Georg Perthes
Georg Clemens Perthes (1869-1927) was a German surgeon.
As a surgeon, Perthes wrote on vascular and chest diseases; maxillofacial injuries; and the surgery of war. He developed a procedure to drain empyema with continuous aspiration of the pleuritic exudate; a pneumatic cuff to maintain haemostasis during limb surgery (Kirschner-Perthes cuff); and a test to evaluate the competence of deep femoral veins (Perthes test).
Early exponent of the clinical use of x-rays in Germany researching the concepts of radiation treatment and therapy. Pioneer in pioneered the use of radiation in the treatment of warts, skin cancer and breast carcinoma.
His interest in tuberculosis and tuberculous hip disease, led to in depth study of atypical hip cases he termed arthritis deformans juvenilis Legg-Calvé-Perthes disease (1910). Perthes took the first X-rays of a patient with LCPD in 1898
Biographical Timeline
- 1869 – Born January 17 in Moers, Rhineland, Germany, son of the Gymnasialoberlehrer Clemens Perthes and his wife. His mother died of tuberculosis during his youth; his father later moved to Davos, Switzerland, to teach tubercular children.
- 1883 – At age 14, his father died. Georg was raised by his aunt Agnes Perthes, who connected him with prominent surgeon Friedrich Trendelenburg (1844-1924), who became his mentor.
- 1891 – Completed medical studies in Bonn, Berlin, and Freiburg; received his doctorate.
- 1895 – Became assistant to Friedrich Trendelenburg at Leipzig, beginning a lifelong professional and personal collaboration.
- 1898 – Habilitation in surgery.
- 1900–1901 – Served as military surgeon with the German army in the Boxer Rebellion, posted to Tsingtao (Qingdao), China. Conducted radiographic studies, including pioneering X-rays of bound feet of Chinese women.
- 1903 – Appointed Extraordinary Professor and Director of the Surgical-Polyclinic Institute, Leipzig. Early reports on the biological and therapeutic effects of Röntgen radiation.
- 1910 – Appointed Professor of Surgery and Director of the Surgical Clinic at the University of Tübingen, a position he held until death. Published on juvenile arthritis deformans (later Legg–Calvé–Perthes disease).
- 1914–1918 (WWI) – Served as German military surgeon; published on peripheral nerve and maxillofacial injuries.
- 1920s – Continued surgical innovation, including suction drainage of empyema, use of the pneumatic cuff for haemostasis, and reconstructive procedures for joint deformities.
- 1927 – Died January 3 following a stroke at Arosa, Switzerland while on a winter holiday, aged 57.
Medical Eponyms
Perthes test (1895)
Clinical test for assessing the competence of the deep venous system in patients with varicose veins.
1895 – Perthes described the manoeuvre in his paper “Über die Operation der Unterschenkelvarizen nach Trendelenburg”. The method involved elevation of the leg and application of a firm elastic bandage from the toes to the thigh to obliterate the superficial veins. The patient was then asked to walk with the bandage in situ:
- If deep veins obstructed, the patient experienced pain, swelling, and worsening of the varices.
- If deep veins patent, the patient experienced no pain and the superficial varices collapsed.
“…wenn der Kranke mit verbundenem Beine umhergeht und die Venen sich nicht füllen, so ist dies ein Beweis für die Durchgängigkeit der tiefen Venen…”
Perthes, 1895
(“…if the patient walks with the bandaged leg and the veins do not fill, this is proof of the patency of the deep veins…”)
The modified Perthes test involves applying a tourniquet at the sapheno-femoral junction rather than bandaging the entire leg. Both variants became standard clinical manoeuvres for differentiating superficial from deep venous incompetence before the era of duplex ultrasound.
Perthes Lesion (1906) [Perthes-Bankart lesion; Bankart lesion]
Antero-inferior detachment of the glenoid labrum, commonly (85-97%) associated with first-time traumatic anterior shoulder dislocations.
1906 – Perthes published an early pathological description of recurrent anterior shoulder dislocation. He recognised that instability was not due only to capsular laxity, but often to detachment of the labrum glenoidale from the inner rim of the glenoid fossa.
Die operative Behandlung der rezidivierenden Schultergelenksluxation ist noch kein abgeschlossenes Kapitel der Chirurgie…Bedeutungsvoller scheint mir vielmehr in einer gewissen Gruppe von Fällen der Abriß der am Tuberculum majus inserierenden Muskeln, und in einer anderen der Abriß des Labrum glenoidale am inneren Pfannenrande. Die Rücksicht auf diese pathologischen Veränderungen führte mich dazu, in zwei Fällen die verloren gegangene Insertion der Muskeln am Tuberculum majus wiederherzustellen, in einem weiteren Fall die am inneren Pfannenrand abgesprengte Gelenklippe wieder zu befestigen, während in einem vierten Falle nur die Verkleinerung und Verstärkung der erweiterten und erschlafften Kapsel ausgeführt wurde.
The operative treatment of recurrent shoulder subluxations is still no concluded chapter in surgery…Of significance is a group of cases with tearing of the muscles inserting on the major tubercle, and another group, with tearing of the glenoid labrum on the inner glenoid fossa. The consideration of these pathological changes led me to reconstruct the lost insertion point of the muscles on the major tubercle in two cases, in a further case to reattach the labrum to the glenoid, whilst in a fourth only the reduction and reinforcement of the enlarged and loosened capsule was performed – Perthes, 1906; 85: 199-227
1938 – Arthur Sydney Blundell Bankart standardised and popularised the surgical repair, leading to enduring eponym “Bankart lesion/repair.”. However, Perthes’ contribution remains historically important and some authors refer to it as the “Bankart–Perthes lesion.”
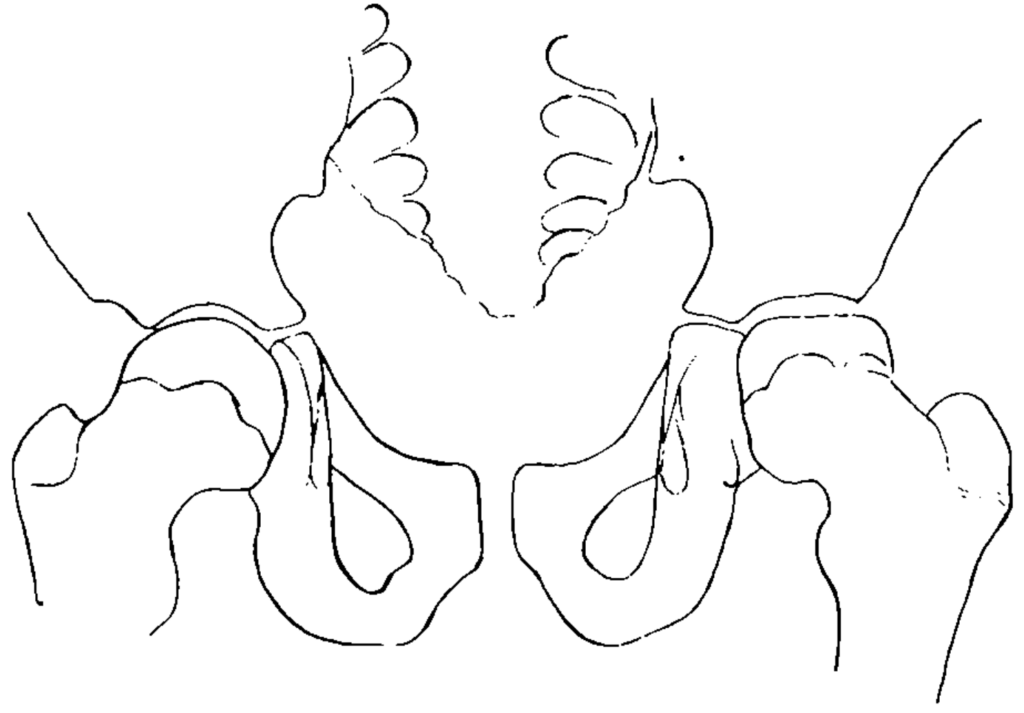
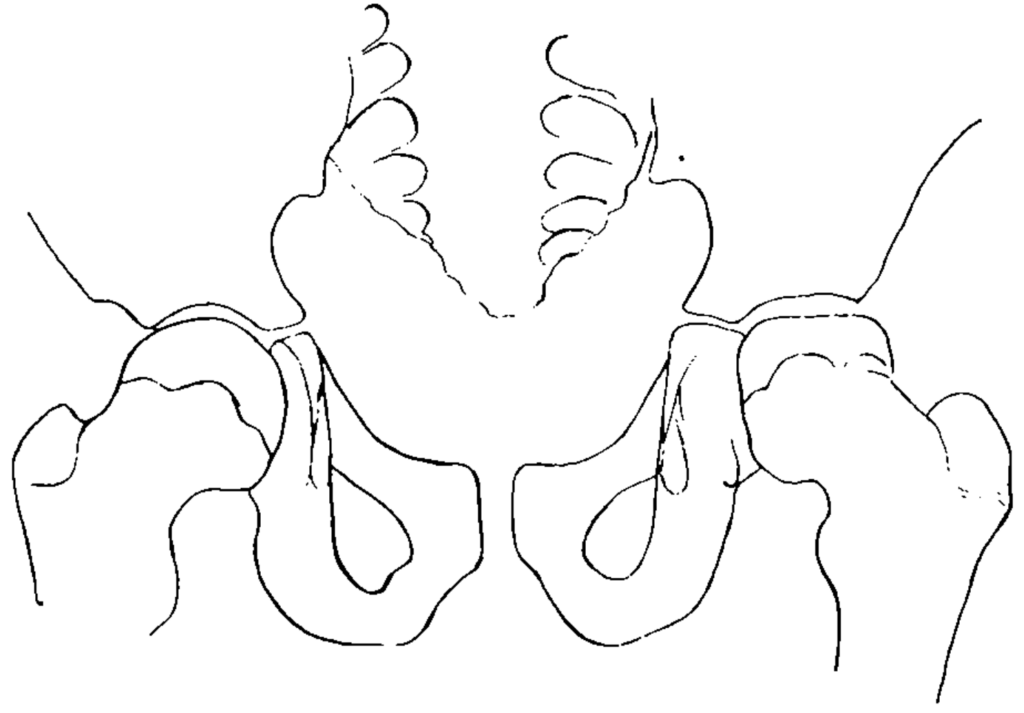
Legg-Calvé-Perthes disease (LCPD); (1910)
Legg–Calvé–Perthes disease (LCPD) is an idiopathic avascular necrosis of the proximal femoral epiphysis in children. It typically presents insidiously, sometimes after minor trauma, with hip pain, limp, or restricted movement. It most often affects boys aged 4–10 years, is unilateral in 90% of cases, and when bilateral, the hips are usually affected sequentially rather than simultaneously.
In 1910, Legg, Calvé and Perthes independently reported a hip disease in children with a symptomatic picture resembling that described by Henning Waldenström in 1909. These authors believed the process to be unrelated to tuberculosis:
Perthes highlighted the unique morphology of the femoral head and suggested vascular pathology as a key mechanism. He refuted the importance of trauma but opined the disease he termed ‘Arthritis deformans juvenilis‘ was the result of an inflammatory process in the joint that had occurred during the years of infancy. Furthermore, he commented on the likely importance of poor vasculature being a contributing aetiological factor.
Im Februar 1909 wurde ein 11jähriger Knabe zur Poliklinik gebracht, weil seinen Eltern ein wenig hinkender Gang aufgefallen war. Der Trochanter stand 1 cm über der Roser-Nélatonschen Linie. Schmerzen bestanden weder bei den Beugebewegungen, noch bei Druck auf das Gelenk. Das Röntgenbild zeigte, daß unser erster Gedanke an eine Coxa vara nicht richtig war. Der Schenkelhalswinkel war völlig normal; dagegen zeigte der Schenkelkopf an Stelle der Kugelform die Form eines Kegels…
Wenn wir zum Schluß auf die Ätiologie der juvenilen Arthritis deformans des Hüftgelenks und auf die Auffassung eingehen, welche das Leiden erfahren hat, so stoßen wir nun auf Hypothesen und können nichts anderes tun, als unbewiesene Anschauungen auf ihren Wert prüfen.
Jedenfalls werden wir an der interessanten Möglichkeit nicht zweifeln können, daß die Arthritis deformans juvenilis auf eine anscheinend zunächst ohne Folgen ausgeheilte Hüftgelenksentzündung im Säuglingsalter zurückgeht…
Als ätiologisch bedeutungsvollsten pathologischen Befund betrachtet Wollenberg die von ihm nachgewiesenen Veränderungen kleiner Knochengefäße (Endarteritis obliterans) und Stauungen in den Venen. Diese Veränderungen, die selbst durch verschiedenartige Ursachen hervorgerufen werden, können doch…das Bild der Arthritis deformans hervorrufen, indem der Arterienverschluß zu Ernährungsstörungen im Knochen, die Stauung zu Wucherungsvorgängen führt.
In February 1909 an 11 year old boy was brought to the clinic, as his parents had noticed a somewhat limping gait. The trochanter lay 1cm above the Roser-Nélaton line. Pain was not elicited on active movement, nor with pressure on the joint. The X-ray showed that our initial thought of Coxa vara was not correct. The femoral neck was completely normal; in contrast the femoral head appeared to have a conical, rather than a rounded shape.
To end, if we consider the aetiology of the juvenile Arthritis deformans, and the conception of this illness, we encounter hypotheses and can do nothing other than test unproven opinions for their merit.
In any case we cannot doubt of the interesting possibility, that the juvenile arthritis deformans can be traced back to a seemingly initially inconsequential inflammation of the hip in infancy.
The most aetiologically significant pathological discovery, according to Wollenberg, it the changes he has demonstrated in the small bony vasculature (Endarteritis obliterans), and the venous congestion. These changes, which can be the sequel of different causes themselves, can indeed…create the picture of arthritis deformans, whereby the arterial closure can lead to nutritional deficiencies in the bone, and the congestion to proliferative processes.
Major Publications
- Perthes G. Über die Operation der Unterschenkelvarizen nach Trendelenburg. Deutsche medizinische Wochenschrift, 1895; 21: 253-257. [Perthes test]
- Perthes G. Über Operationen bei habitueller Schulterluxation. Deutsche Zeitschrift für Chirurgie. 1906; 85: 199-227. [Bankart lesion] [Hills-Sachs defect]
- Perthes G. Über Arthritis deformans juvenilis. Deutsche Zeitschrift für Chirurgie. 1910; 107: 111–159. [Perthes G.On juvenile arthritis deformans. 1910. Clin Orthop Relat Res. 2012; 470(9): 2349-2368] [Legg-Calvé-Perthes disease]
- Perthes G. Über Osteochondritis deformans juvenilis. Archiv für klinische chirurgie 1913; 101: 779
- Perthes G. Über plastischen Daumenersatz insbesondere bei Verlust des ganzen Daumenstrahles. Archiv für orthopädische und Unfall-Chirurgie, 1921; 19: 198–214
References
Biography
- Sauerbruch F. Georg Perthes. Deutsche Zeitschrift für Chirurgie 1927; 200: VII
- Mostofi SB. Who’s Who in Orthopedics. Springer. 2005: 267
- Brand RA. Biographical Sketch: Georg Clemens Perthes, MD (1869–1927). Clin Orthop Relat Res. 2012; 470(9): 2347–2348.
- Bibliography. Perthes, G. WorldCat Identities
Eponymous terms
- Schulitz KP, Dustmann HO. Georg Clemens Perthes (1869–1927). In: Morbus Perthes: Ätiopathogenese, Differentialdiagnose, Therapie und Prognose. Springer. 1991: 13-15
- Pouliart N, Gagey O. Consequences of a Perthes-Bankart lesion in twenty cadaver shoulders. J Shoulder Elbow Surg. 2008 Nov-Dec;17(6):981-5.
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
