Lateral STEMI
Clinical Significance of lateral STEMI
- The lateral wall of the LV is supplied by branches of the left anterior descending (LAD) and left circumflex (LCx) arteries.
- Infarction of the lateral wall usually occurs as part of a larger territory infarction, e.g. anterolateral STEMI.
- Isolated lateral STEMI is less common, but may be produced by occlusion of smaller branch arteries that supply the lateral wall, e.g. the first diagonal branch (D1) of the LAD, the obtuse marginal branch (OM) of the LCx, or the ramus intermedius.
- Lateral STEMI is a stand-alone indication for emergent reperfusion.
- Lateral extension of an anterior, inferior or posterior MI indicates a larger territory of myocardium at risk with consequent worse prognosis.
How to recognise a lateral STEMI
- ST elevation in the lateral leads (I, aVL, V5-6).
- Reciprocal ST depression in the inferior leads (III and aVF).
- ST elevation primarily localised to leads I and aVL is referred to as a high lateral STEMI.
NB. Reciprocal change in the inferior leads is only seen when there is ST elevation in leads I and aVL. This reciprocal change may be obliterated when there is concomitant inferior ST elevation (i.e an inferolateral STEMI)
Patterns of lateral infarction
Three broad categories of lateral infarction:
- Anterolateral STEMI due to LAD occlusion.
- Inferior-posterior-lateral STEMI due to LCx occlusion.
- Isolated lateral infarction due to occlusion of smaller branch arteries such as the D1, OM or ramus intermedius.
ECG Examples
Example 1
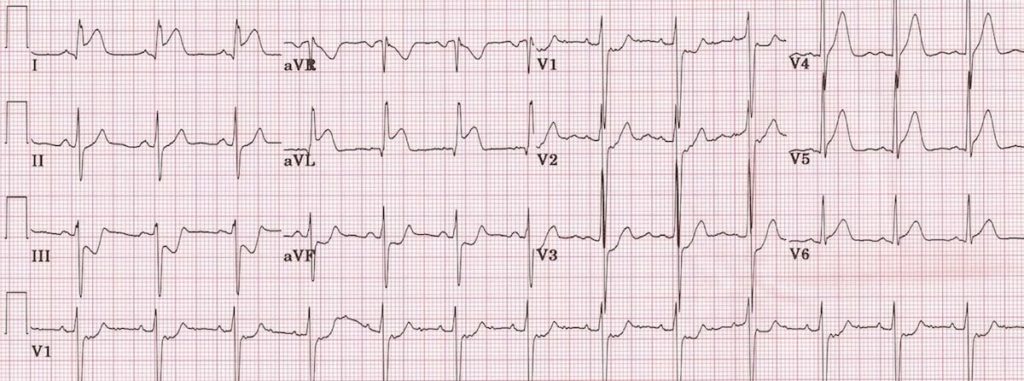
- ST elevation is present in the high lateral leads (I and aVL).
- There is also subtle ST elevation with hyperacute T waves in V5-6.
- There is reciprocal ST depression in the inferior leads (III and aVF) with associated ST depression in V1-3 (which could represent anterior ischaemia or reciprocal change).
- This pattern is consistent with an acute infarction localised to the superior portion of the lateral wall of the left ventricle (high lateral STEMI).
- The culprit vessel in this case was an occluded first diagonal branch of the LAD.
This ECG is reproduced from an article by Zajarias et al. in the Journal of Invasive Cardiology. Interestingly, this particular STEMI occurred in a 19-year old male as the result of blunt myocardial trauma causing mechanical occlusion of the first diagonal artery. Read more about this fascinating case here.
Example 2

- ST elevation is present in the high lateral leads (I and aVL).
- There is reciprocal ST depression in the inferior leads (III and aVF).
- QS waves in the anteroseptal leads (V1-4) with poor R wave progression indicate prior anteroseptal infarction.
- This pattern suggests proximal LAD disease with an acute occlusion of the first diagonal branch (D1).
Example 3

Recent High Lateral MI:
- There is subtle ST elevation in the high lateral leads (I and avL).
- There is a pathological Q wave in aVL plus inverted T waves in both I and aVL.
- This pattern is diagnostic of a recent (“completed”) high lateral MI.
- The patient in this case had a 90% occlusion of his obtuse marginal artery (= a branch of the LCx supplying the lateral wall of the LV).
This ECG was originally featured on Dr Smith’s ECG Blog. Click here for a description of the case along with some useful pearls from Dr Smith regarding diagnosis of lateral infarction.
Example 4

Anterolateral STEMI:
- ST elevation is present in the anterior (V2-4) and lateral leads (I, aVL, V5-6).
- Q waves are present in both the anterior and lateral leads, most prominently in V2-4.
- There is reciprocal ST depression in the inferior leads (III and aVF).
- This pattern indicates an extensive infarction involving the anterior and lateral walls of the left ventricle
ST elevation in the precordial leads plus the high lateral leads (I and aVL) is strongly suggestive of an acute proximal LAD occlusion (this combination predicts a proximal LAD lesion 87% of the time).
Example 5

Hyperacute Anterolateral STEMI:
- There is early ST elevation with hyperacute T waves in the anteroseptal leads (V1-4).
- There is also subtle ST elevation in the high lateral leads (I and aVL); this may be easily missed.
- However, the presence of reciprocal ST depression in the inferior leads (III and aVF) makes the lateral ST elevation more obvious.
- This ECG represents the early stages of a large anterolateral infarction.
- As with the previous case, the combination of ST elevation in the precordial and high lateral leads is indicative of proximal LAD occlusion.
Tip: ST depression localised to the inferior leads should prompt you to scrutinise the ECG for evidence of high lateral infarction
Example 6

Inferolateral STEMI:
- There is ST elevation in the inferior (II, III, aVF) and lateral (I, V5-6) leads.
- The precordial ST elevation extends out as far as V4, however the maximal STE is in V6.
- ST depression in V1-3 is suggestive of associated posterior infarction (the R/S ratio > 1 in V2 is consistent with this).
- This is an acute inferolateral STEMI with probable posterior extension.
- This constellation of ECG abnormalities is typically produced by occlusion of the proximal circumflex artery.
Example 7

Inferoposterolateral STEMI:
- ST elevation is present in the inferior (II, III and aVF) and lateral leads (I, V5-6).
- ST depression in V1-3 with tall, broad R waves and upright T waves and a R/S ratio > 1 in V2 indicate concomitant posterior infarction (this patient also had ST elevation in the posterior leads V7-9).
- These changes are consistent with a massive infarction involving the inferior, lateral and posterior walls of the left ventricle.
- The culprit vessel is again very likely to be an occluded proximal circumflex artery.
Related Topics
- Anterior STEMI
- Inferior STEMI
- Posterior infarction
- Right ventricular infarction
- High lateral STEMI (South Africa Flag sign)
References
- Morris F, Brady WJ. ABC of clinical electrocardiography: Acute myocardial infarction-Part I. BMJ. 2002; 324: 831-4.
- Edhouse J, Brady WJ, Morris F. ABC of clinical electrocardiography: Acute myocardial infarction-Part II. BMJ. 2002; 324: 963-6.
- Zajarias A, Thanigaraj S, Taniuchi M. Acute Coronary Occlusion and Myocardial Infarction Secondary to Blunt Chest Trauma from an Automobile Airbag Deployment Journal of Invasive Cardiology, Jan 2008.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner

