Right Ventricular Outflow Tract Tachycardia
Overview
Right ventricular outflow tract (RVOT) tachycardia is a form of monomorphic VT originating from the outflow tract of the right ventricle or occasionally from the tricuspid annulus. It is usually seen in patients without underlying structural heart disease.
The majority (80%) of outflow tract ventricular arrhythmias (OTVAs) originate from the RVOT. The RVOT is divided into rightward (free wall), anterior, leftward, and posterior (septal) parts. RVOT VT can originate from any of these sites but carry common ECG characteristics.
ECG features
- LBBB morphology
- Inferior axis
- rS complex in V1 and R complex in V6
- Precordial transition usually ≥ V3, with the exception of septal origin, which occurs at ≤ V3
Other general features of VT, such as AV dissociation, fusion and/or capture beats may also be present.
Causes
Idiopathic VT
RVOT tachycardia is most commonly a form of idiopathic VT, whereby no structural heart disease, metabolic/electrolyte abnormalities, or long QT syndrome can be found. There are two main forms of clinical presentation:
- Repetitive, unsustained, monomorphic VT is the most common form seen in 60-90%
- Exercise-induced sustained ventricular arrhythmias
Arrhythmogenic Right Ventricular Dysplasia (ARVD)
ARVD is a genetic disorder of myocardium in which there is fatty infiltration of the right ventricular free wall, and accounts for up to 10% of sudden cardiac death in individuals under 65 years of age. Affected individuals often present with exercise-induced episodes of VT accompanied by LBBB morphology.
Differentiation between idiopathic RVOT tachycardia and that caused by ARVD can be difficult and may rely on previous ECG findings as well as family history.
Clinical implications
- RVOT tachycardia can be difficult to distinguish from SVT with LBBB
- Inferior axis (+90 degrees) is usually the most differentiating feature, but other features of VT such as AV dissociation may be present
Treatment:
- Acute termination of idiopathic RVOT tachycardia in a stable patient can be achieved by vagal manoeuvres or adenosine (6mg up to 24mg)
- IV verapamil is an alternative if the patient has an adequate blood pressure reserve
- RVOT tachycardia in ARVD does not terminate with adenosine
In stable patients with a regular broad complex tachycardia, adenosine is useful and safe as a diagnostic and potentially therapeutic agent.
In unstable patients, if there is doubt regarding the rhythm (SVT v VT), proceed to DCCV
Example ECGs
Example 1
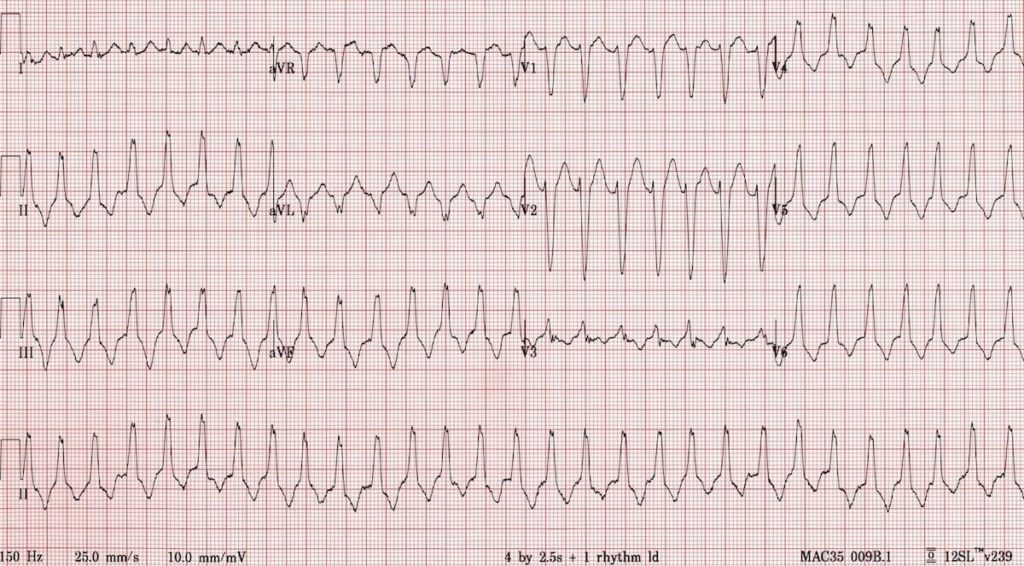
RVOT tachycardia:
- Regular broad complex tachycardia
- LBBB-like morphology with rS complex in V1 and R complex in V6
- Precordial transition at V3
- Inferior axis (+ 90 degrees)
Example 2
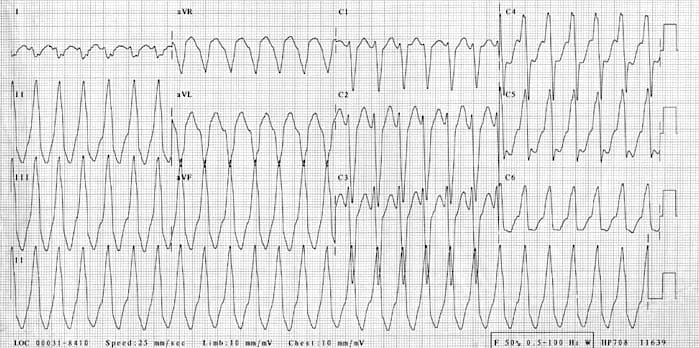
RVOT tachycardia:
- Regular broad complex tachycardia
- LBBB-like morphology with rS complex in V1 and R complex in V6
- Precordial transition at V4
- Inferior axis (+ 90 degrees)
Video Lessons
Professor Sanjay Sharma discusses Right Ventricular VT in ARVD.
Related Topics
- Ventricular tachycardia
- Arrhythmogenic Right Ventricular Dysplasia
- ECG Exigency 8 — “Sudden Syncope on the Soccer Field”
References
- Lerman B, Stein KM, Markowitz SM, Mittal S, Slotwiner DJ. Right Ventricular Outflow Tract Tachycardia: An Update. Cardiac Electrophysiology Review. 2002;6, 1-2:68-71
- Brugada J, Diez DP. How to recognise and manage idiopathic ventricular tachycardia. e-Journal of Cardiology Practice 2010; 8(26)
- Bogossian H et al. Spot diagnosis of inferior axis and concordant R-pattern predicts left ventricular inflow tract tachycardia: Ablation from the great cardiac vein of an underdiagnosed entity. Int J Cardiol. 2016 Jul 1;214:175-9.
- Anderson RD et al. Differentiating Right- and Left-Sided Outflow Tract Ventricular Arrhythmias: Classical ECG Signatures and Prediction Algorithms. Circ Arrhythm Electrophysiol. 2019 Jun;12(6):e007392.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner

