Arrhythmogenic Right Ventricular Dysplasia (ARVD)
Overview of ARVD
Autosomal dominant genetic disorder of myocardium in which there is fatty infiltration of the right ventricular free wall, predisposing to paroxysmal ventricular arrhythmias, sudden cardiac death, and biventricular failure
- Second most common cause of sudden cardiac death in young people (after HOCM), accounting for up to 10% of sudden cardiac deaths in patients < 65 yrs of age
- Prevalence ~ 1 in 5000
- Diagnosis is difficult and relies on a combination of clinical, electrocardiographic and radiological features, as defined by the (horribly complicated) 2010 Task Force Criteria
ECG features
- T wave inversion in right precordial leads V1-3, in absence of RBBB (85% of patients)
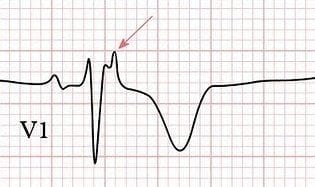
- Epsilon wave (most specific finding, seen in 50% of patients)
- Localised QRS widening in V1-3 (> 110ms)
- Prolonged S wave upstroke of 55ms in V1-3
- Ventricular ectopy of LBBB morphology, with frequent PVCs > 1000 per 24 hours
- Paroxysmal episodes of ventricular tachycardia (VT) with LBBB morphology (RVOT tachycardia)

Note: Some authors recommend recording ECG rhythm strips at double speed (50 mm/second) and double amplitude (20mV/10mm) to enhance the detection of some of these features
Clinical Features
- ARVD causes symptoms due to ventricular ectopic beats or sustained VT (with LBBB morphology), and typically presents with palpitations, syncope or cardiac arrest precipitated by exercise
- The first presenting symptom may be sudden cardiac death
- Over time, surviving patients develop features of right ventricular failure, which may progress to severe biventricular failure and dilated cardiomyopathy
- There is usually a family history of sudden cardiac death
Fontaine leads
Fontaine bipolar precordial leads (F-ECG) are used to increase the sensitivity of epsilon wave detection. Leads are placed as shown:
- Right Arm (RA) over the manubrium;
- Left Arm (LA) over the xiphoid process;
- and Left Leg (LL) in the standard V4 position (5th ICS MCL).
Instead of regular leads I, II, and III, there are now three bipolar chest leads that are termed FI, FII, and FIII. These record potentials developed in the right ventricle, from the infundibulum to the diaphragm.
The vertical bipolar lead FI (similar to aVF) magnifies the atrial potentials and can be used to record:
- Epsilon waves
- Search for AV dissociation in ventricular tachycardia
- Study abnormal atrial rhythms when the P waves are too small on regular leads
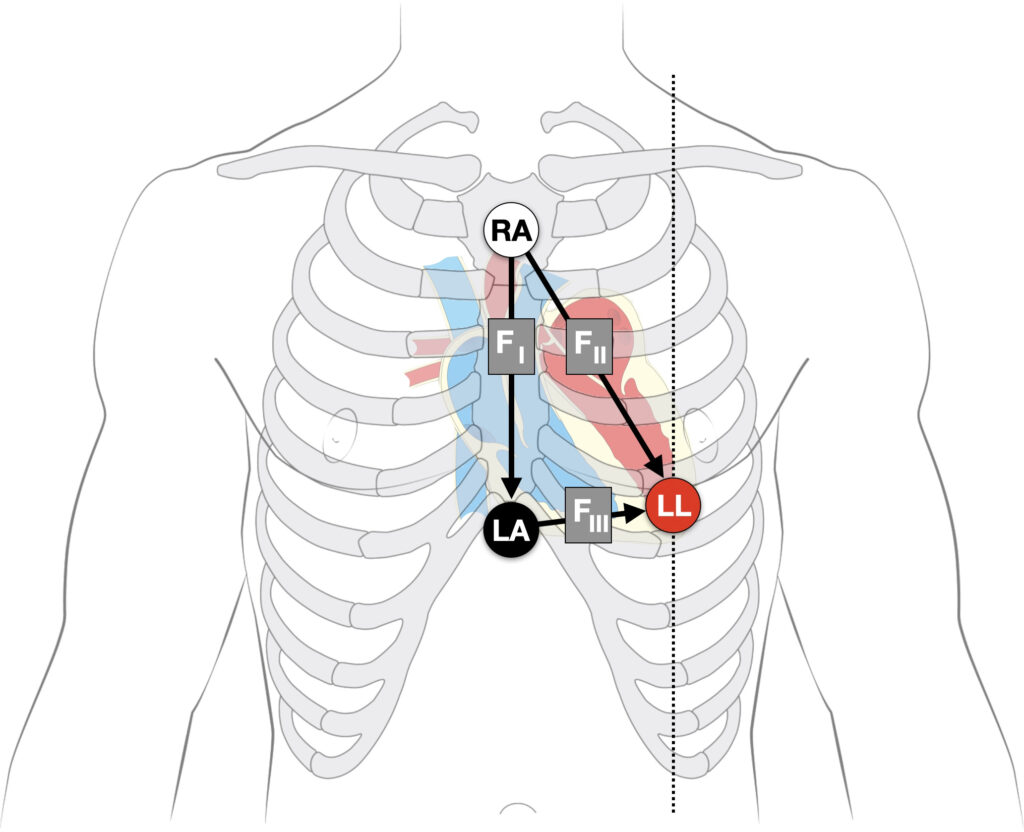
The Epsilon waves in arrhythmogenic right ventricular dysplasia were first defined and described in 1977 by Guy Fontaine (1936-2018). The waves may be seen more readily using Fontaine leads.
ECG Examples
Example 1

Baseline ECG of a patient with Arrhythmogenic Right Ventricular Dysplasia (ARVD), demonstrating:
- T-wave inversion in precordial and inferior leads, without RBBB pattern
- Epsilon wave in V1
- Localised widening of QRS in V1-2
Example 2
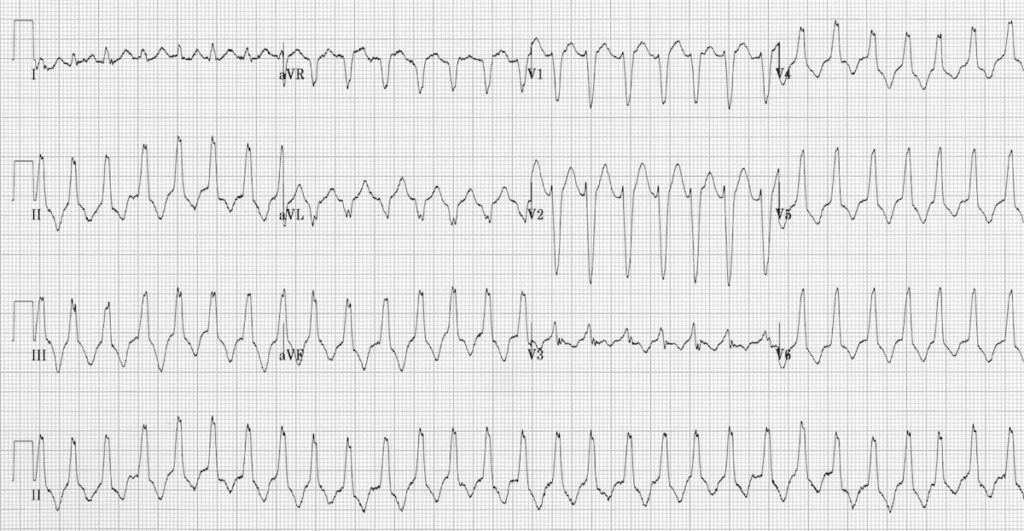
Right Ventricular Outflow Tract (RVOT) Tachycardia, demonstrated by:
- Regular broad complex tachycardia with LBBB morphology
- Inferior axis (+90 degrees)
- AV dissociation seen in V1
- Read more about RVOT tachycardia
Imaging
- Echocardiography is the first-line investigation, and may demonstrate a dilated, hypokinetic right ventricle with prominent apical trabeculae and dilatation of the RV outflow tract
- The imaging modality of choice in many centres is cardiovascular MRI, which can accurately demonstrate structural and functional features of ARVD such as fibrofatty infiltration and thinning of the RV myocardium, RV aneurysms, RV dilatation, regional wall motion abnormalities and global systolic dysfunction
- Histological diagnosis, either via endomyocardial biopsy or at autopsy, provides a definitive diagnosis but is impractical, and for those patients diagnosed at post-mortem… far too late!
Risk Assessment
Patients with ARVD are considered to be at high risk of sudden death if they have any of the following:
- A history of syncope due to cardiac arrest
- Recurrent arrhythmias not suppressed by anti-arrhythmic drug therapy
- A family history of cardiac arrest in first degree relatives
Treatment Options
Primary treatment involves arrhythmia suppression and prevention of thrombus formation:
- In patients with no high risk features, initial treatment is with anti-arrhythmic drugs such as beta-blockers or amiodarone to suppress cathecholamine-triggered ventricular arrhythmias. Currently, the most effective drug for this is sotalol. Warfarin is often recommended to prevent thrombus formation due to RV hypokinesis
- In patients with persistent symptomatic arrhythmias, radiofrequency ablation of conduction pathways may be attempted. However, progression of disease means over half of cases recur
- Patients with any high risk features require urgent insertion of an implantable cardioverter-defibrillator (ICD)
- Heart failure is treated in the usual way, with diuretics, ACE inhibitors and anticoagulants. In severe cases, cardiac transplantation may be required
Related Topics
- RVOT tachycardia
- The Epsilon Wave
- ECG Exigency 008 – Sudden Syncope on the Soccer Field
Learn From The Experts!
Professor Sanjay Sharma explains ARVD
References
- Protonotarios N, Tsatsopoulou A et al. Cardiac abnormalities in familial palmoplantar keratosis. Br Heart J. 1986 Oct;56(4):321-6.
- Fontaine G. Arrhythmogenic right ventricular dysplasia. Current Opinion in Cardiology, 1995; 10(1): 16-20
- Fontaine G, Fontaltaliran F. About the histology of arrhythmogenic right ventricular dysplasia. Circulation. 1997 Sep 16;96(6):2089-90
- Fontaine G, Chen HS. Arrhythmogenic Right Ventricular Dysplasia Back in Force. Am J Cardiol. 2014 May 15;113(10):1735-9
- Protonotarios N, Tsatsopoulou A. Naxos disease. Indian Pacing Electrophysiol J. 2005 Apr 1;5(2):76-80
- Anderson EL. Arrhythmogenic right ventricular dysplasia. Am Fam Physician. 2006 Apr 15;73(8):1391-8
- Perez Diez D, Brugada J. Diagnosis and Management of Arrhythmogenic Right Ventricular Dysplasia: An article from the E-Journal of the ESC Council for Cardiology Practice, European Society of Cardiology 2008
- Long B. Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy: EM Highlights. emDocs 2015
- Guy Hugues Fontaine (1936 – 2018)
- Dr Smith’s ECG Blog — ARVC
- ARVD.com. The website of the Johns Hopkins ARVD Patient Registry based in Baltimore, Maryland
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |


AMAZING WEBSITE FOR LEARNING ECG