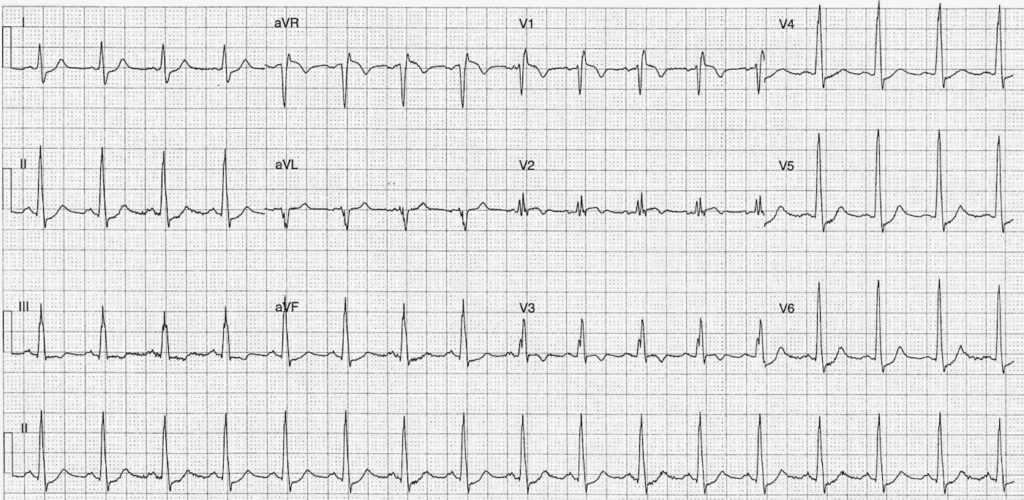
ECG Case 104
This ECG is from a 47 year old female. She presents with acute onset severe dyspnoea.
Her vitals signs are BP 95/42; RR 30; sats 88% (room air)
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
Rate:
- 102
Rhythm:
- Regular
- Sinus Rhythm
Axis:
- Normal (~80 deg)
Intervals:
- PR – Normal (~160ms)
- QRS – Prolonged (100-120ms)
- QT – 320ms (QTc Bazett ~410 ms)
Segments:
- ST Elevation leads aVR (1.5mm) V1 (1mm) V2 (subtle)
- ST Depression Leads I, II, III, V4, V5, V6
Additional:
- T wave inversion leads III, aVR, V1, V2, V3
- S wave lead I
- Small Q waves (<1mm) leads II, III, aVF
- RSR’ pattern V1, V2
- Partial / Complete RBBB – QRS varies 100-120ms
Interpretation:
- The ECG findings really suggest two likely pathologies:
- Pulmonary Embolism
- ACS
- With this clinical stem of hypoxia, hypotension, and pre-syncope I’d argue PE is more likely than ACS
CLINICAL PEARLS
Does the ECG help us in PE ?
The ECG in Pulmonary Embolism ultimately lacks sensitivity and specificity. Its most important role is the detection of another cause for the patients symptoms e.g. ACS or STEMI.
Some ECG features that are associated with PE are:
- Normal ECG in 9-26% of cases
- Sinus Tachycardia in 44-73% of cases
- RBBB (Complete or incomplete) in 18-25% of cases
- RAD in 16-23% of cases
- P pulmonale in 9-33% of cases
- Supraventricular arrhythmia in 8-33% of cases
- Clockwise rotation in 18-30% of cases
- T inversion Right Precordial leads in 10-46% of cases
- S1Q3T3 in 12-25% of cases
- S1Q3T3 whilst oft quoted as ‘the’ ECG finding in PE lacks sensitivity, specificity, and is certainly not pathognomonic of PE.
The incidence of the ECG changes in PE vary greatly between sources. further review over at
ACS vs PE
Dr Smith has already done the work for me on this one, with a great case example, and a reference to an article by Kosuge et al. Head over to Dr Smith’s blog post and read the Kosuge et al. paper.
The presence of T wave inversion in lead V1 plus lead III, as in our case here, was only seen in 1% of ACS patients versus 88% of patients with Acute Pulmonary Embolism (n=87 in ACS group, n=40 in PE group).
For a great review of the ACS vs PE issues check out the Chart Review post on ‘A Clear cut case of ACS‘
CLINICAL OUTCOME
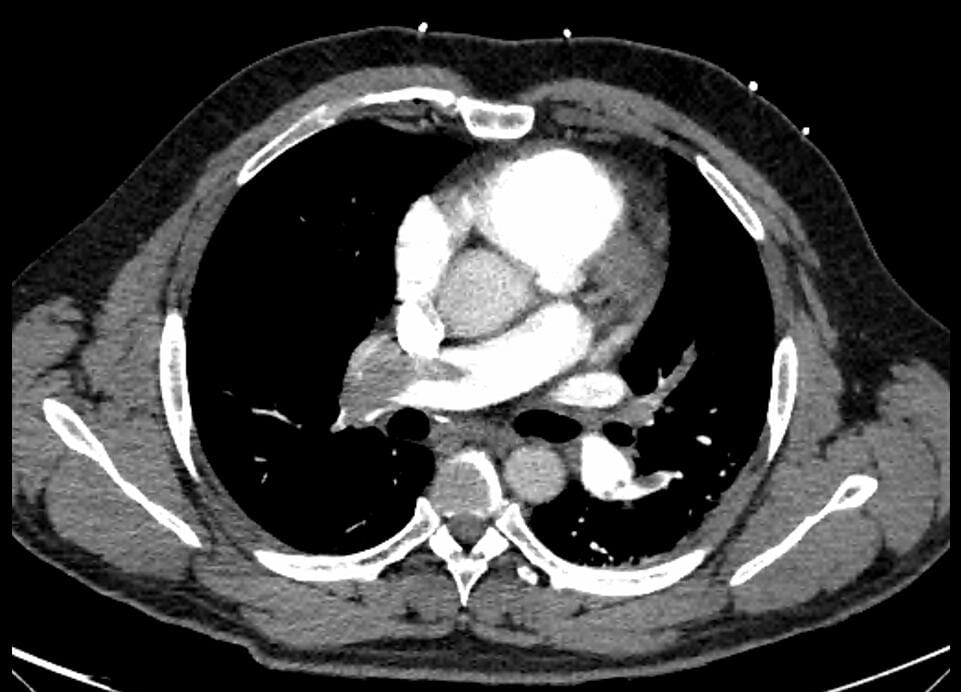
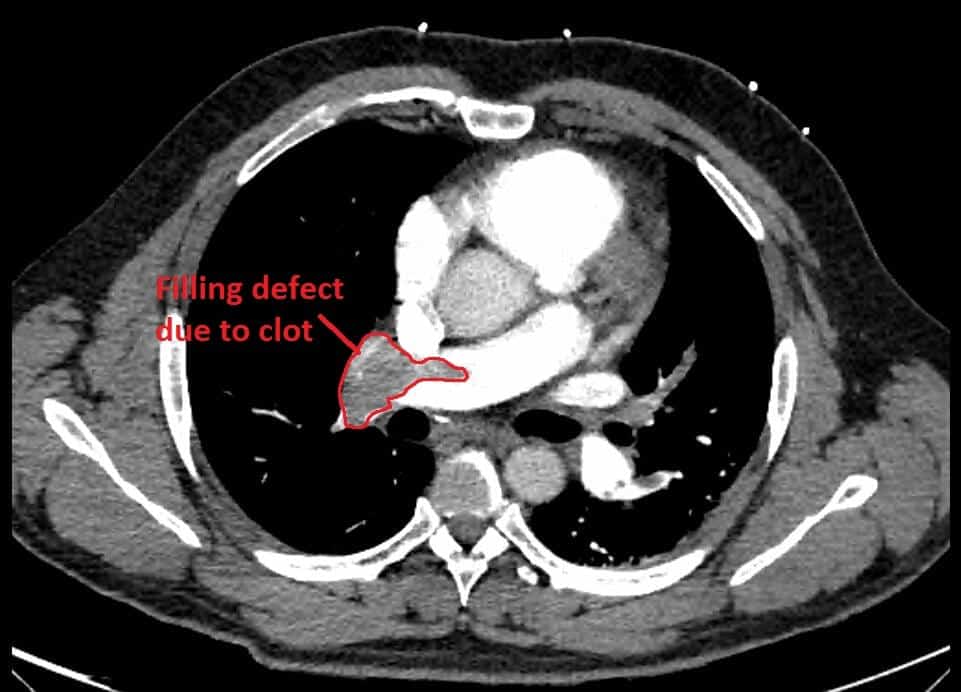
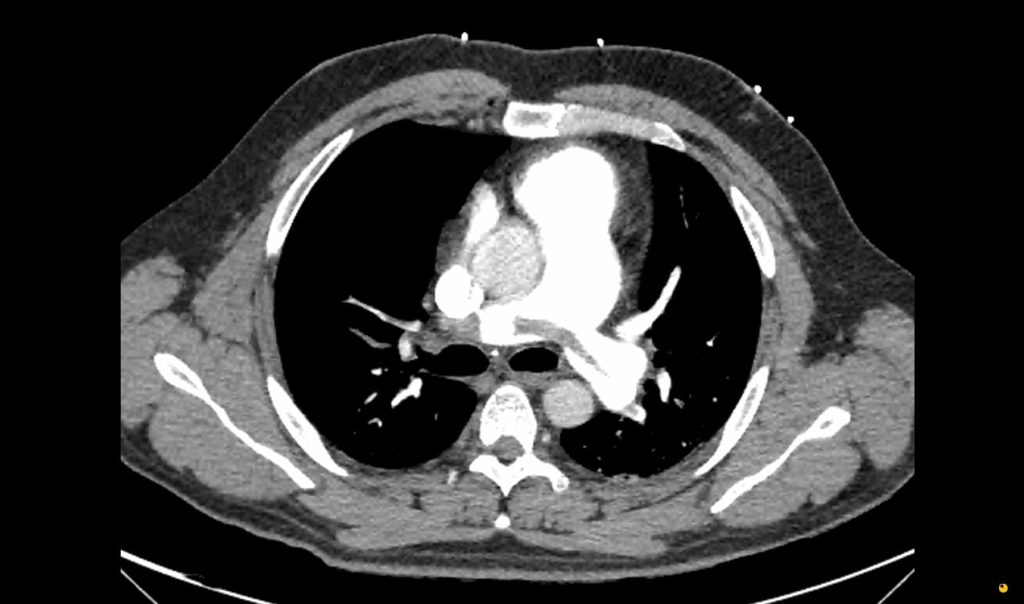
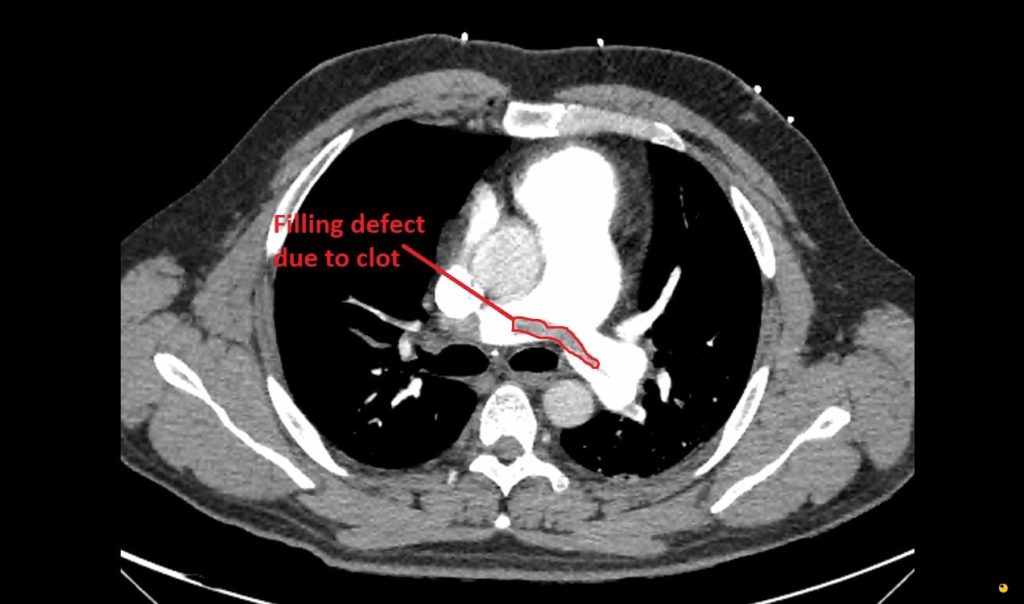
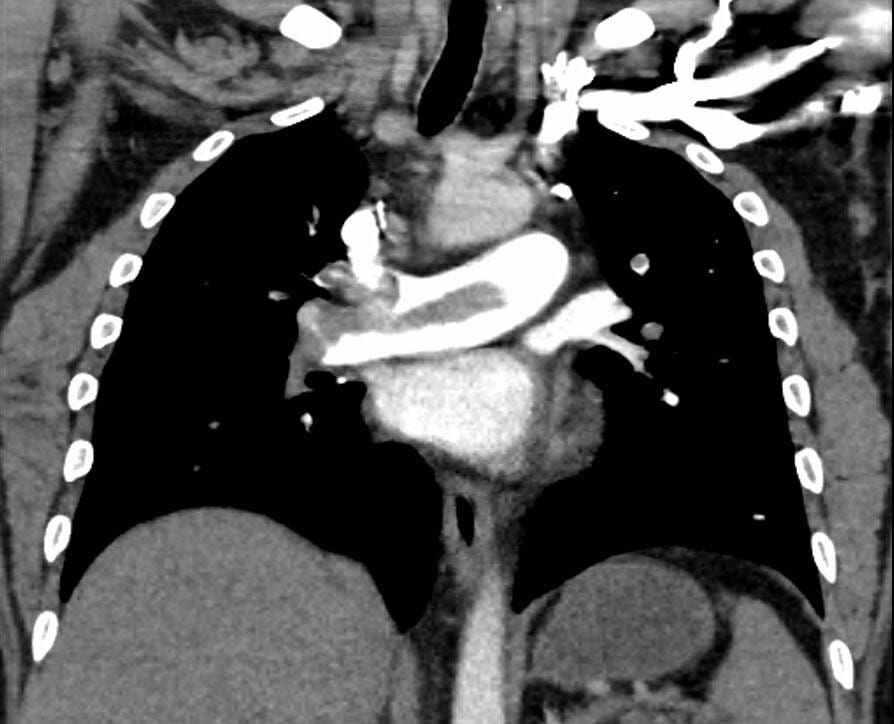
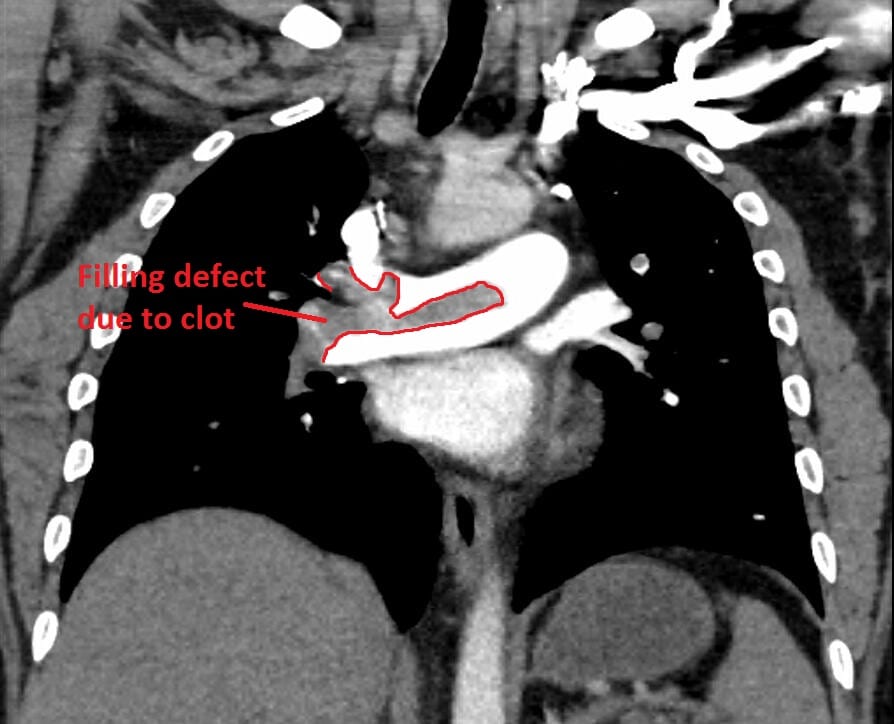
Here is the CXR and CTPA of this case. Check out CXR in PE for a great overview on the CXR features of PE
Formal CTPA report: Saddle pulmonary embolism is noted. Heavy bilateral thrombus burden. There is CT evidence for right heart strain.
If you want to read more about CTPA and its role/limitations in PE severity assessment check out this article by Ghaye et al.
Our patient was then transferred to a Tertiary Centre and underwent a successful pulmonary embolectomy and was discharged from hospital within a week.
FURTHER READING
TOP 150 ECG Series
Emergency Medicine Specialist MBChB FRCEM FACEM. Medical Education, Cardiology and Web Based Resources | @jjlarkin78 | LinkedIn |