Abdominal CT: aortic aneurysm
Detecting a rupturing abdominal aortic aneurysm
An abdominal aortic aneurysm (AAA) is an abnormal bulging of the abdominal aorta which can pose a risk for bursting (i.e., rupture) over time. A rupturing abdominal aortic aneurysm is a vascular surgical emergency and requires urgent diagnosis with clear communication of the findings to direct patient care.
Patients with an AAA might present with abdominal pain, hypotension, or pulsating abdominal mass. In many cases, the diagnosis of an AAA is unexpected as it mimics other, more common causes of abdominal pain.
Key findings
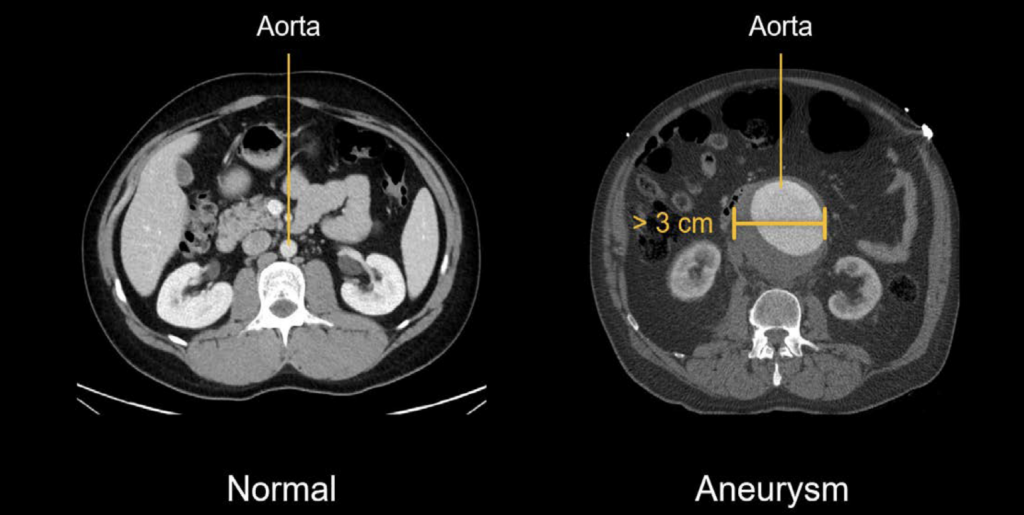
The diagnosis of AAA is made when the maximum diameter of the abdominal aorta is greater than 3 cm. However, aneurysms smaller than 5 cm do not pose a significant risk of rupture. Rupture becomes a greater concern for aneurysms that are larger than 5 cm and for growing aneurysms.
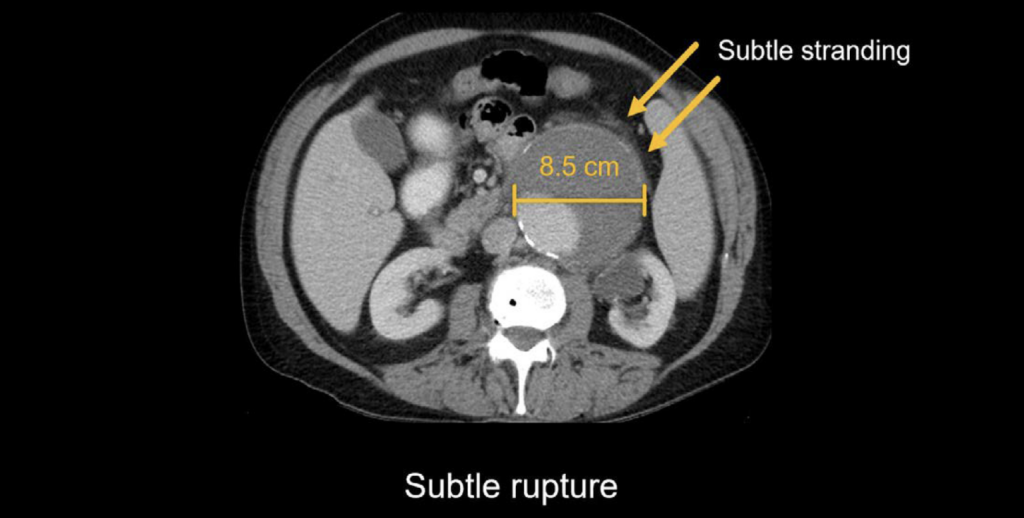
When an aneurysm ruptures, it can be relatively subtle (resulting in blood slowly leaking from the aneurysm sac) or it can be dramatic (resulting in a large amount of blood surrounding the aorta). Subtle ruptured AAA In the case below, we can see a large aneurysm of the abdominal aorta measuring 8.5 cm with only subtle surrounding stranding, which indicates an early or slow rupture. Even though there is not a lot of blood leaking, this is still a surgical emergency.
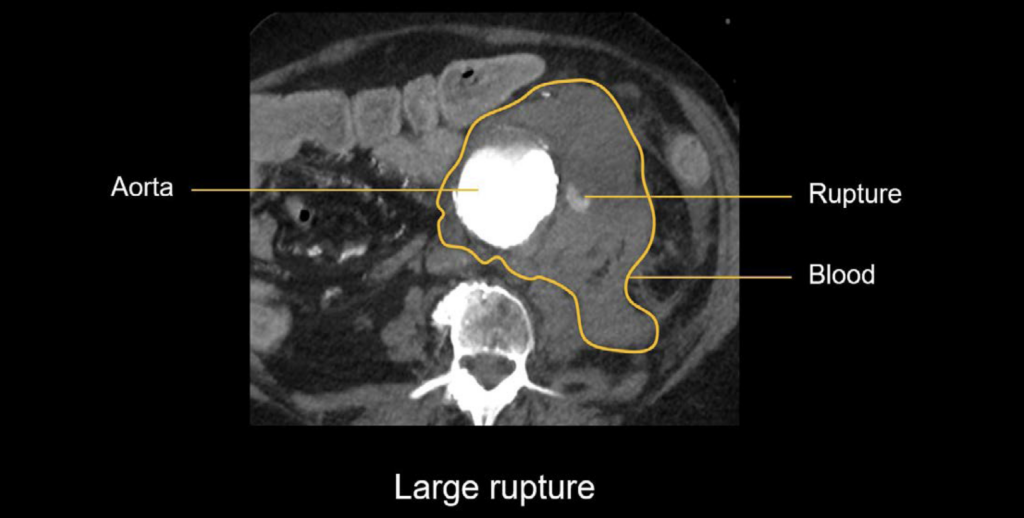
Large ruptured AAA
In the CT angiogram image below, the aorta is very bright with contrast. There is a large, irregular aneurysm with extensive bleeding around the aorta, and you can even see blood actively leaking out from the area of the rupture. This indicates a very poor prognosis for the patient.
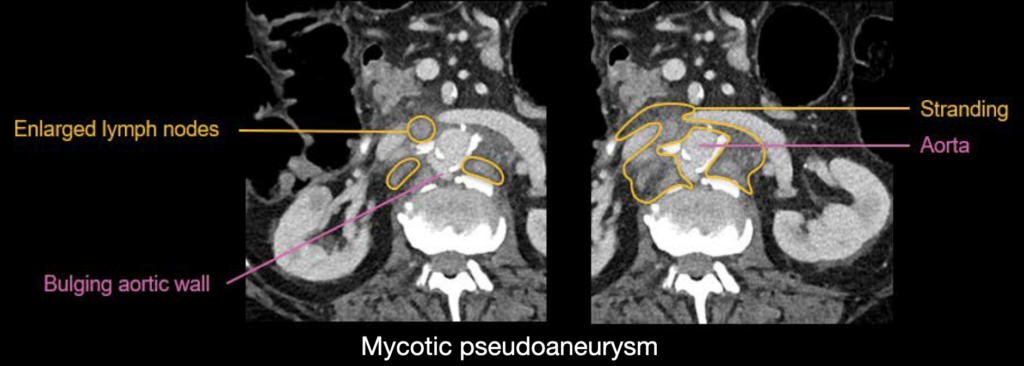
Mycotic pseudoaneurysm
While smoking, advanced age, and atherosclerosis are important risk factors for forming an AAA, these aneurysms can also form due to infection of the arterial wall (from the spread of infection in the blood). This is called a mycotic aneurysm, and it causes a false aneurysm to form. Mycotic aneurysms are at high risk of rupture even if they are relatively small in size.
Example 1
Relatively subtle bulging of the posterior aortic wall. This is called a mycotic pseudoaneurysm or infected pseudoaneurysm. There is inflammatory stranding and enlarged lymph nodes surrounding the aorta. The patient has positive blood cultures for bacterial infection, which support this diagnosis.
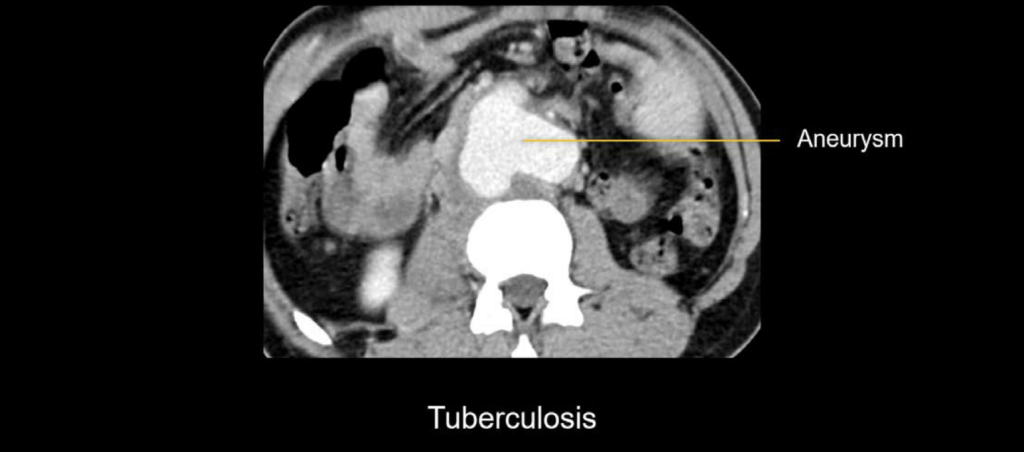
Example 2
The aneurysm has an irregular, bilobed shape with areas of wall thickening. This is not a typical shape for an AAA. In this case, the patient was young and was recently diagnosed with tuberculosis, which led to the diagnosis of a tuberculous mycotic aneurysm. This aneurysm required surgical repair to prevent rupture.
Look for an AAA even if you don’t suspect it!
The clinical presentation of a patient with a rupturing AAA often mimics other causes of abdominal pain such as diverticulitis or renal stones. Thus, you should be prepared to make this diagnosis even when you’re not expecting it, as the study ordered is not a conventional CT angiography.
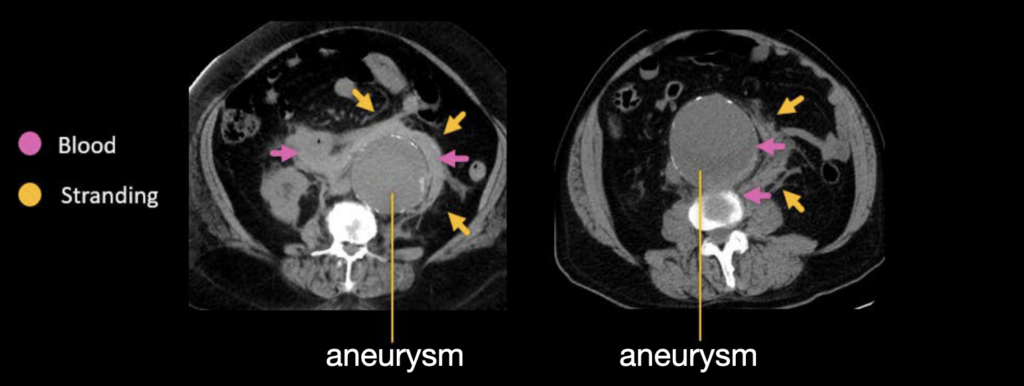
Examples 3 and 4
In both cases the patients presented with pain that was thought to be caused by renal stones, and a non-contrast flank pain CT was ordered. However, instead of renal stones, both patients had very large rupturing abdominal aortic aneurysms!
The case on the left has a large amount of blood surrounding the aorta with some stranding, while the case on the right is relatively subtle with only small amounts of blood and stranding along the lateral side of the aorta.
Knowledge iteration
Let’s reinforce these concepts by reviewing cases of both subtle and obvious rupture
Case 1
Scroll through the images in the online PACS viewer of this subtle case
- You can immediately notice the very large size of the AAA, which measures about 8 cm in diameter. It has a large, rounded appearance which projects out from the aorta.
- You can also see atherosclerotic calcifications on the aortic wall.
- There is relatively subtle haziness due to stranding surrounding the aorta, which perhaps is more apparent on the coronal images. This haziness is due to a slow leakage of blood products, indicating an early rupture. This is a surgical emergency.
Case 2
Scroll through the images in the online PACS viewer of this more dramatic presentation of rupture
- Notice the large AAA.
- This time you can see blood products distributing throughout the retroperitoneum, displacing surrounding structures.
- You can see the site of rupture along the posterior side of the aorta where there is an irregular false aneurysm (i.e., pseudoaneurysm) extending beyond the margin of the aneurysm sac.
- You can also see that there has been bleeding and thickening of the vessel wall due to injury.
This is an edited excerpt from the Medmastery course Abdominal CT Pathologies by Michael P. Hartung, MD. Acknowledgement and attribution to Medmastery for providing course transcripts
- Hartung MP. Abdominal CT: Common Pathologies. Medmastery
- Hartung MP. Abdominal CT: Essentials. Medmastery
- Hartung MP. Abdomen CT: Trauma. Medmastery
References
- Top 100 CT scan quiz. LITFL
- Rippey J. Ultrasound Case 049. LITFL
Radiology Library: Acute abdomen. Solid organ and Vascular pathology
- Hartung MP. Abdominal CT: acute interstitial pancreatitis
- Hartung MP. Abdominal CT: acute necrotizing pancreatitis
- Hartung MP. Abdominal CT: renal stones and the flank pain CT
- Hartung MP. Abdominal CT: renal infections
- Hartung MP. Abdominal CT: cholecystitis
- Hartung MP. Abdominal CT: intestinal ischaemia
- Hartung MP. Abdominal CT: rupturing abdominal aortic aneurysm
Abdominal CT interpretation
Assistant Professor of Abdominal Imaging and Intervention at the University of Wisconsin Madison School of Medicine and Public Health. Interests include resident and medical student education, incorporating the latest technology for teaching radiology. I am also active as a volunteer teleradiologist for hospitals in Peru and Kenya. | Medmastery | Radiopaedia | Website | Twitter | LinkedIn | Scopus
MBChB (hons), BMedSci - University of Edinburgh. Living the good life in emergency medicine down under. Interested in medical imaging and physiology. Love hiking, cycling and the great outdoors.


