Puzzling Paroxysmal Palpitations
aka ECG Exigency 004
A previously healthy 15-year old boy presents to ED with sudden onset of palpitations while playing sport.
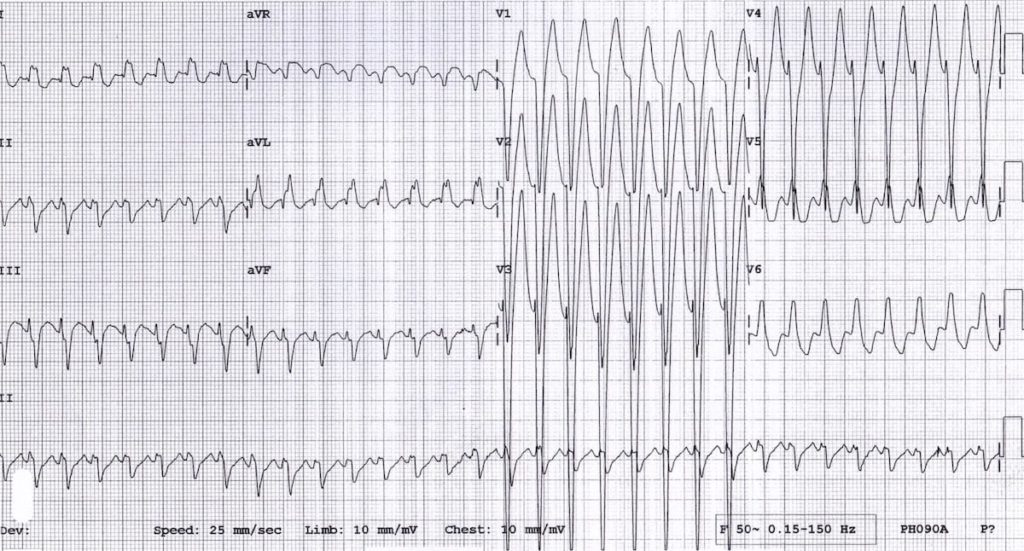
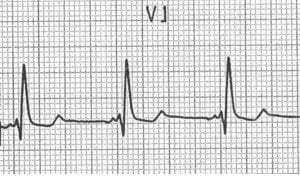
On arrival to ED he is alert and pain free with a good blood pressure. His ECG is shown below:
Q1. Describe the ECG.
Answer and Interpretation
Features of the ECG include:
- Regular broad complex tachycardia at 190 bpm
- No P waves preceding the QRS complexes
- Left axis deviation
- QRS complexes show a left bundle branch block morphology with dominant S-wave in V1, broad, notched R waves in the lateral leads (I, aVL) and secondary ST/T-wave changes
- High left ventricular voltage (HLVV)
Q2. What is the differential diagnosis of this rhythm?
Answer and Interpretation
The diagnosis of a regular broad complex tachycardia (BCT) involves a distinction between two main entities:
- Ventricular tachycardia (VT)
- Supraventricular tachycardia (SVT) with aberrant conduction
The term ‘ supraventricular tachycardia’, while often used synonymously with junctional re-entry tachycardia (JRT), can refer to any tachycardia arising above the level of the ventricles, including:
Junctional re-entry tachycardia can be divided into:
- AV nodal re-entry tachycardia (AVNRT; micro-re-entry circuit within the AV node)
- Atrio-ventricular re-entry tachycardia (AVRT; macro-re-entry circuit via an accessory pathway as seen in WPW syndrome). This can be either orthodromic, where the impulse travels down through the AV node and recycles back up the accessory pathway (producing a narrow complex SVT) or antidromic, where the impulse travels down the accessory pathway and recycles back via the AV node (producing a broad complex SVT)
Only VT and junctional tachycardia with aberrancy would produce a regular BCT with no discernible atrial activity. Sinus tachycardia, ectopic atrial tachycardia and flutter would all be expected to show characteristic P waves or flutter waves visible somewhere on the ECG.
So, the differential diagnosis of this ECG boils down to three main possibilities:
- Ventricular tachycardia
- AVNRT with LBBB
- Antidromic AVRT due to WPW
Q3. What is aberrant conduction?
Answer and Interpretation
- Aberrant conduction is any situation where electrical impulses take an abnormal route through the conducting system, leading to a broadening of the QRS complex
- The most common causes being either bundle branch block (LBBB, RBBB) or pre-excitation (e.g. Wolff-Parkinson-White syndrome).
- There are other types of aberrancy that can produce broad complexes, including conditions such as rate-related bundle branch block (discussed in ECG Exigency 002) and Ashman aberrancy (a type of transient aberrant conduction related to abrupt changes in heart rate).
Q4. Is there any way to distinguish between diagnoses based on ECG alone?
Answer and Interpretation
The answer is no!
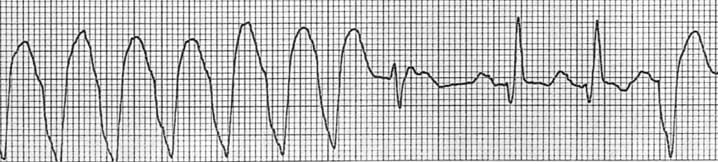
The electrocardiographic differentiation of VT from SVT with aberrancy is not always possible. There are several electrocardiographic features (not present on this ECG) that increase the likelihood of VT:
- Absence of typical RBBB or LBBB morphology
- Extreme axis deviation (“northwest axis”)
- Very broad complexes (>160ms)
- AV dissociation (P and QRS complexes at different rates)
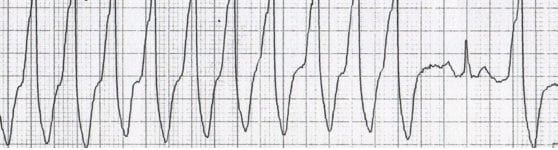
- Capture beats — occur when the sinoatrial node transiently ‘captures’ the ventricles, in the midst of AV dissociation, to produce a QRS complex of normal duration.
- Fusion beats — occur when a sinus and ventricular beat coincides to produce a hybrid complex.
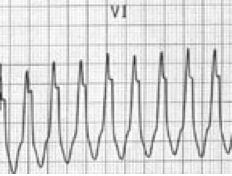
- Positive or negative concordance throughout the chest leads, i.e. leads V1-6 show entirely positive (R) or entirely negative (QS) complexes, with no RS complexes seen.
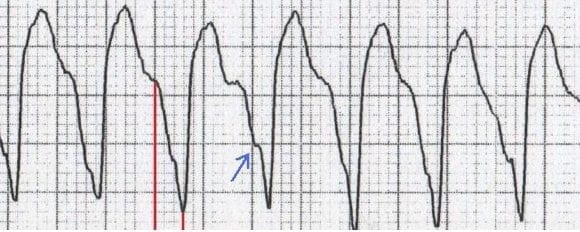
- Brugada sign – The distance from the onset of the QRS complex to the nadir of the S-wave is > 100ms
- Josephson sign – Notching near the nadir of the S-wave
- RSR’ complexes with a taller left rabbit ear. This is the most specific finding in favour of VT. This is in contrast to RBBB, where the right rabbit ear is taller.
Examples of these ECG features are shown below


Q5. What features, other than those present on the ECG, are suggestive of each of the differential diagnoses?
Answer and Interpretation
The likelihood of VT is also increased with:
- Age > 35 (positive predictive value of 85%)
- Structural heart disease
- Ischaemic heart disease
- Previous MI
- Congestive heart failure
- Cardiomyopathy
- Family history of sudden cardiac death (suggesting conditions such as HOCM, congenital long QT syndrome, Brugada syndrome or arrhythmogenic right ventricular dysplasia that are associated with episodes of VT)
The likelihood of SVT with aberrancy is increased if:
- Previous ECGs show a bundle branch block pattern with identical morphology to the broad complex tachycardia.
- Previous ECGs show evidence of WPW (short PR < 120ms, broad QRS, delta wave).
- The patient has a history of paroxysmal tachycardias that have been successfully terminated with adenosine or vagal manoeuvres.
… But don’t rely on these features to make the diagnosis!
Q6. How would manage a patient presenting with a regular BCT?
Answer and Interpretation
All these patients need to be managed in a monitored bed equipped for cardiopulmonary resuscitation, defibrillation and airway management.The first question is whether the patient is stable or unstable…
Signs of instability:
- Hypotension
- Loss of consciousness
- Chest pain
- Acute heart failure
Unstable patients require immediate synchronised DC cardioversion. Starting energy is 100 J (monophasic) or 70 J (biphasic), with titration of energy settings upwards as required.
In stable patients, consider whether SVT with aberrancy is likely.
- Previous similar episodes
- Young, fit patient with structurally normal heart
- No family history of sudden death or cardiomyopathy
In these cases, a trial of adenosine or vagal manoeuvres (Valsalva manoeuvre or carotid sinus massage) is a reasonable next step. The starting dose of adenosine is 6mg rapid IV push, preferably through a proximally-sited large-bore cannula, followed by incremental doses at 12mg and 18mg.
Beware that adenosine may occasionally provoke degeneration to VF (particularly in patients with coronary artery disease) so the patient should have defibrillator pads attached during this procedure.
If adenosine is unsuccessful, or if VT is the likely diagnosis, then the options for treatment are as follows:
- Procedural sedation and DC cardioversion – this would be the treatment of choice in a fasted patient with no significant cardio-respiratory comorbidities
- Amiodarone 150 mg IV over 10 mins (first-line antiarrhythmic)
- Lignocaine 1-1.5 mg/kg over 2-3 minutes
- Procainamide 100mg every 5 minutes up to a maximum dose of 10-20mg/kg
Serum electrolytes (potassium and magnesium) should be corrected to normal and associated conditions such as hypoxia, myocardial ischaemia and drug toxicities (e.g. poisoning with sodium-channel blocking drugs) should be treated.
Remember that overall, VT accounts for:
- 80% of cases of BCT
- 95% of cases of BCT in patients with structural heart disease
So if in doubt, treat as VT!
Q7. Can you guess the underlying diagnosis?
Answer and Interpretation
This ECG is an example of antidromic AVRT secondary to Wolff-Parksinson-White syndrome.
- The patient gave a history of previous similar palpitations and recalled one previous ED presentation where his palpitations had been successfully terminated with adenosine.
- He was due to see a cardiologist but had not yet attended his appointment.On this occasion, he reverted to sinus rhythm following a Valsalva manoeuvre, with immediate narrowing of his QRS complexes.
- Baseline ECG showed sinus rhythm with PR interval of 110ms and subtle delta waves.
- Electrophysiology testing confirmed pre-excitation with a right-sided accessory pathway (Type B WPW).
- Echocardiography revealed a structurally normal heart. He was discharged home on oral flecainide pending ablation of his accessory pathway.
References
- Hampton, JR. The ECG In Practice, 6e
- Mattu A, Brady W. ECG’s for the Emergency Physician 1
- Mattu A, Brady W. ECGs for the Emergency Physician 2
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6e
- Wagner, GS. Marriott’s Practical Electrocardiography 12e
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
CLINICAL CASES
ECG EXIGENCY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
