without organic findings. Multiple cases published e.g. cécité temporaire provoquée par l’éclatement d’obus à proximité
- Georges-Paul Dieulafoy (1839-1911) was a French Clinician
- Dieulafoy G. Deux case de cécité hystérique. Clinique Médicale de l’Hôtel-Dieu de Paris, 1904; V: 75 [triade symptomatique de la cécité hystérique]
Horner syndrome (1869)
Horner syndrome, also known as oculosympathetic paresis, is a neurological disorder caused by disruption of the sympathetic pathway from the hypothalamus to the eye and face. It manifests with a classic triad of
- Ptosis: Drooping of the upper eyelid due to paralysis of the superior tarsal muscle
- Miosis: Constricted pupil due to loss of sympathetic innervation to the dilator pupillae muscle
- Anhidrosis: Absence of sweating on the affected side of the face
Horner first described the condition clinically in 1869, expanding on earlier experimental work by Claude Bernard (1813-1878). His description helped localize the lesion within the sympathetic chain and distinguish central from peripheral lesions.
1869 – Horner reported the findings of ptosis, miosis, enophthalmos in a 40-year-old peasant woman in Über eine Form von Ptosis. He also observed increased skin temperature and dryness of the ipsilateral face.
- Johann Friedrich Horner (1831-1886) was a Swiss ophthalmologist
- Horner F. Über eine Form von Ptosis. Klinische Monatsblätter für Augenheilkunde 1869;7:193-198
Hutchinson triad (1858)
- Hutchinson teeth (notched central incisors and peg-like lateral incisors),
- Interstitial keratosis,
- Sensorineural deafness (due to lesions of the 8th cranial nerve)
Hutchinson triad of congenital syphilis typically appears after 2 years of age as part of late congenital syphilis.
- Sir Jonathan Hutchinson (1828-1913) was an English surgeon, dermatologist, ophthalmologist, pathologist and venereologist…
- Hutchinson J. Report on the effects of infantile syphilis in marring the development of the teeth. Transactions of the Pathological Society of London, 1858; 9: 449-456. [Hutchinson teeth]
- Hutchinson J. A clinical memoir on certain diseases of the eye and ear, consequent on inherited syphilis. 1863
Kartagener triad (1933)
- Situs Inversus
- Bronchiectasis
- Chronic Sinusitis
Kartagener syndrome (KS) is an inherited disorder (autosomal recessive) and is is a subset of primary ciliary dyskinesia with abnormal ciliary structure/function associated with impaired ciliary motility
- Manes Kartagener (1897-1975) was an Austrian-Swiss physician
- Kartagener M. Zur Pathogenese der Bronchiektasien. I. Mitteilung: Bronchiektasien bei Situs viscerum inversus. Beiträge zur Klinik der Tuberkulose. 1933;83(4):489–501
Mackler’s triad (1952)
Mackler described the three characteristic features of oesophageal rupture and an indication for left thoracotomy:
- Vomiting,
- Lower thoracic pain (T10)
- Subcutaneous cervical emphysema
Mackler pointed out the difference between rupture and perforation. Rupture is a spontaneous cause or due to indirect trauma likely related to increase intra-abdominal pressure. Mackler supported this with the histopathology of oesophageal ruptures.
- Saul Allen Mackler (1913-2007) was an American thoracic Surgeon
- Mackler SA. Spontaneous rupture of the esophagus. An experimental and clinical study. Surgery, Gynecology & Obstetrics 1952; 95: 345-356.
Meigs Triad (1934)
Triad of ascites with hydrothorax in association with benign ovarian tumour, that is cured after tumour resection.
- Ascites
- Pleural effusion (hydrothorax)
- Benign ovarian fibroma (or fibroma-like tumour)
1934 – In his book Tumors of the Female Pelvic Organ Meigs noted a recurrent pattern of fluid accumulation in association with benign ovarian fibromas.
1937 – Meigs and John W. Cass published a more detailed clinical series in American Journal of Obstetrics and Gynecology, reporting seven cases of ovarian fibromas accompanied by ascites and hydrothorax. This was the first formal articulation of the syndrome as a distinct clinical entity.
A pelvic tumor, ascites, and hydrothorax occurred together in all seven cases…In each case the operative removal of the ovarian fibroma was followed by prompt and complete disappearance of both the abdominal and the thoracic fluids.
Meigs, Cass 1937
Both fluid accumulations resolve spontaneously after tumour removal. It is a diagnosis of exclusion, requiring histological confirmation of a benign tumour and elimination of metastatic disease.
- Joe Vincent Meigs (1892-1963) was an American obstetrician and gynecologist
- Meigs JV. Tumors of the Female Pelvic Organs. New York, NY. 1934: 262–3.
- Meigs JV, Cass JW Fibroma of the ovary with ascites and hydrothorax, with a report of seven cases. American Journal of Obstetrics and Gynecology 1937; 33: 249-267.
Merseburger Triad (1840)
- Exophthalmos
- Goitre
- Tachycardia/Palpitations
Karl Adolph von Basedow who proposed the name Die Glotzaugen-cachexie [Goggle-eyed cachexia] in 1840. Known more commonly as the Merseburger Triad, named after the small German town where Basedow practiced. In 1858 Georg Hirsch (1858) proposed the eponymous name Basedow disease.
- Karl Adolph von Basedow (1799-1854) was a German general practitioner, surgeon and obstetrician
- Basedow KA. Exophthalmos durch Hypertrophie des Zellgewebes in der Augenhöhle. Wochenschrift für die gesammte Heilkunde. 1840; 13: 197-204
Moschcowitz triad (pericardial effusion)
In 1933 Moschcowitz published A new sign of pericardial effusion, in which he described three physical examination findings that, when present together, are indicative of pericardial effusion:
- Widening of the area of cardiac dullness.
- Abrupt transition from pulmonary resonance to cardiac dullness.
- Extension of cardiac dullness into the second intercostal space
I have found that the conjunction of three signs is usually conclusive in determining the diagnosis of pericardial effusion; in the order of their importance, they are: (1) widening of the area of cardiac flatness, (2) abrupt transition from pulmonary resonance to cardiac flatness and (3) widening of the cardiac dullness in the second intercostal space. No one of these signs, taken singly, is conclusive, but together they form a triad which is thoroughly reliable, as confirmed by roentgen examination or at autopsy.
Moschcowitz 1933
Moschcowitz emphasized that while each sign individually might not be conclusive, their combination provides a reliable diagnostic indicator for pericardial effusion, as confirmed by roentgen examination or autopsy
- Eli Moschcowitz (1879-1964) was a Hungarian born, American pathologist and physician
- Moschcowitz E. A new sign of pericardial effusion. JAMA. 1933; 100(21):1663-1664
Quincke’s triad (hemobilia)
- Right hypochondrium pain
- Jaundice
- Gastrointestinal bleeding (haematemesis and melena)
1871 – Heinrich Quincke published a detailed case of hepatic artery aneurysm rupture leading to bleeding into the biliary tree. He associated three cardinal features now recognised as Quincke’s triad:
Die Krankheit begann…mit Kolik, Erbrechen und etwas Blutbeimengung im Stuhl… Der Kranke war bleich, hatte leichten Ikterus… gegen Abend Bluterbrechen…Wiederholte Blutungen aus dem Magen und schwarzer Stuhl wechselten mit Gelbsucht und Schmerzanfällen im rechten Hypochondrium – Quincke 1871
The illness began…with colic, vomiting and some blood in the stool…The patient was pale, had slight jaundice…in the evening he vomited blood…Repeated bleeding from the stomach and black stools alternated with jaundice and attacks of pain in the right hypochondrium – Quincke 1871
1975 – Eddy Davis Palmer (1917-2010) first documented use of the term Quincke’s triad of hemobilia in the second edition of his textbook Practical Points in Gastroenterology as:
Quincke’s triad of hemobilia consists of GI hemorrhage, biliary colic, and jaundice.
- Heinrich Irenaeus Quincke (1842-1922) was a German physician
- Quincke H. Ein fall von Aneurysma der Leberarterie. Berliner Klinische Wochenschrift 1871; 8: 349-352 [Hepatic artery aneurysm. Described triad of biliary tract haemorrhage]
Rigler’s Triad (1941)
Radiographic features pathognomonic for gallstone ileus, a mechanical small bowel obstruction caused by the migration of a gallstone into the gastrointestinal tract via a biliary-enteric fistula
- Ectopic gallstone (often radiopaque and located in the intestinal lumen)
- Small bowel obstruction (evident as dilated small bowel loops)
- Pneumobilia (air in the biliary tree or gallbladder lumen)
The specific signs which permit a roentgenologic diagnosis of this condition are evidences of dynamic ileus, presence of gas or contrast medium in the biliary tract and direct or indirect visualization of the calculus.
Rigler, JAMA 1941
- Leo George Rigler (1896-1979) was an American radiologist
- Rigler LG, Borman CN, Noble JF. Gallstone obstruction: pathogenesis and roentgen manifestations. JAMA. 1941; 117(21): 1753-1759
Saint’s triad (1946)
Saint’s triad refers to the clinical coexistence of three conditions:
- Hiatal hernia
- Cholelithiasis (gallstones)
- Diverticular disease (diverticulosis of colon)
…the importance of considering the possibility of multiple separate diseases in a patient whenever his or her history and the results of the physical examination were atypical of any single condition.
1946 – Charles F. M. Saint (1886–1973), Professor of Surgery at the University of Cape Town, anecdotally highlighted the importance of suspecting multiple coexisting diseases when clinical signs diverged from classic presentations.
1948 – Radiologist C.J.B. Muller at Johannesburg General Hospital published the first clinical report of Hiatus hernia, diverticula and gall stones* : Saint’s triad in three patients.
- Charles Frederick Morris Saint (1886-1973) was an English-born South African surgeon
- Muller CJB. Hiatus hernia, diverticula and gall stones* : Saint’s triad. South African Medical Journal 1948; 22(11): 376-382
Samter’s triad (1968)
- Bronchial asthma,
- Chronic sinus inflammation with recurrent nasal polyps
- Aspirin sensitivity/intolerance (and other NSAID that inhibit an enzyme called cyclooxygenase-1)
Samter’s Triad, or Aspirin-Exacerbated Respiratory Disease (AERD), is a chronic condition defined by asthma, chronic sinus inflammation with recurrent nasal polyps, and sensitivity to aspirin and other NSAIDs. It typically develops in adulthood, causing severe respiratory reactions, sinus issues, and loss of smell.
- Max Samter (1908–1999) was a German-American immunologist
- Widal F, Abrama P, Lermoyez J. Anaphylaxie et idiosyncrasie. Presse Medicale. 1922; 30: 189–193
- Samter M, Beers RF Jr. Intolerance to aspirin. Clinical studies and consideration of its pathogenesis. Ann Intern Med. 1968 May;68(5):975-83.
- Kim SD, Cho KS. Samter’s Triad: State of the Art. Clin Exp Otorhinolaryngol. 2018 Jun;11(2):71-80.
Virchow’s Triad
Whipple’s triad (1938)
- Symptoms consistent with hypoglycemia: These include neuroglycopenic symptoms (confusion, blurred vision, seizures, altered mental status) and autonomic/adrenergic symptoms (sweating, palpitations, tremor, hunger).
- Low plasma glucose concentration: Generally defined as blood sugar below 55 mg/dL (3.0 mmol/L) at the time of symptoms.
- Relief of symptoms upon correcting glucose: The immediate reversal of symptoms after administering carbohydrates or raising blood sugar.
Three criteria (Whipple criteria) which were deemed suggestive of hypoglycaemia that may indicate the presence of pancreatic insulinomas requiring surgical management:
- Allen Oldfather Whipple (1881-1963) was an American surgeon.
- Whipple AO. The Surgical Therapy of Hyperinsulinism. Journal International de Chirurgie. 1938; 3: 237-276
Zieve’s triad (1958)
Acute alcohol-induced hepatic injury and fatty liver disease. The syndrome typically follows a binge or withdrawal phase in chronic alcohol use. Episodes resolve with abstinence and supportive management.
- Jaundice
- Haemolytic anaemia
- Transient hyperlipidaemia
1958 – First described by Leslie Zieve as a distinct, self-limited syndrome of haemolysis, jaundice, and hyperlipidaemia in patients with alcoholic steatohepatitis. The haemolysis is thought to result from altered red blood cell membrane composition due to hepatic dysfunction and elevated plasma lipids.
- Leslie Zieve (1915-2000) was an American hepatologist
- Zieve L. Jaundice, hyperlipemia and hemolytic anemia: a heretofore unrecognized syndrome associated with alcoholic fatty liver and cirrhosis. Ann Intern Med. 1958 Mar;48(3):471-96
PENTADS
TETRADS
eponymythology
the myths behind the names
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
