Atrial Fibrillation
Atrial fibrillation (AF) is the most common sustained arrhythmia. It is characterised by disorganised atrial electrical activity and contraction.
The incidence and prevalence of AF is increasing. Lifetime risk over the age of 40 years is ~25%. Complications of AF include haemodynamic instability, cardiomyopathy, cardiac failure, and embolic events such as stroke.
ECG Features of Atrial Fibrillation
- Irregularly irregular rhythm
- No P waves
- Absence of an isoelectric baseline
- Variable ventricular rate
- QRS complexes usually < 120ms, unless pre-existing bundle branch block, accessory pathway, or rate-related aberrant conduction
- Fibrillatory waves may be present and can be either fine (amplitude < 0.5mm) or coarse (amplitude > 0.5mm)
- Fibrillatory waves may mimic P waves leading to misdiagnosis
Mechanism of Atrial Fibrillation
The mechanisms underlying AF are not fully understood, but it requires an initiating event (focal atrial activity / PACs) and substrate for maintenance (i.e. dilated left atrium). Proposed mechanisms include:
- Focal activation – in which AF originates from an area of focal activity. This activity may be triggered due to increased automaticity or from micro re-entry. Often located in the pulmonary veins.
- Multiple wavelet mechanism – in which multiple small wandering wavelets are formed. The fibrillation is maintained by re-entry circuits formed by some of the wavelets. This process is potentiated in the presence of a dilated LA — the larger surface area facilitates continuous waveform propagation.
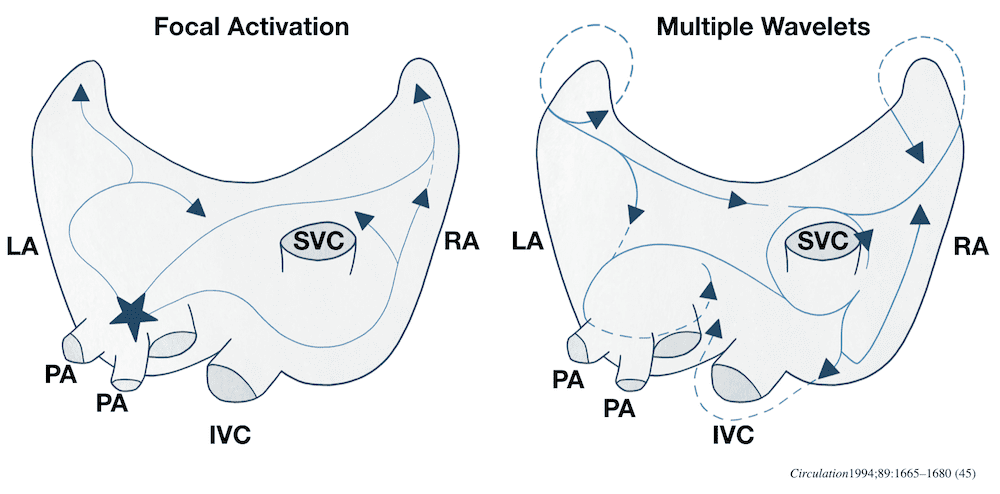
Right: Multiple small wavelets, maintained by re-entry circuits
Causes of Atrial Fibrillation
- Ischaemic heart disease
- Hypertension
- Valvular heart disease (esp. mitral stenosis / regurgitation)
- Acute infections
- Electrolyte disturbance (hypokalaemia, hypomagnesaemia)
- Thyrotoxicosis
- Drugs (e.g. sympathomimetics)
- Alcohol
- Pulmonary embolus
- Pericardial disease
- Acid-base disturbance
- Pre-excitation syndromes
- Cardiomyopathies: dilated, hypertrophic.
- Phaeochromocytoma
Other features:
- Ashman Phenomenon – aberrant ventricular conducted beats, usually of RBBB morphology, secondary to a long refractory period as determined by the preceding R-R interval
- The ventricular response and thus ventricular rate in AF is dependent on several factors including vagal tone, other pacemaker foci, AV node function, refractory period, and medications
- AF is most commonly associated with a ventricular rate ~ 110 – 160
- AF is often described as having ‘rapid ventricular response’ once the ventricular rate is > 100 bpm.
- ‘Slow’ AF is a term often used to describe AF with a ventricular rate < 60 bpm.
- Causes of ‘slow’ AF include hypothermia, digoxin toxicity, and medications.
- A connection between Sick Sinus Syndrome (SSS) or Sinus node dysfunction (SND) and atrial fibrillation (AF) has been recognized in the literature since the 1960s. There is some evidence to support AF inducing SND and some support for the notion that SND causes and promotes the development of AF. [Sinus Node Dysfunction in Atrial Fibrillation: Cause or Effect?, 2008]
Classification of Atrial Fibrillation
Classification is dependent on the presentation and duration of atrial fibrillation as below:
- First episode – initial detection of AF regardless of symptoms or duration
- Recurrent AF – More than 2 episodes of AF
- Paroxysmal AF – Self terminating episode < 7 days
- Persistent AF – Not self terminating, duration > 7 days
- Long-standing persistent AF – > 1 year
- Permanent (Accepted) AF – Duration > 1 yr in which rhythm control interventions are not pursued or are unsuccessful
Note paroxysmal AF of > 48 hr duration is unlikely to spontaneously revert to sinus rhythm and anticoagulation must be considered.
Management of Atrial Fibrillation
Management of atrial fibrillation is complex, and depends on the duration of atrial fibrillation, co-morbidities, underlying cause, symptoms, and age. Management can be considered in a step-wise manner:
- Diagnosis of atrial fibrillation
- Assessment of duration
- Assessment for anticoagulation
- Rate or rhythm control
- Treatment of underlying / associated diseases
Guidelines for the Management of Atrial Fibrillation
A number of national and international guidelines exist for the management of AF including:
- European Society of Cardiology Guidelines 2016
- American College of Cardiology Foundation Atrial Fibrillation Toolkit
- Canadian Cardiovascular Society Guidelines 2016
- NICE Guideline Atrial fibrillation management
Risk of Stroke and Anticoagulation
- Atrial fibrillation is associated with disorganised atrial contraction and stasis within the left atrial appendage with associated thrombus formation and risk of embolic stroke
- AF associated with valvular disease has a particularly high risk of stroke
- Guideline recommendations for stroke prevention and anticoagulation also include atrial flutter due to the high likelihood of these patients developing AF
- Anticoagulation strategies may include NOACs, warfarin, aspirin, and clopidogrel
- Anticoagulation guidelines are based on risk of stroke vs. risk of bleeding.
- Stroke risk stratification requires either an assessment of risk factors or application of a risk score e.g. CHADS2 or CHA2DS2VASc.
- CHADS2 calculator via MDCalc
- CHA2DS2-VASc calculator via MDCalc
Atrial Fibrillation in Wolff-Parkinson-White Syndrome
- Atrial fibrillation can occur in up to 20% of patients with Wolff-Parkinson-White Syndrome (WPW)
- The accessory pathway allows for rapid conduction directly to the ventricles bypassing the AV node
- Rapid ventricular rates may result in degeneration to VT or VF
ECG features of Atrial Fibrillation in WPW:
- Rate > 200 bpm
- Irregular rhythm
- Wide QRS complexes due to abnormal ventricular depolarisation via accessory pathway
- QRS complexes change in shape and morphology
- Axis remains stable, unlikely polymorphic VT
Treatment
- Treatment with AV nodal blocking drugs e.g. adenosine, calcium-channel blockers, beta-blockers may increase conduction via the accessory pathway with a resultant increase in ventricular rate and possible degeneration into VT or VF
- In a haemodynamically unstable patient urgent synchronised DC cardioversion is required.
- Medical treatment options in a stable patient include procainamide or ibutilide, although DC cardioversion may be preferred
ECG Examples
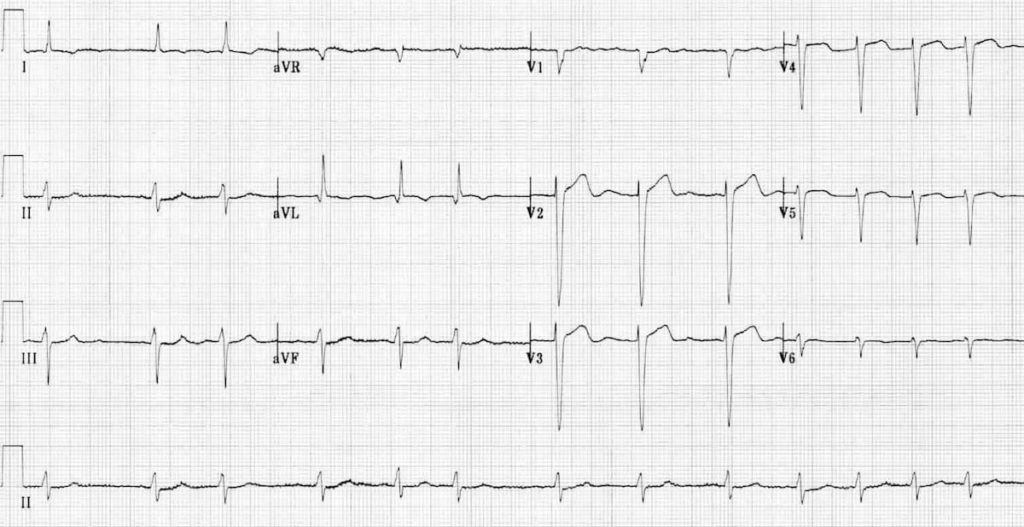
Example 1
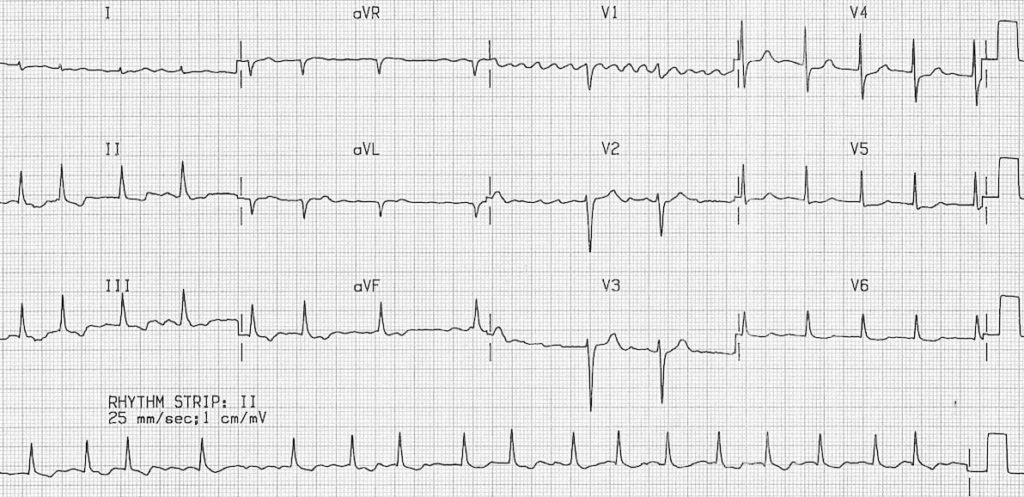
Atrial fibrillation:
- Irregular ventricular response
- Coarse fibrillatory waves are visible in V1
- “Sagging” ST segment depression is visible in V6, II, III and aVF, suggestive of digoxin effect
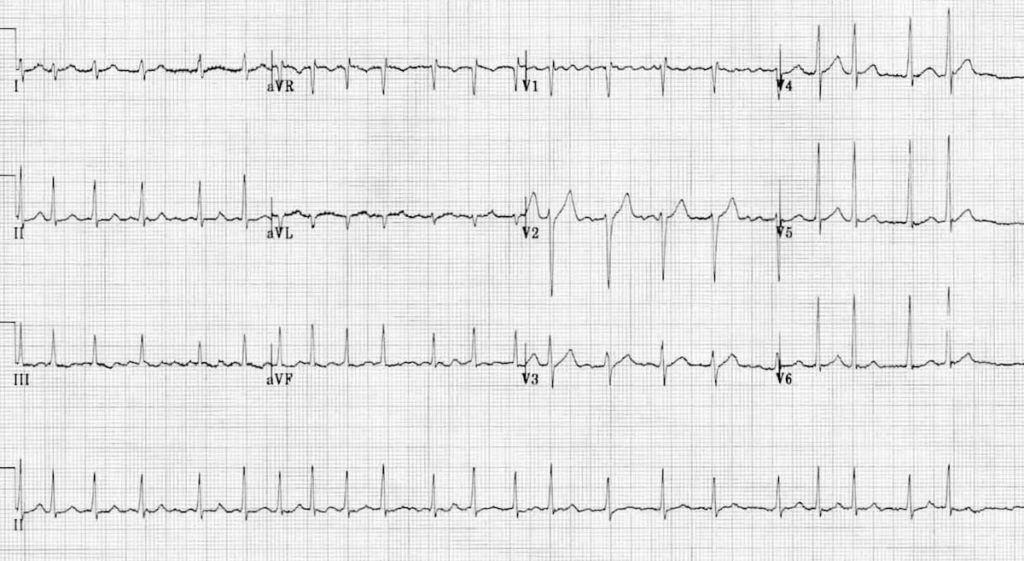
Example 2
Atrial fibrillation:
- Irregular ventricular response
- Coarse fibrillatory waves are visible in V1
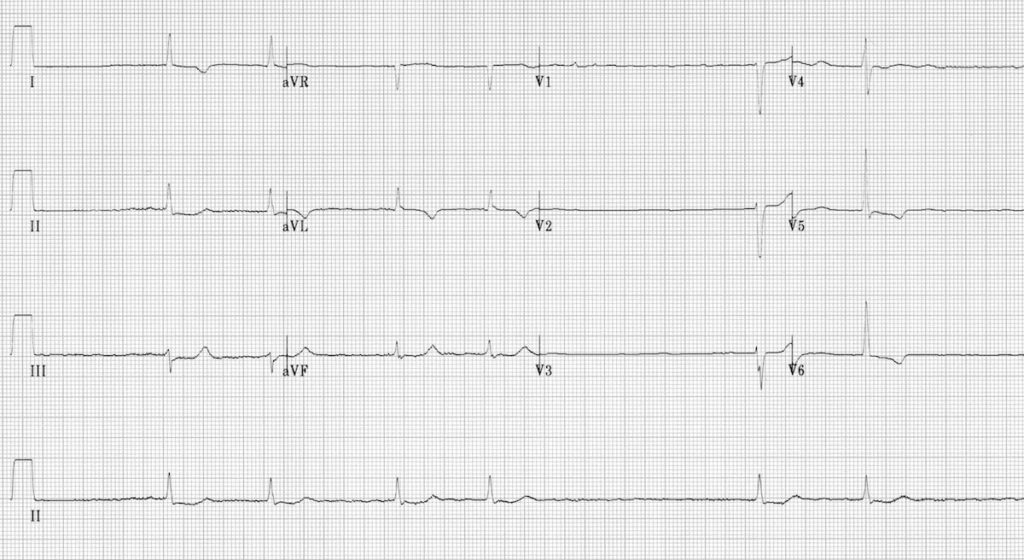
Example 3
Atrial fibrillation:
- Irregular ventricular response
- No evidence of organised atrial activity
- Fine fibrillatory waves seen in V1
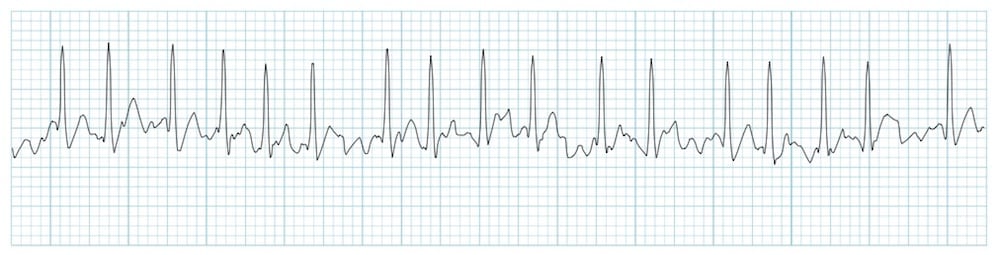
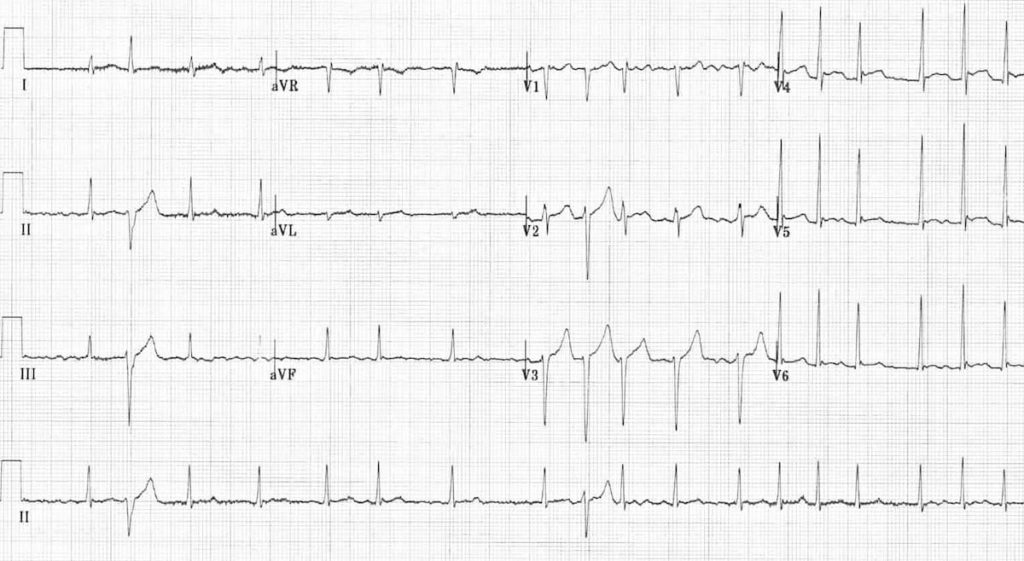
Example 4
AF with rapid ventricular response
- Irregular narrow-complex tachycardia at ~135 bpm
- Coarse fibrillatory waves in V1
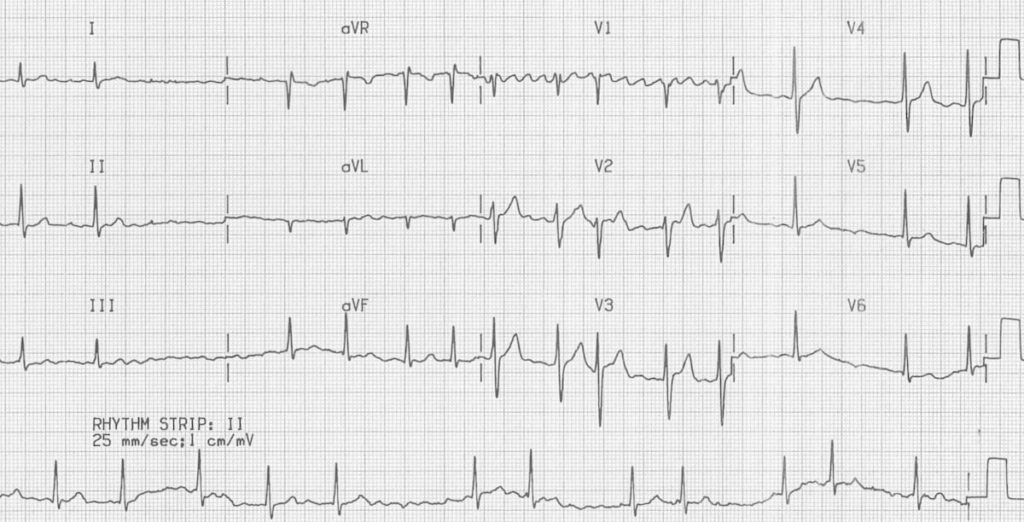
Example 5
AF with slow ventricular response
- Irregular heart rate with no evidence of organised atrial activity
- Fine fibrillatory waves in V1
- ST depression / T wave inversion in the lateral leads could represent ischaemia or digoxin effect
- The slow ventricular rate suggests that the patient is being treated with an AV-nodal blocking drug (e.g. beta-blocker, verapamil/diltiazem, digoxin). Another cause of slow AF is hypothermia
Example 6
There are two aberrantly conducted complexes — each follows a long RR / short RR cycle (= Ashman phenomenon).
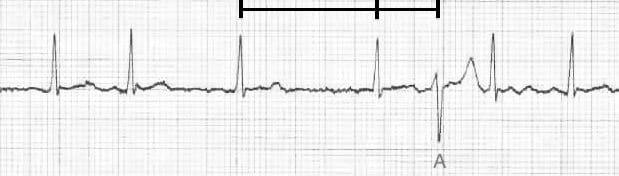
- Atrial flutter
- Ashman Phenomenon (1947) with Prof Richard Ashman
References
- Wiesbauer F. Atrial Fibrillation Management Essentials. Medmastery
- ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006 Aug 15;114(7):e257-354.
- Medi C, Hankey GJ, Freedman SB. Atrial fibrillation. Med J Aust. 2007 Feb 19;186(4):197-202
- Medi C, Hankey GJ, Freedman SB. Stroke risk and antithrombotic strategies in atrial fibrillation. Stroke. 2010 Nov;41(11):2705-13
- Kezerashvili A, Krumerman AK, Fisher JD. Sinus Node Dysfunction in Atrial Fibrillation: Cause or Effect? J Atr Fibrillation. 2008 Sep 16;1(3):30
- Stiell IG, Macle L; CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011 Jan-Feb;27(1):38-46; 47-59
- Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010 Oct;12(10):1360-420
- 2011 ACCF/AHA/HRS Focused Update on the Management of Patients With Atrial Fibrillation (Updating the 2006 Guideline) A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011, 123:104-123
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


How can sinus node dysfunction cause slow AF???? Think it through…..