Posterior Myocardial Infarction
Posterior myocardial infarction (MI) accompanies 15-20% of STEMIs, usually occurring in the context of inferior or lateral infarction. Isolated posterior MI is less common (5-10% of infarcts), and the lack of ST elevation means that the diagnosis is often missed.
Posterior extension of an inferior or lateral infarct implies a much larger area of myocardial damage, with an increased risk of left ventricular dysfunction and death. Always examine closely for evidence of posterior infarction in any patient with a lateral or inferior MI.
ECG diagnostic criteria
As the posterior myocardium is not directly visualised by the standard 12-lead ECG, reciprocal changes of STEMI are sought in the anteroseptal leads V1-3.
Posterior MI is suggested by the following changes in V1-3:
- Horizontal ST depression
- Tall, broad R waves (> 30ms)
- Upright T waves
- Dominant R wave (R/S ratio > 1) in V2
In patients presenting with ischaemic symptoms, horizontal ST depression in the anteroseptal leads (V1-3) should raise the suspicion of posterior MI.
Posterior infarction is confirmed by the presence of ST elevation and Q waves in the posterior leads (V7-9).
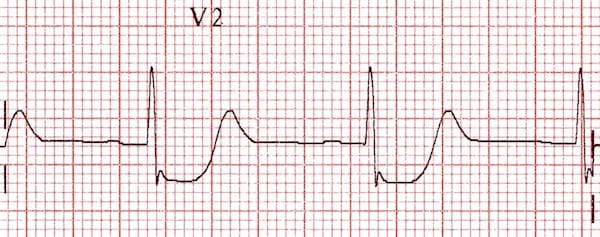
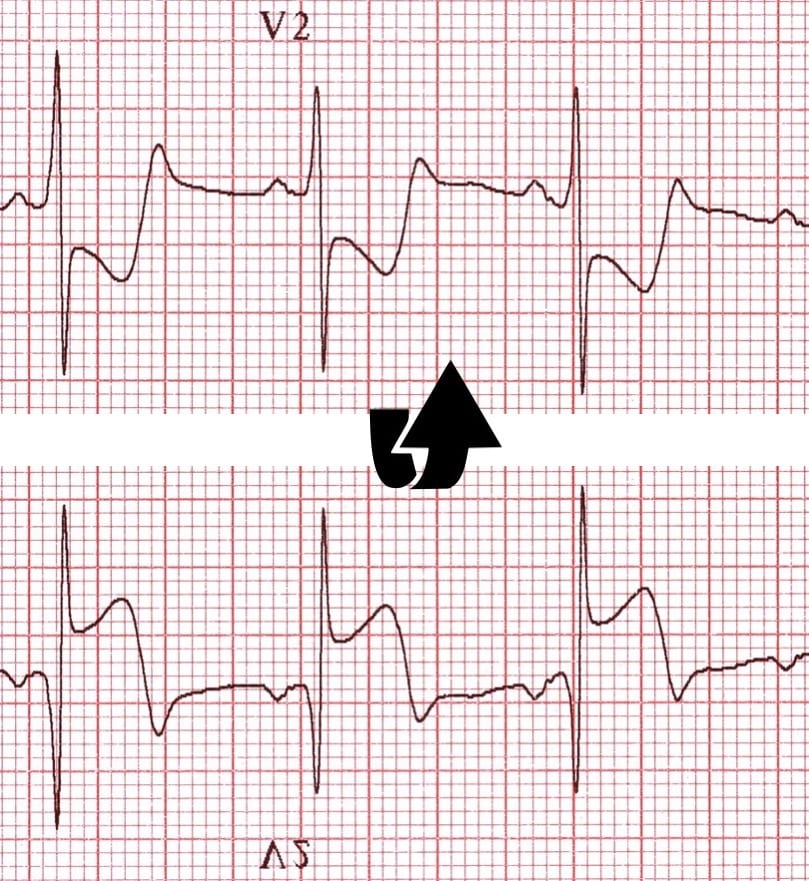
Explanation of the ECG changes in V1-3
The anteroseptal leads are directed from the anterior precordium towards the internal surface of the posterior myocardium. Because posterior electrical activity is recorded from the anterior side of the heart, the typical injury pattern of ST elevation and Q waves becomes inverted:
- ST elevation becomes ST depression
- Q waves become R waves
- Terminal T-wave inversion becomes an upright T wave
The progressive development of pathological R waves in posterior infarction (the “Q wave equivalent”) mirrors the development of Q waves in anteroseptal STEMI.

This picture illustrates the reciprocal relationship between the ECG changes seen in STEMI and those seen with posterior infarction. The previous image (depicting posterior infarction in V2) has been inverted. See how the ECG now resembles a typical STEMI!
Posterior leads
Leads V7-9 are placed on the posterior chest wall in the following positions (see diagram below):
- V7 – Left posterior axillary line, in the same horizontal plane as V6
- V8 – Tip of the left scapula, in the same horizontal plane as V6
- V9 – Left paraspinal region, in the same horizontal plane as V6

The degree of ST elevation seen in V7-9 is typically modest – note that only 0.5 mm of ST elevation is required to make the diagnosis of posterior MI!
Example ECG
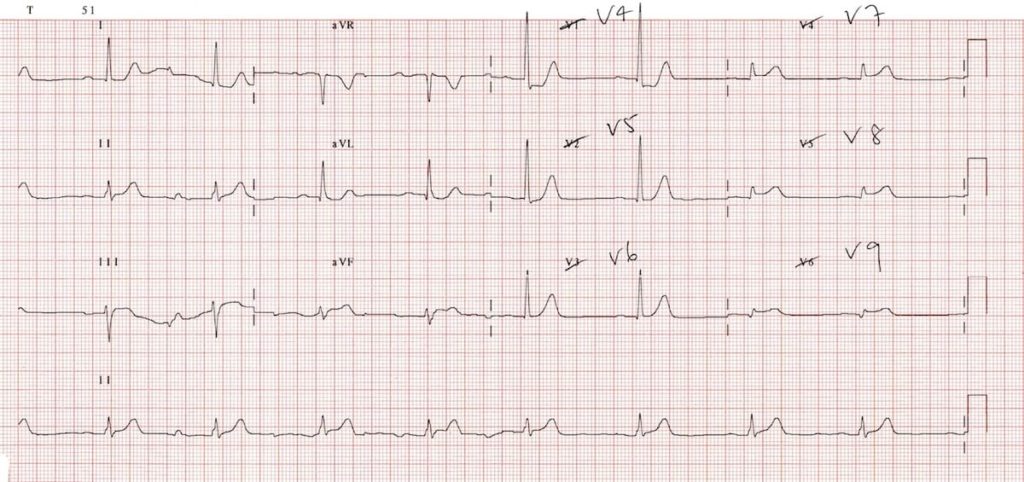
Example 1a
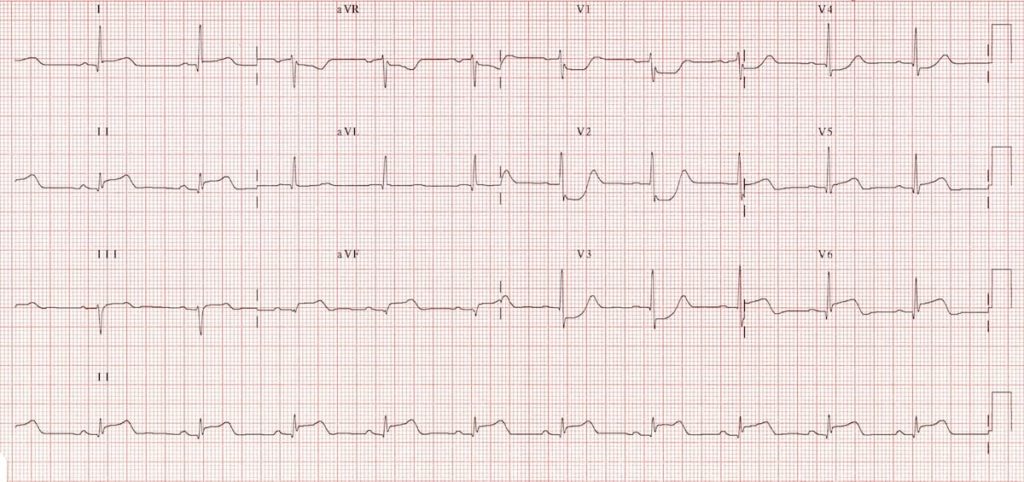
Inferolateral STEMI. Posterior extension is suggested by:
- Horizontal ST depression in V1-3
- Tall, broad R waves (> 30ms) in V2-3
- Dominant R wave (R/S ratio > 1) in V2
- Upright T waves in V2-3
Example 1b
The same patient, with posterior leads recorded:
- Marked ST elevation in V7-9 with Q-wave formation confirms involvement of the posterior wall, making this an inferior-lateral-posterior STEMI (= big territory infarct!).
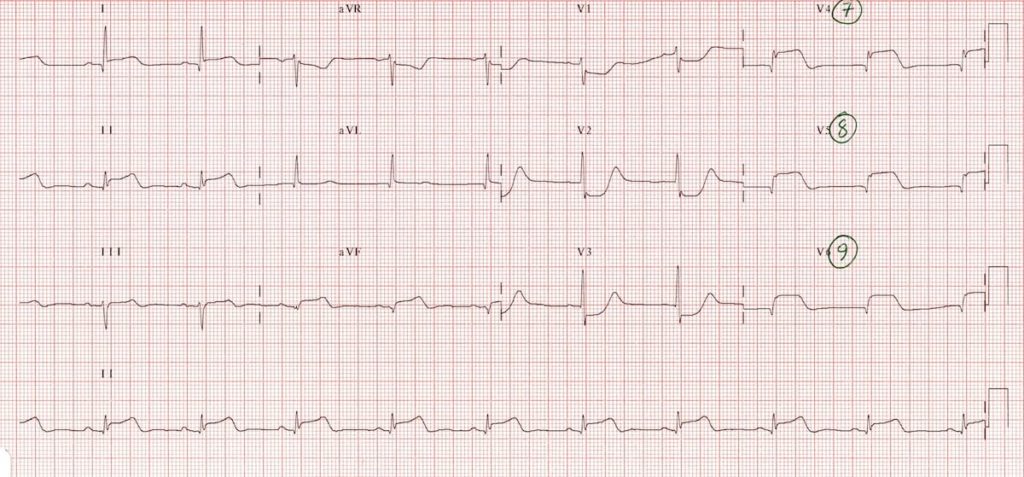
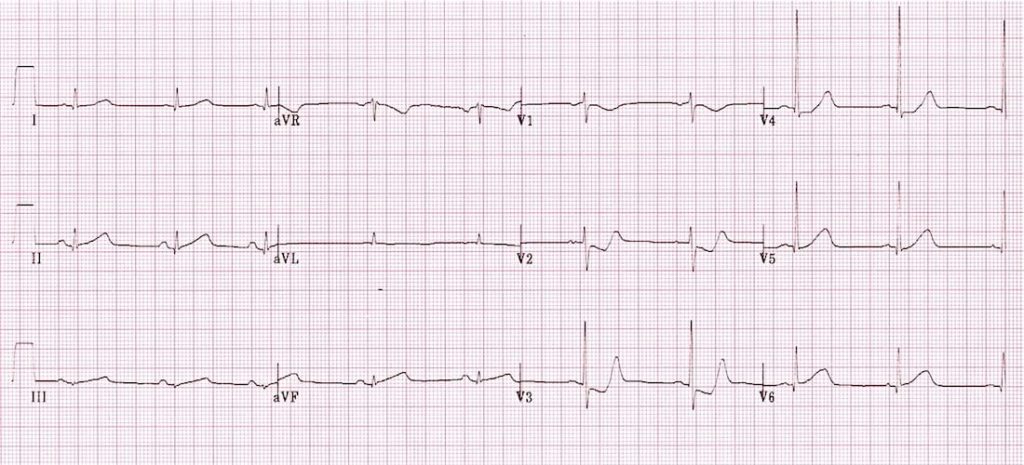
Example 2a
In this ECG, posterior MI is suggested by the presence of:
- ST depression in V2-3
- Tall, broad R waves (> 30ms) in V2-3
- Dominant R wave (R/S ratio > 1) in V2
- Upright terminal portions of the T waves in V2-3
The ECG changes extend out as far as V4, which may reflect superior-medial misplacement of the V4 electrode from its usual position
Example 2b
The same patient, with posterior leads recorded:
- Posterior infarction is diagnosed based on the presence of ST segment elevation >0.5mm in leads V7-9
- Note that there is also some inferior STE in leads III and aVF (but no Q wave formation) suggesting early inferior involvement
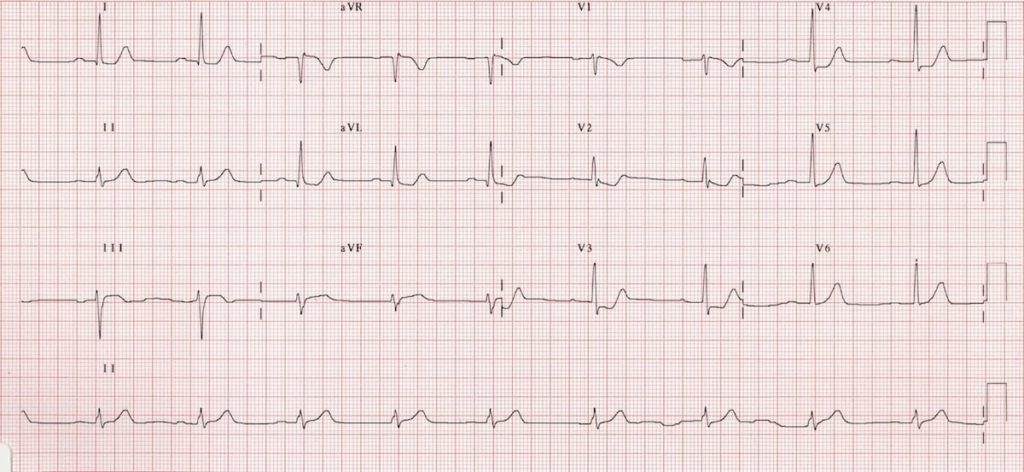
Example 3a
Patient presenting with chest pain:
- The ST depression and upright T waves in V2-3 suggest posterior MI
- There are no dominant R waves in V1-2, but it is possible that this ECG was taken early in the course of the infarct, prior to pathological R-wave formation
- There are also some features suggestive of early inferior infarction, with hyperacute T waves in II, III and aVF
Example 3b
An ECG of the same patient taken 30 minutes later:

- There is now some ST elevation developing in V6
- With the eye of faith there is perhaps also some early ST elevation in the inferior leads (lead III looks particularly abnormal)
Example 3c
The same patient with posterior leads recorded:

- Posterior infarction is confirmed by the presence of ST elevation >0.5mm in leads V7-9
Example 4a
Patient presenting with central chest pain

- Inferior STEMI with posterior extension. Extensive territory
Example 4b
The same patient with posterior leads (V8,9) recorded:

Related Topics
References
- Morris F, Brady WJ. ABC of clinical electrocardiography: Acute myocardial infarction-Part I. BMJ. 2002; 324: 831-4
- Edhouse J, Brady WJ, Morris F. ABC of clinical electrocardiography: Acute myocardial infarction-Part II. BMJ. 2002; 324: 963-6.
- Van Gorselen EO, Verheugt FW, Meursing BT, Oude Ophuis AJ. Posterior myocardial infarction: the dark side of the moon. Neth Heart J. 2007; 15: 16-21
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |


Can someone please clarify something for me. So St depression in v2 and v3. Swap leads v4, 5 and 6, and place them on the posterior aspect of the thorax as per diagram. When the ecg is recorded how come in some of the examples above leads v4, 5 and 6 are crossed out and replaced by leads v7, 8 and 9. On contrast some examples have v1, 2 and 3 cross out and are replaced by v7, 8 and 9.
Can someone please tell me the correct was to record a posterior ecg or are both ways acceptable?
Many thanks
Were you able to understand why Lee? Let me know and I’ll explain it.
Hi Mr.Lee,
1. Take conventional ECG
2 take out v4,v5,V6 and place them posteriorly. Mark as v7,v8v9.
You gotta keep two ecgs and read it.