ECG Case 131
An 88-year-old man is brought in by ambulance complaining of palpitations. BP 133/75, SpO2 100, GCS 15.
HR is fixed at 150 bpm. Is this atrial flutter?
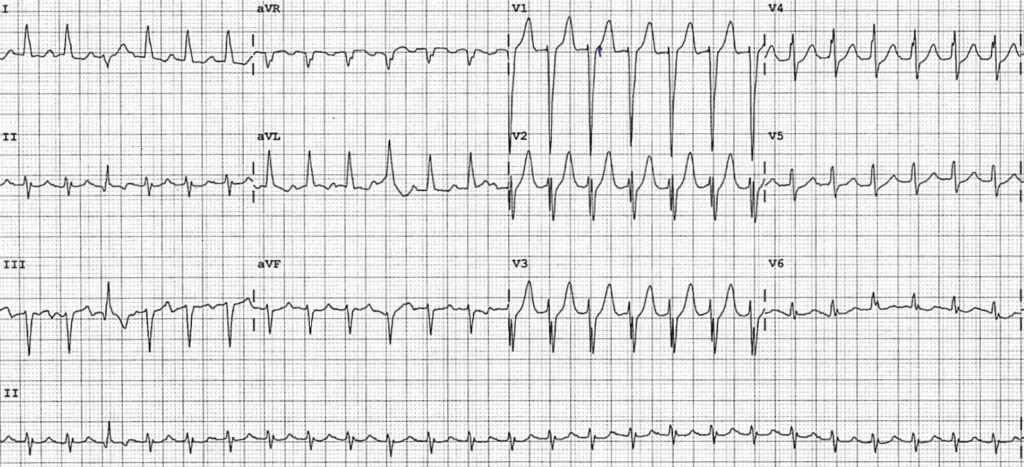
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
- Regular narrow complex tachycardia, rate 150 bpm
- Left anterior fascicular block
- ST depression in V2-5 is suggestive of rate-related ischaemia
- There is a long R-P interval, with P waves visible buried in the end of the T wave. These are seen as an additional positive deflection in lead II. Similarly upright P waves in aVL may be easily mistaken for T waves, which are actually inverted and visible just prior
- P wave axis is abnormal with a leftward deviation
- The third complex is a ventricular ectopic beat (VEB). Note that if this were a functional bundle block due to rate or aberrancy, we would expect the rate to change

In patients with a regular narrow complex tachycardia and a long R-P interval, our differentials include:
- Focal atrial tachycardia (FAT)
- Atypical AVNRT
- Permanent junctional reciprocating tachycardia (PJRT)
Atypical AVNRT and PJRT both produce retrograde P waves from a focus near the AV node – we would therefore expect a negative P wave axis in inferior leads, which is not the case here. An abnormal P wave axis here with an upright P wave in lead II suggests FAT as the most likely rhythm.
OUTCOME
Given doubt regarding the rhythm, and a fixed heart rate of 150 bpm that is often seen in atrial flutter, treating clinicians chose to administer adenosine to assist in differentiating the cause.
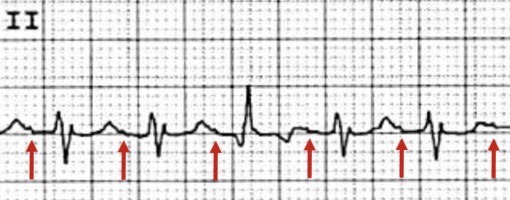
12mg of adenosine was administered and the patient reverted to sinus rhythm:

What is your interpretation?
- Sinus rhythm, rate ~100 bpm
- LAFB as seen earlier
- P wave axis has changed and is now within normal range, approximately +45 degrees
So this must have been AVNRT, right?
No.
Whilst less effective than in AVNRT, adenosine may cause reversion in some cases of FAT. Along with vagal manoeuvres it is reasonable to trial as a first line management option (see discussion).
Baseline bloods were unremarkable. The patient remained in sinus rhythm and was discharged without further intervention.
CLINICAL PEARLS
Last week we discussed differentiating regular narrow complex tachycardias, with the most common differentials being AV nodal re-entry tachycardia (AVNRT), atrial flutter, and focal atrial tachycardia (FAT). Other causes to be aware of include orthodromic atrioventricular re-entry tachycardias (AVRT). Understanding the mechanisms behind each of these tachycardias allows us to better identify them on the ECG.
Typical versus atypical AVNRT
The most common, typical form of AVNRT accounts for up to 90% of cases and is due to a slow-fast pathway. This produces “slow” anterograde conduction and rapid retrograde conduction, resulting in P waves buried in the QRS complex or visible shortly afterwards.
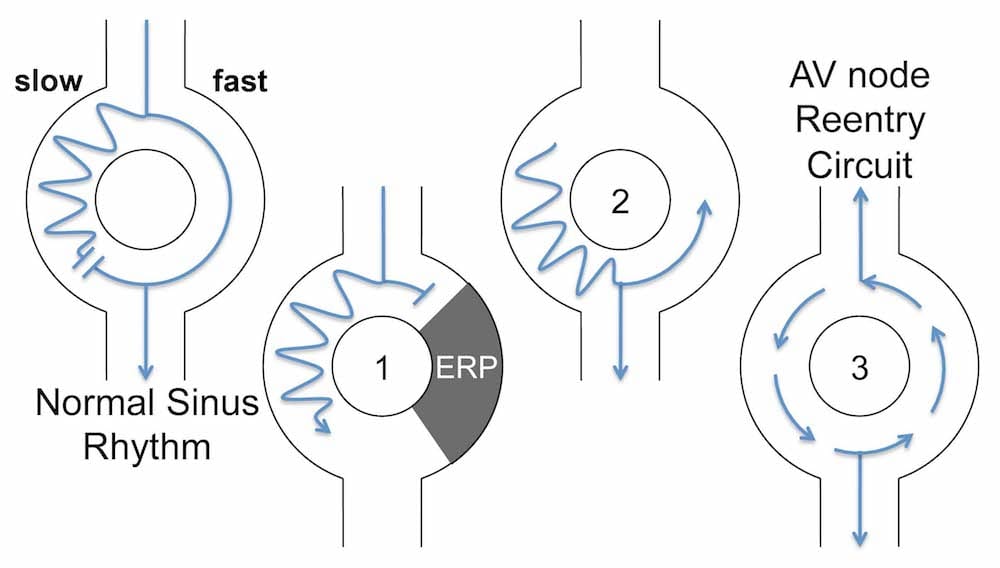
1) A premature atrial contraction (PAC) arrives while the fast pathway is still refractory, and is directed down the slow pathway
2) The ERP in the fast pathway ends, and the PAC impulse travels retrogradely up the fast pathway
3) The impulse continually cycles around the two pathways
Atypical AVNRT is characterised by slow retrograde conduction, due to either a fast-slow pathway or rarely a slow-slow pathway. P waves are usually seen after T waves or buried within them, with a long R-P interval.
In both forms of AVNRT, retrograde conduction of P waves produces a P wave axis directed away from inferior leads. P waves will be negative in lead II and positive in aVR and V1.
Permanent junctional reciprocating tachycardia (PJRT)
PJRT is a form of orthodromic AVRT in which retrograde conduction through the accessory pathway is slow. This creates a stable re-entry circuit, as there is already slow anterograde conduction through the AV node. The slow-slow nature of the re-entry circuit leads to a somewhat slower ventricular rate of around 120-160 BPM, with a long R-P interval. Retrograde P waves are most commonly inverted in inferior leads.
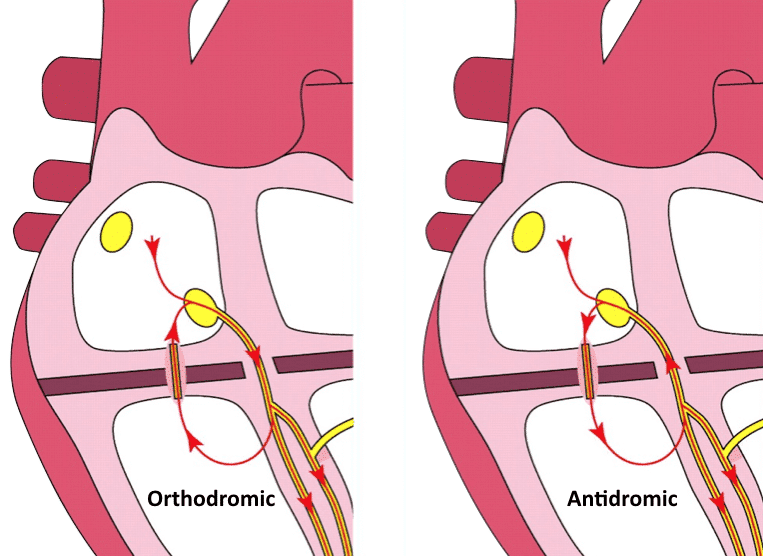
PJRT tends to be an incessant (or “permanent”) form of SVT that requires ablation to achieve arrhythmia control. The stable nature of the re-entry circuit means that chronic suppression is usually not possible with medications alone.
Note that our patient above had a ventricular ectopic beat (VEB) in the midst of his arrhythmia. This ECG feature alone excludes a permanent re-entry circuit such as PJRT as a differential here.
Subtle focal atrial tachycardia — is it not just sinus tachycardia?
P wave abnormalities in FAT are variable and depend on the location of the ectopic focus. They can be subtle, particularly in our patient above where there is a concurrent QRS axis deviation. Comparison of P wave axis in a sinus rhythm ECG allows us to determine if there was an initial ectopic focus. In the case of a near normal P wave axis, serial ECGs can assist in differentiating from sinus tachycardia. FAT will generally have a more fixed rate. If the rhythm is paroxysmal, FAT will have a more abrupt onset and/or termination, compared to sinus tachycardia which can take 30-60 seconds to “warm up” or slow down.
But this patient reverted with adenosine — does that not diagnose AVNRT?
Although generally less effective than in the case of AVNRT, adenosine may cause reversion of some automatic and triggered FATs to sinus rhythm. Even if unsuccessful, it is useful in diagnosing the underlying rhythm. Similar to unmasking flutter waves, adenosine will unmask rapid regular atrial activity in FAT. If reversion is successful, cessation of tachycardia without a blocked P wave favours FAT. A rhythm strip of reversion to sinus rhythm in our patient above would have been useful to confirm the diagnosis of FAT.
- In patients with a regular narrow complex tachycardia and long R-P interval, our main differentials include focal atrial tachycardia (FAT), atypical AVNRT and permanent junctional reciprocating tachycardia (PJRT)
- Examine the P wave axis to further differentiate between these rhythms
- Adenosine has a role in both diagnosing and treating FAT
Further reading
Related topics
References
- Iwai et al. Response to adenosine differentiates focal from macroreentrant atrial tachycardia: validation using three-dimensional electroanatomic mapping. Circulation. 2002 Nov 26;106(22):2793-9
Further reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Interventional cardiologist, ECG and hemodynamics fan. MD, Assoc. Prof. at Marmara University, Pendik T&R Hospital, Assoc. Editor at Archives of TSC, ESC National Prevention Coordinator



Can someone explain how there is a left deviation of the P axis, its positive in II and III?