Anterior Myocardial Infarction
ECG Features of Anterior STEMI
- ST segment elevation with subsequent Q wave formation in precordial leads (V1-6) +/- high lateral leads. These changes are often preceded by hyperacute T waves
- Reciprocal ST depression in inferior leads (mainly III and aVF)
NB: The magnitude of reciprocal change in inferior leads is determined by the magnitude of ST elevation in I and aVL (as these leads are electrically opposite III and aVF), and hence may be minimal or absent in anterior STEMIs that do not involve high lateral leads.
Clinical Relevance of Anterior Myocardial Infarction
Anterior STEMI usually results from occlusion of the left anterior descending artery (LAD). Anterior myocardial infarction carries the poorest prognosis of all infarct locations, due to the larger area of myocardium infarct size.
A study comparing outcomes from anterior and inferior infarctions (STEMI + NSTEMI) found that compared with inferior MI, patients with anterior MI had higher incidences of:
- In-hospital mortality (11.9 vs 2.8%)
- Total mortality (27 vs 11%)
- Heart failure (41 vs 15%)
- Significant ventricular ectopic activity (70 vs 59%)
- Lower ejection fraction on admission (38 vs 55%)
In addition to anterior STEMI, other high-risk presentations of anterior ischaemia include left main coronary artery (LMCA) stenosis, Wellens syndrome and De Winter T waves.
Patterns of Anterior Infarction
The nomenclature of anterior infarction can be confusing, with multiple different terms used for the various infarction patterns. The following is a simplified approach to naming the different types of anterior MI.
The precordial leads can be classified as follows:
- Septal leads = V1-2
- Anterior leads = V3-4
- Lateral leads = V5-6
The different infarct patterns are named according to the leads with maximal ST elevation:
- Septal = V1-2
- Anterior = V2-5
- Anteroseptal = V1-4
- Anterolateral = V3-6, I + aVL
- Extensive anterior / anterolateral = V1-6, I + aVL
NB: While these definitions are intuitive, there is often a poor correlation between ECG features and precise infarct location as determined by imaging or autopsy. For an alternative approach to the naming of myocardial infarctions, take a look at this 2006 article from Circulation.
Clinical Pearls
Other important ECG patterns to be aware of:
- Anterior-inferior STEMI due to occlusion of a “wraparound” LAD. This presents with simultaneous ST elevation in the precordial and inferior leads, due to occlusion of a variant (“type III”) LAD that wraps around the cardiac apex to supply both the anterior and inferior walls of the left ventricle
- Left main coronary artery stenosis: widespread ST depression with ST elevation in aVR ≥ V1
- Wellens syndrome: deep precordial T wave inversions or biphasic T waves in V2-3, indicating critical proximal LAD stenosis (a warning sign of imminent anterior infarction)
- De Winter T waves: upsloping ST depression with symmetrically peaked T waves in the precordial leads; a “STEMI equivalent” indicating acute LAD occlusion.
ECG Examples
Example 1

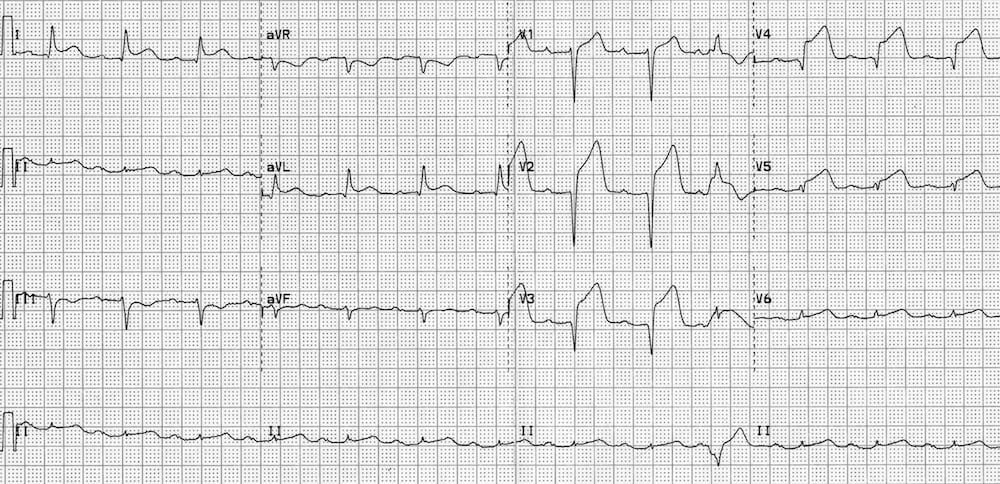
Hyperacute Anteroseptal STEMI:
- ST elevation and hyperacute T waves in V2-4
- ST elevation in I and aVL with reciprocal ST depression in lead III
- Q waves are present in the septal leads V1-2
- These features indicate a hyperacute anteroseptal STEMI
Example 2(a)

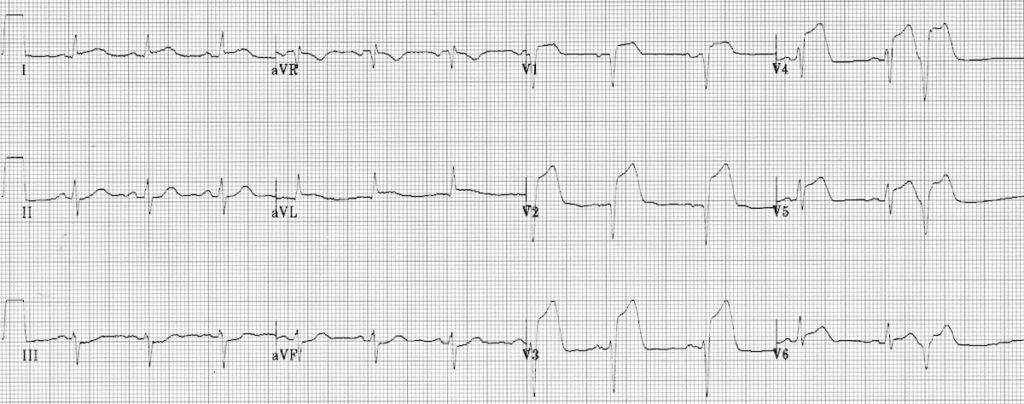
Hyperacute Anterior STEMI:
- There are hyperacute T-waves in V2-6 (most marked in V2 and V3) with loss of R wave height.
- Normal sinus rhythm with 1st degree AV block
- There are premature atrial complexes (beat 4 on the rhythm strip) and multifocal ventricular ectopy (PVCs of two different types), indicating an “irritable” myocardium at risk of ventricular fibrillation
Example 2(b)
A ECG of the same patient taken around 40-50 minutes later:
- There is progressive ST elevation and Q wave formation in V2-5
- ST elevation is now also present in I and aVL
- There is some reciprocal ST depression in lead III
Example 3

Extensive Anterolateral STEMI (acute):
- ST elevation in V2-6, I and aVL.
- Reciprocal ST depression in III and AVF.
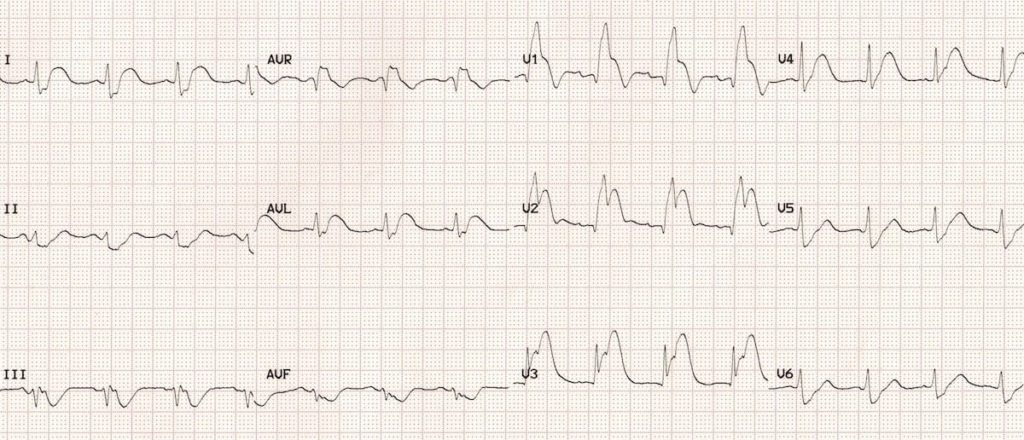
Example 4
Extensive Anterior STEMI (acute):
- ST elevation in V1-6 plus I and aVL (most marked in V2-4)
- Minimal reciprocal ST depression in III and aVF
- Q waves in V1-2, reduced R wave height (a Q-wave equivalent) in V3-4
- There is a premature ventricular complex (PVC) with “R on T’ phenomenon at the end of the ECG; this puts the patient at risk for malignant ventricular arrhythmias
Example 5
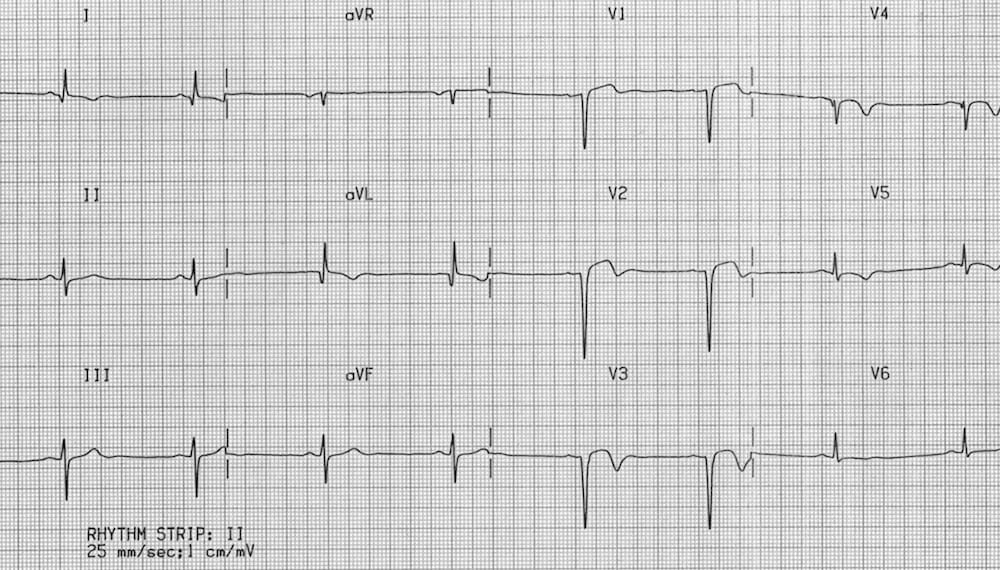
Prior Anteroseptal / Lateral MI
- Deep Q waves in V1-3 with markedly reduced R wave height in V4.
- Residual ST elevation in V1-3 (“left ventricular aneurysm” morphology)
- Biphasic/inverted T waves in V1-5
- Poor R wave progression (R wave height < 3mm in V3)
- Abnormal Q waves and T-wave inversion in I and aVL
- The pattern indicates prior infarction of the anteroseptal and lateral walls
Example 6

Extensive anterior MI (“tombstoning” pattern)
- Massive ST elevation with “tombstone” morphology is present throughout the precordial (V1-6) and high lateral leads (I, aVL)
- This pattern is seen in proximal LAD occlusion and indicates a large territory infarction with a poor LV ejection fraction and high likelihood of cardiogenic shock and death
Example 7

Anterior-inferior STEMI
- ST elevation is present throughout the precordial and inferior leads
- There are hyperacute T waves, most prominent in V1-3
- Q waves are forming in V1-3, as well as leads III and aVF
- This pattern is suggestive of occlusion occurring in “type III” or “wraparound” LAD (i.e. one that wraps around the cardiac apex to supply the inferior wall)
Prediction of the Site of LAD Occlusion
The site of LAD occlusion (proximal versus distal) predicts both infarct size and prognosis.
- Proximal LAD / LMCA occlusion has a significantly worse prognosis due to larger infarct territory size and more severe haemodynamic disturbance
- The site of occlusion can be inferred from the pattern of ST changes in leads corresponding to the two most proximal branches of the LAD: the first septal branch (S1) and the first diagonal branch (D1).
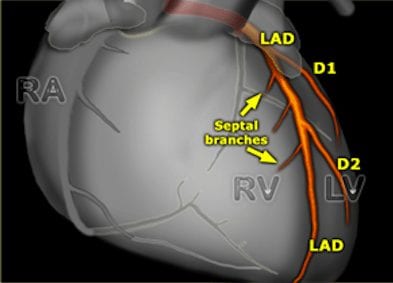
[This great diagram was originally featured on The Radiology Assistant – follow the link for a more detailed review of coronary artery anatomy.]
Territories
- S1 supplies the basal part of the interventricular septum, including the bundle branches (corresponding to leads aVR and V1)
- D1 supplies the high lateral region of the heart (leads I and aVL)
Occlusion proximal to S1
Signs of basal septal involvement:
- ST elevation in aVR
- ST elevation in V1 > 2.5 mm
- Complete RBBB
- ST depression in V5
Occlusion proximal to D1
Signs of high lateral involvement:
- ST elevation / Q-wave formation in aVL and I
- ST depression ≥ 1 mm in II, III or aVF (reciprocal to STE in aVL)
In the context of anterior STEMI, ST elevation in aVR of any magnitude is 43% sensitive and 95% specific for LAD occlusion proximal to S1. Right bundle branch block in anterior MI is an independent marker of poor prognosis; this is due to the extensive myocardial damage involved rather than the conduction disorder itself.
More Examples
Example 8
This patient’s ECG shows several signs of a very proximal LAD occlusion (ostial LAD occlusion septal STEMI):
- There is a septal STEMI with ST elevation maximal in V1-2 (extending out to V3).
- There is a new bifascicular block (RBBB + LAFB)
- Marked ST elevation (> 2.5 mm) in V1 plus STE in aVR — these features suggest occlusion proximal to S1
This patient came in post VF arrest and was taken straight to the cath lab where he was found to have a complete ostial occlusion of his LAD.
Example 9

Acute anteroseptal STEMI with STE maximal in V1-4. The following signs of proximal LAD occlusion are present:
- RBBB
- STE in aVR
- STE in aVL
- > 1 mm ST depression in the inferior leads
Learn From The Experts!
- Dr Smith’s ECG Blog – Subtle Anterior STEMI
- Dr Smith’s ECG Blog – The Smith Equation For Ruling In Subtle Anterior STEMI
- Dr Smith’s ECG Blog – How To Recognise LAD Occlusion
- Dr Smith’s ECG Blog – Wraparound LAD
Related Topics
LAD Stenosis Syndromes
Other STEMI patterns
References
- Arbane M, Goy JJ. Prediction of the site of total occlusion in the left anterior descending coronary artery using admission electrocardiogram in anterior wall acute myocardial infarction. Am J Cardiol. 2000 Feb 15;85(4):487-91, A10 [PMID 10728956]
- Aygul N, et al. Value of lead aVR in predicting acute occlusion of proximal left anterior descending coronary artery and in-hospital outcome in ST-elevation myocardial infarction: an electrocardiographic predictor of poor prognosis. J Electrocardiol. 2008 Jul-Aug;41(4):335-41 [PMID 18455178]
- Bayés de Luna A, et al. International Society for Holter and Noninvasive Electrocardiography. A new terminology for left ventricular walls and location of myocardial infarcts that present Q wave based on the standard of cardiac magnetic resonance imaging: a statement for healthcare professionals from a committee appointed by the International Society for Holter and Noninvasive Electrocardiography. Circulation. 2006 Oct 17;114(16):1755-60.
- Barrabes JA, Figueras J, Moure C, Cortadellas J, Soler-Soler J. Prognostic value of lead aVR in patients with a first non-ST-segment elevation acute myocardial infarction. Circulation 2003; 108: 814 – 819
- Birnbaum Y, Hasdai D, Sclarovsky S, Herz I, Strasberg B, Rechavia E. Acute myocardial infarction entailing ST-segment elevation in lead aVL: electrocardiographic differentiation among occlusion of the left anterior descending, first diagonal, and first obtuse marginal coronary arteries. Am Heart J. 1996 Jan;131(1):38-42 [PMID 8554017]
- Engelen DJ, Gorgels AP, Cheriex EC, De Muinck ED, Ophuis AJ, Dassen WR et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol. 1999 Aug;34(2):389-95
- Eskola MJ, Nikus KC, Holmvang L, et al. Value of the 12-lead electrocardiogram to define the level of obstruction in acute anterior wall myocardial infarction: Correlation to coronary angiography and clinical outcome in the DANAMI-2 trial. Int J Cardiol 2009;131:378–383 [PMID 18191483]
- Hennings JR, Fesmire FM. A new electrocardiographic criteria for emergent reperfusion therapy. Am J Emerg Med. 2011 Jun 22. Epub ahead of print [PMID 21703800]
- Kosuge M, Kimura K, Ishikawa T, Ebina T, Shimizu T, Hibi K, et al. Predictors of left main or three-vessel disease in patients who have acute coronary syndromes with non-ST-segment elevation. Am J Cardiol 2005; 95: 1366 – 1369 [PMID 15904646]
- Rostoff P, Piwowarska W, Konduracka E, Libionka A, Bobrowska- Juszczuk M, Stopyra K, et al. Value of lead aVR in the detection of significant left main coronary artery stenosis in acute coronary syndrome. Kardiol Pol 2005;62:128-37 [PMID 15815796]
- Stone PH, Raabe DS, Jaffe AS, et al. Prognostic significance of location and type of myocardial infarction: independent adverse outcome associated with anterior location. J Am Coll Cardiol 1988; 11:453 [PMID 3278032]
- Vasudevan K, Manjunath CN, Srinivas KH, Prabhavathi, Davidson D, Kumar S, Yavagal ST. Electrocardiographic localization of the occlusion site in left anterior descending coronary artery in acute anterior myocardial infarction. Indian Heart J. 2004 Jul-Aug;56(4):315-9 [PMID 15586740]
- Yamaji H, Iwasaki K, Kusachi S, Murakami T, Hirami R, Hamamoto H, et al. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1). J Am Coll Cardiol. 2001 Nov 1;38(5):1348-54
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner

