Supraventricular Tachycardia (SVT)
Definition
The term supraventricular tachycardia (SVT) refers to any tachydysrhythmia arising from above the level of the Bundle of His, and encompasses regular atrial, irregular atrial, and regular atrioventricular tachycardias
- It is often used synonymously with AV nodal re-entry tachycardia (AVNRT), a form of SVT
- In the absence of aberrant conduction (e.g. bundle branch block), the ECG will demonstrate a narrow complex tachycardia
- Paroxysmal SVT (pSVT) describes an SVT with abrupt onset and offset – characteristically seen with re-entrant tachycardias involving the AV node such as AVNRT or atrioventricular re-entry tachycardia (AVRT)
Classification
- SVTs can be classified based on:
- Site of origin (atria or AV node) or;
- Regularity (regular or irregular)
- Classification based on QRS width is unhelpful as this is also influenced by the presence of pre-existing bundle branch block, rate-related aberrant conduction, or presence of accessory pathways.
Classification of SVT by site of origin and regularity
Regular Atrial
- Sinus tachycardia
- Atrial tachycardia
- Atrial flutter
- Inappropriate sinus tachycardia
- Sinus node reentrant tachycardia
Regular Atrioventricular
AV Nodal Re-entry Tachycardia (AVNRT)
- This is the commonest cause of palpitations in patients with structurally normal hearts
- AVNRT is typically paroxysmal and may occur spontaneously or upon provocation with exertion, caffeine, alcohol, beta-agonists (salbutamol) or sympathomimetics (amphetamines)
- It is more common in women than men (~ 75% of cases occurring in women) and may occur in young and healthy patients as well as those suffering chronic heart disease
- Patients will typically complain of the sudden onset of rapid, regular palpitations. Other associated symptoms may include:
- Presyncope or syncope due to a transient fall in blood pressure
- Chest pain, especially in the context of underlying coronary artery disease
- Dyspnoea
- Anxiety
- Rarely, polyuria due to elevated atrial pressures causing release of atrial natriuretic peptide
- The tachycardia typically ranges between 140-280 bpm and is regular in nature. It may self-resolve or continue indefinitely until medical treatment is sought
- The condition is generally well tolerated and is rarely life threatening in patients with pre-existing heart disease
Pathophysiology
In comparison to AVRT, which involves an anatomical re-entry circuit (Bundle of Kent), in AVNRT there is a functional re-entry circuit within the AV node.
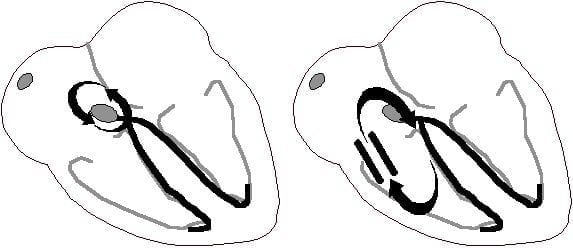
Alrternate re-entry loops: Functional circuit in AVNRT (left), anatomical circuit in AVRT (right)
Functional pathways within the AV node
There are two pathways within the AV node:
- The slow pathway (alpha): a slowly-conducting pathway with a short refractory period.
- The fast pathway (beta): a rapidly-conducting pathway with a long refractory period.
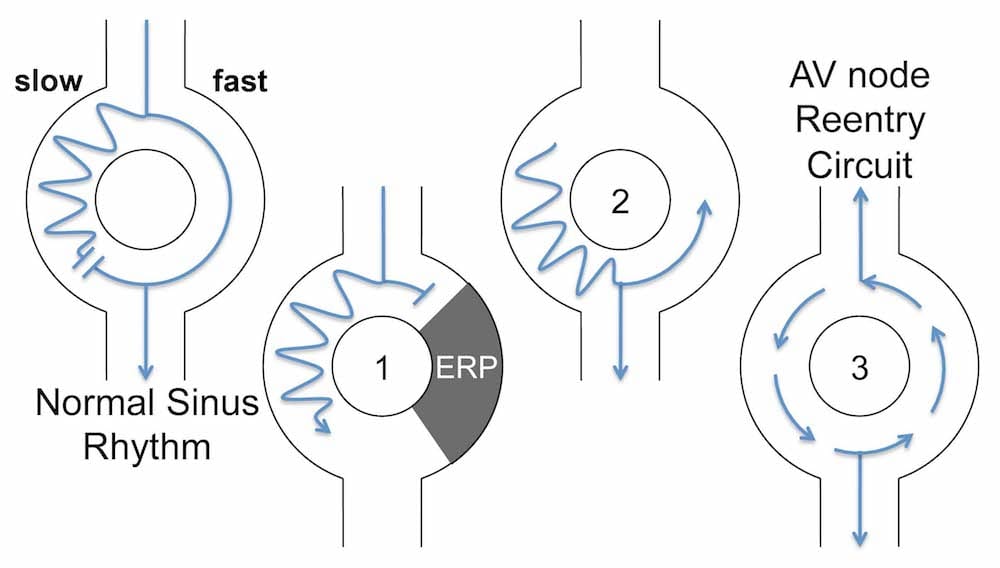
1) A premature atrial contraction (PAC) arrives while the fast pathway is still refractory, and is directed down the slow pathway
2) The ERP in the fast pathway ends, and the PAC impulse travels retrogradely up the fast pathway
3) The impulse continually cycles around the two pathways
Initiation of re-entry
- During normal sinus rhythm, electrical impulses travel down both pathways simultaneously. The impulse transmitted down the fast pathway enters the distal end of the slow pathway and the two impulses cancel each other out
- However, if a premature atrial contraction (PAC) arrives while the fast pathway is still refractory, the electrical impulse will be directed solely down the slow pathway (1)
- By the time the premature impulse reaches the end of the slow pathway, the fast pathway is no longer refractory, and the impulse is permitted to recycle retrogradely up the fast pathway (2)
- This creates a circus movement whereby the impulse continually cycles around the two pathways, activating the Bundle of His anterogradely and the atria retrogradely (3)
- The short cycle length is responsible for the rapid heart rate
- This most common type of re-entrant circuit is termed Slow-Fast AVNRT
- Similar mechanisms exist for the other types of AVNRT
Electrocardiographic Features
ECG features of AVNRT
- Regular tachycardia ~140-280 bpm
- Narrow QRS complexes (< 120ms) unless there is co-existing bundle branch block, accessory pathway, or rate-related aberrant conduction
- P waves if visible exhibit retrograde conduction with P-wave inversion in leads II, III, aVF. They may be buried within, visible after, or very rarely visible before the QRS complex
Associated features include:
- Rate-related ST depression, which may be seen with or without underlying coronary artery disease
- QRS alternans – phasic variation in QRS amplitude associated with AVNRT and AVRT, distinguished from electrical alternans by a normal QRS amplitude
Subtypes of AVNRT
Different subtypes vary in terms of the dominant pathway, and the R-P interval, which is the time between anterograde ventricular activation (R wave) and retrograde atrial activation (P wave).
- Slow-Fast AVNRT (80-90%)
- Fast-Slow AVNRT (10%)
- Slow-Slow AVNRT (1-5%)
1. Slow-Fast AVNRT (common type)
- Accounts for 80-90% of AVNRT
- Associated with slow AV nodal pathway for anterograde conduction and fast AV nodal pathway for retrograde conduction
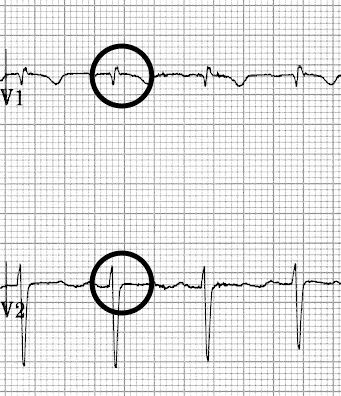
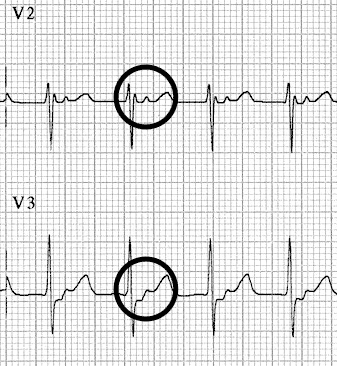
- The retrograde P wave is obscured in the corresponding QRS or occurs at the end of the QRS complex as pseudo R’ or S waves
ECG features:
- P waves are often hidden – being embedded in the QRS complexes
- Pseudo R’ wave may be seen in V1 or V2
- Pseudo S waves may be seen in leads II, III or aVF
- In most cases this results in a ‘typical’ SVT appearance with absent P waves and tachycardia
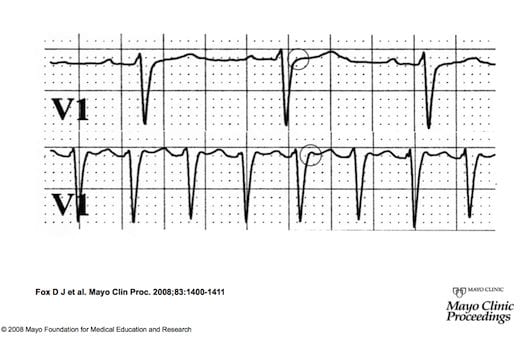
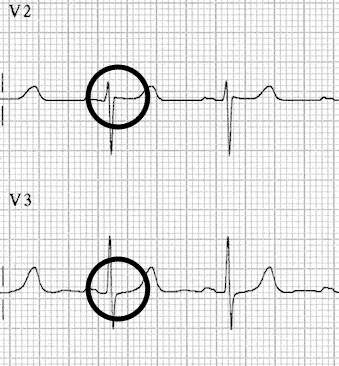
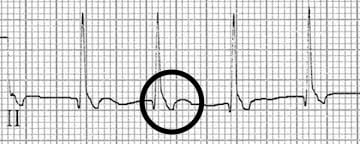
Bottom strip: Paroxysmal SVT. The P wave is seen as a pseudo-R wave (circled) in lead V1 during tachycardia. This very short ventriculo-atrial time is frequently seen in typical Slow-Fast AVNRT
2. Fast-Slow AVNRT (Uncommon AVNRT)
- Accounts for 10% of AVNRT
- Associated with Fast AV nodal pathway for anterograde conduction and Slow AV nodal pathway for retrograde conduction
- Due to the relatively long ventriculo-atrial interval, the retrograde P wave is more likely to be visible after the corresponding QRS
ECG features:
- QRS-P-T complexes
- Retrograde P waves are visible between the QRS and T wave
3. Slow-Slow AVNRT (Atypical AVNRT)
- 1-5% AVNRT
- Associated with Slow AV nodal pathway for anterograde conduction and Slow left atrial fibres as the pathway for retrograde conduction.
ECG features:
- Tachycardia with a P-wave seen in mid-diastole, effectively appearing “before” the QRS complex.
- May be misinterpreted as sinus tachycardia
Summary of AVNRT subtypes
- No visible P waves? –> Slow-Fast
- P waves visible after the QRS complexes? –> Fast-Slow
- P waves visible before the QRS complexes? –> Slow-Slow
Management of AVNRT
- May respond to vagal maneuvers with reversion to sinus rhythm.
- The mainstay of treatment is adenosine
- Other agents which may be used include calcium-channel blockers, beta-blockers and amiodarone
- DC cardioversion is rarely required
- Catheter ablation may be considered in recurrent episodes not amenable to medical treatment.
Other types of SVT
Most other types of SVT are discussed elsewhere (follow links in classification table). Two less common types include:
Inappropriate Sinus Tachycardia
- Typically seen in young healthy female adults
- Sinus rate persistently elevated above 100 bpm in absence of physiological stressor
- Exaggerated rate response to minimal exercise
- ECG indistinguishable from sinus tachycardia
Sinus Node Reentrant Tachycardia (SNRT)
- Caused by reentry circuit close to or within the sinus node
- Abrupt onset and termination
- P wave morphology is normal
- Rate usually 100 – 150 bpm
- May terminate with vagal manoeuvres
ECG Examples
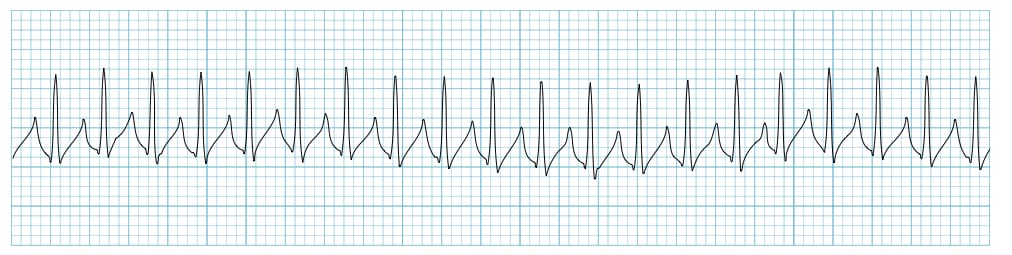
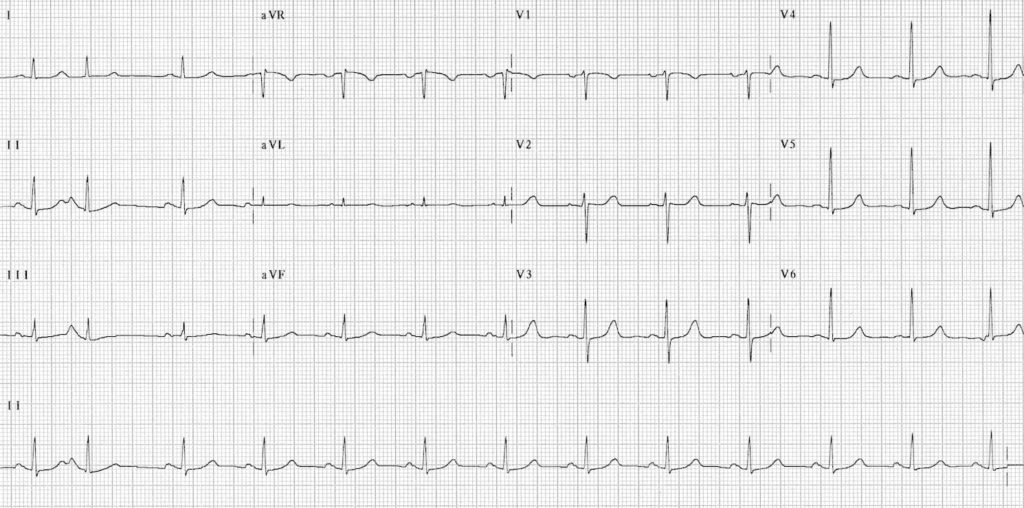
Example 1a
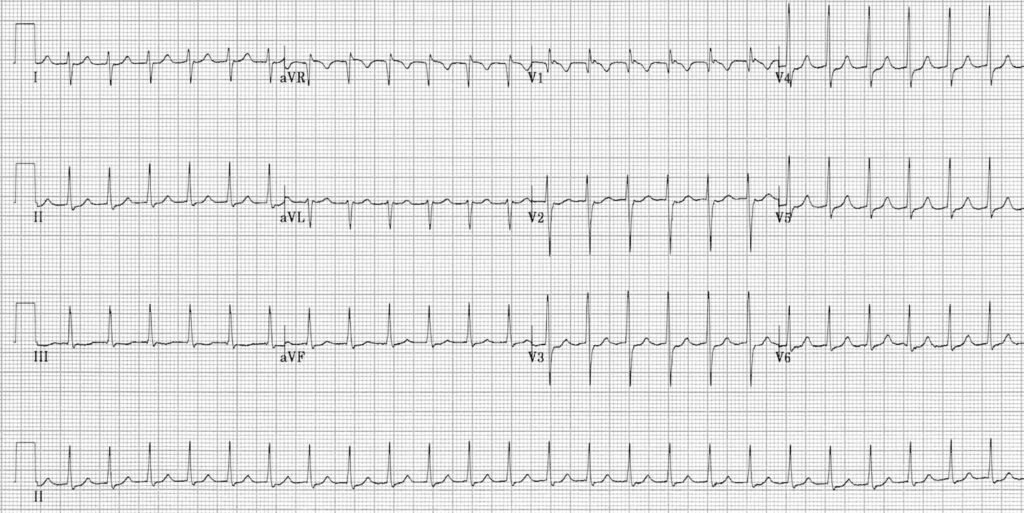
Slow-Fast (Typical) AVNRT:
- Narrow complex tachycardia at ~ 150 bpm
- No visible P waves
- There are pseudo R’ waves in V1-2

Example 1b
The same patient following resolution of the AVNRT:
- Sinus rhythm
- The pseudo R’ waves have now disappeared
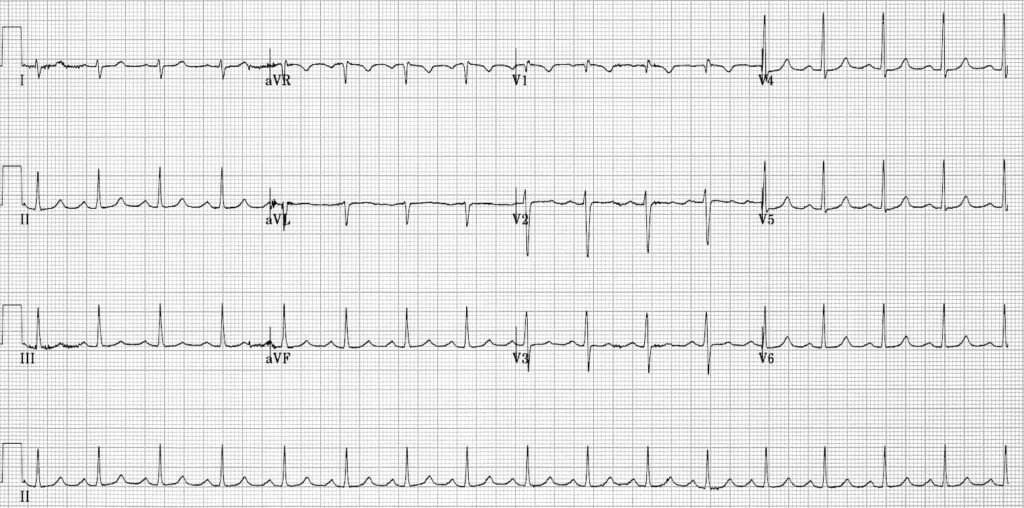
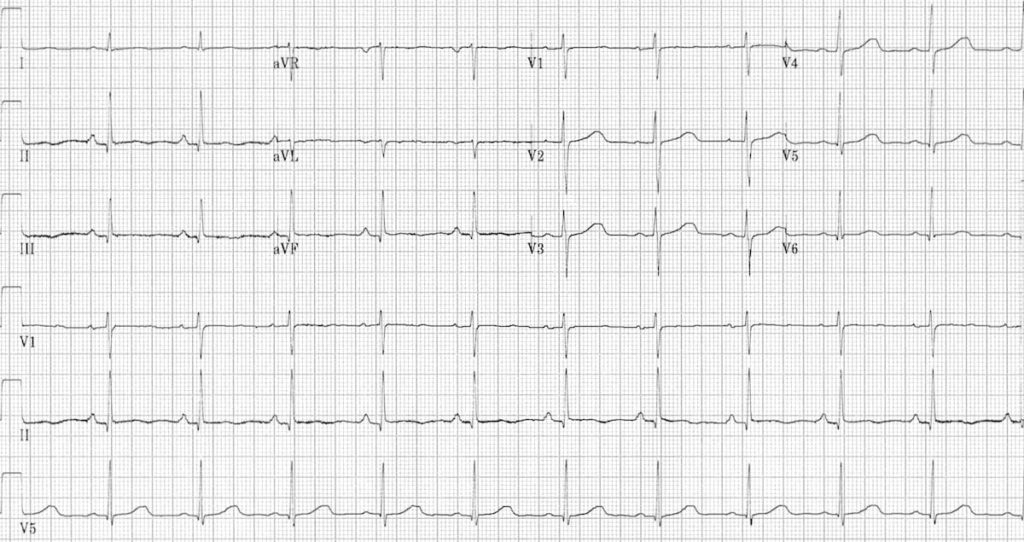
Example 2a
Slow-Fast AVNRT:
- Narrow complex tachycardia ~ 220 bpm
- No visible P waves
- Subtle notching of the terminal QRS in V1 (= pseudo R’ wave)
- Widespread ST depression — this is a common electrocardiographic finding in AVNRT and does not necessarily indicate myocardial ischaemia, provided the changes resolve once the patient is in sinus rhythm
Example 2b
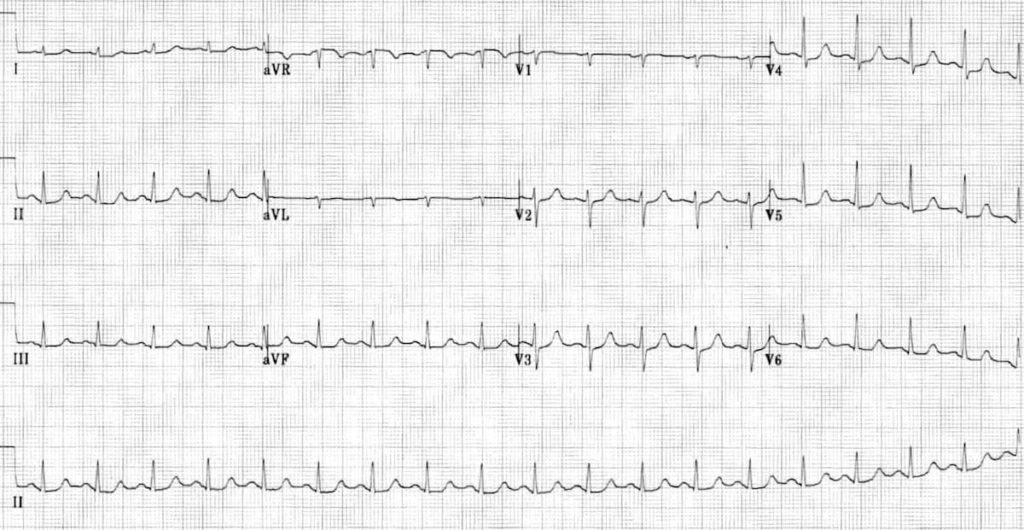
The same patient following resolution of the AVNRT:
- Sinus rhythm
- Pseudo R’ waves have disappeared
- There is residual ST depression in the inferior and lateral leads (most evident in V4-6), indicating that the patient did indeed have rate-related myocardial ischaemia (± NSTEMI)
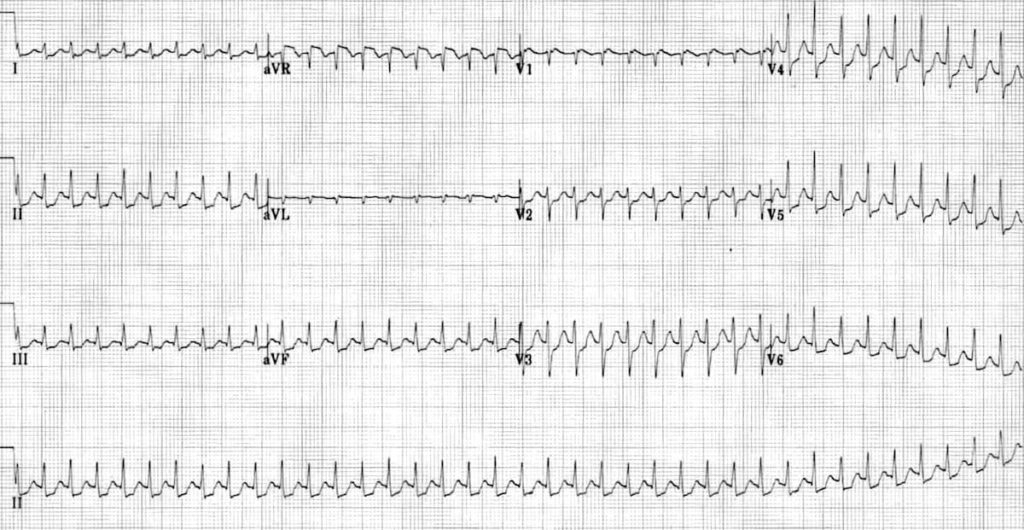
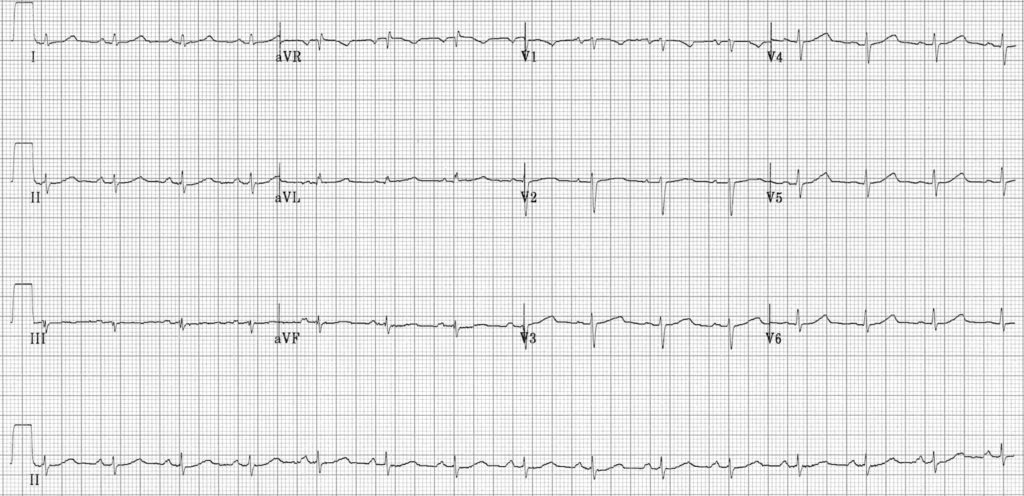
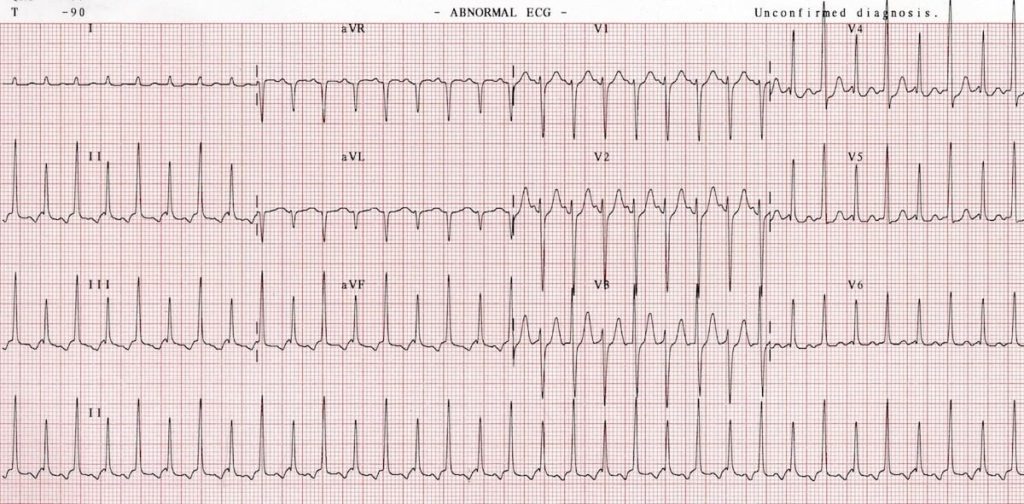
Example 3
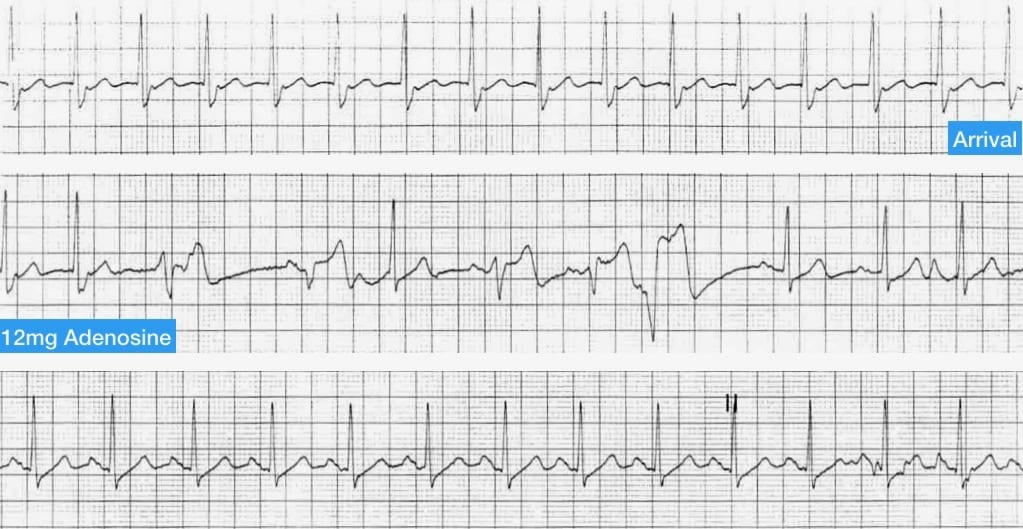
Patient with Slow-Fast AVNRT undergoing treatment with adenosine:
- The top rhythm strip shows AVNRT with absent P waves and pseudo R’ waves clearly visible
- The middle strip shows adenosine acting on the AV node to suppress AV conduction — there are several broad complex beats which may be aberrantly-conducted supraventricular impulses or ventricular escape beats (this is extremely common during administration of adenosine for AVNRT)
- The bottom section shows reversion to sinus rhythm; the pseudo R’ waves have resolved.
Example 4a
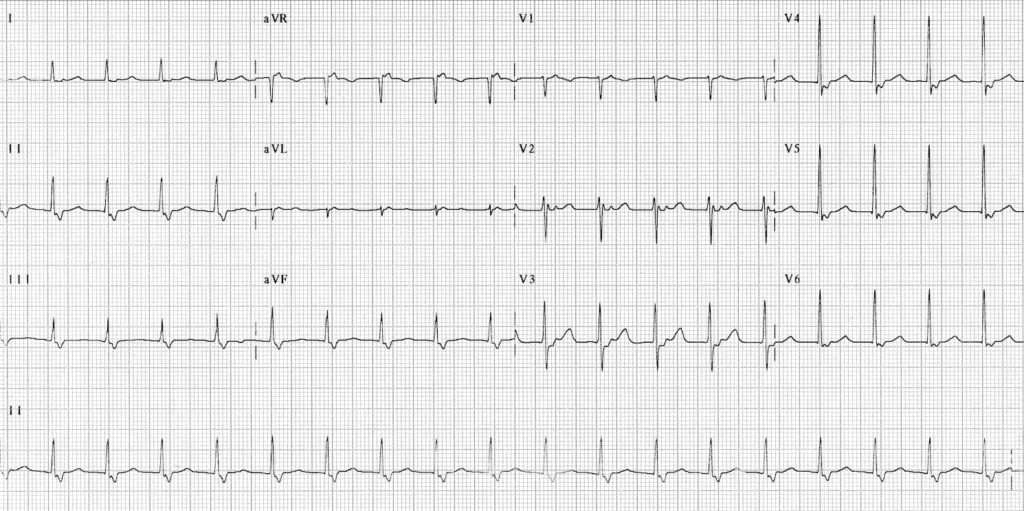
Fast-Slow (Uncommon) AVNRT:
- Narrow complex tachycardia ~ 120 bpm.
- Retrograde P waves are visible after each QRS complex — most evident in V2-3.
Example 4b
The same patient following resolution of the AVNRT:
- Now in sinus rhythm.
- The retrograde P waves have disappeared.
Example 5a

Fast-Slow AVNRT:
- Narrow complex tachycardia ~ 135 bpm.
- Retrograde P waves following each QRS complex — upright in aVR and V1; inverted in II, III and aVL.


Example 5b
The same patient following resolution of the AVNRT:
- Sinus rhythm
- The retrograde P waves have disappeared


Example 6a
Fast-Slow AVNRT:
- Narrow complex tachycardia at ~ 125 bpm
- Retrograde P waves follow each QRS complex: upright in V1-3; inverted in II, III and aVF

Example 6b
The same patient following resolution of the AVNRT:
- Sinus rhythm.
- Retrograde P waves have disappeared.


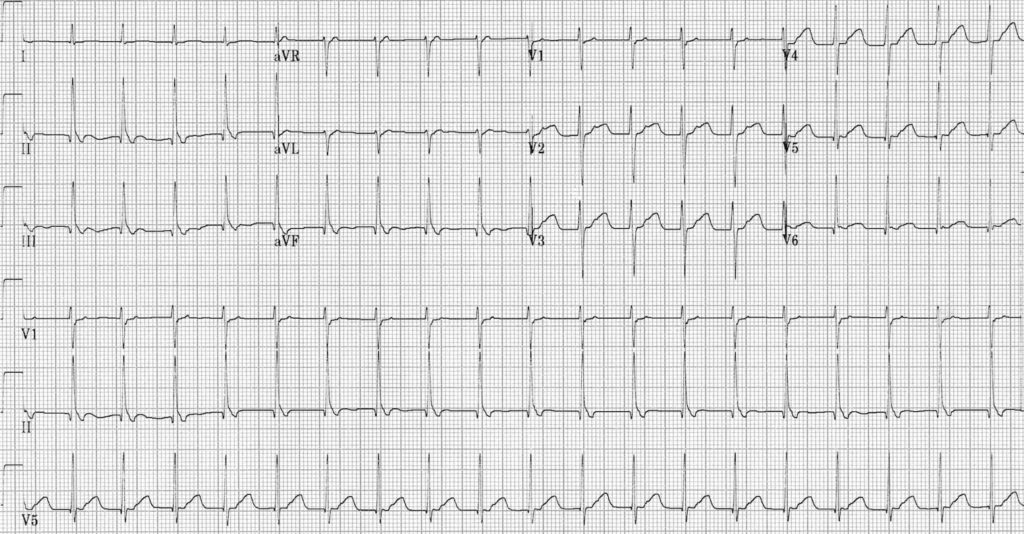
Example 7
SVT with QRS alternans:
- Narrow complex tachycardia ~ 215 bpm
- Retrograde P waves are visible preceding each QRS complex (upright in V1, inverted in lead II)
- There is a beat-to-beat variation in the QRS amplitude without evidence of low voltage (= QRS alternans)
- The PR interval is ~ 120 ms, so this could be either a low atrial tachycardia or possibly an AVNRT with a long RP interval (i.e. either Fast-Slow or Slow-Slow varieties)
Related Topics
- Sinus tachycardia
- Atrial tachycardia
- Atrioventricular re-entry tachycardia (AVRT)
- Atrial flutter
- Atrial fibrillation
- Multifocal atrial tachycardia
- VT versus SVT with aberrancy
References
- Jazayeri MR, Massumi A, Mihalick MJ, Hall RJ. Sinus node reentry: case report and review of electrocardiographic and electrophysiologic features. Tex Heart Inst J. 1985 Sep;12(3):249-52
- Fox DJ, Tischenko A, Krahn AD, Skanes AC, Gula LJ, Yee RK, Klein GJ. Supraventricular tachycardia: diagnosis and management. Mayo Clin Proc. 2008 Dec;83(12):1400-11
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Most useful information I have been looking for, cheers and thumbs up for dr Ed Burns.
Dr Bukhari
FACRRM, MBBS
Dear Ed,
Few conflicting information out there in the lit about treatment of SVT w WPW. I feel safest is to just shock because at that speed, u cant afford to make the error of diagnosising regular vs irregular rhythm. I.e AF w WPW.
Your thoughts please?