Abdominal CT: diverticulitis
Detecting diverticulitis
As we age, it is common for the large intestine to form little round outpouchings in the wall called diverticula.
These diverticula usually do not cause much trouble, but sometimes they can become obstructed resulting in inflammation and infection (known as diverticulitis). These infected diverticula can even rupture if untreated.

Signs and symptoms
Patients with diverticulitis often present with left lower quadrant pain and an elevated white blood cell count. While diverticulitis is most common in the sigmoid colon, it can occur throughout the entire gastrointestinal (GI) tract. It can involve both the large and small bowel and thus can mimic other causes of abdominal pain.
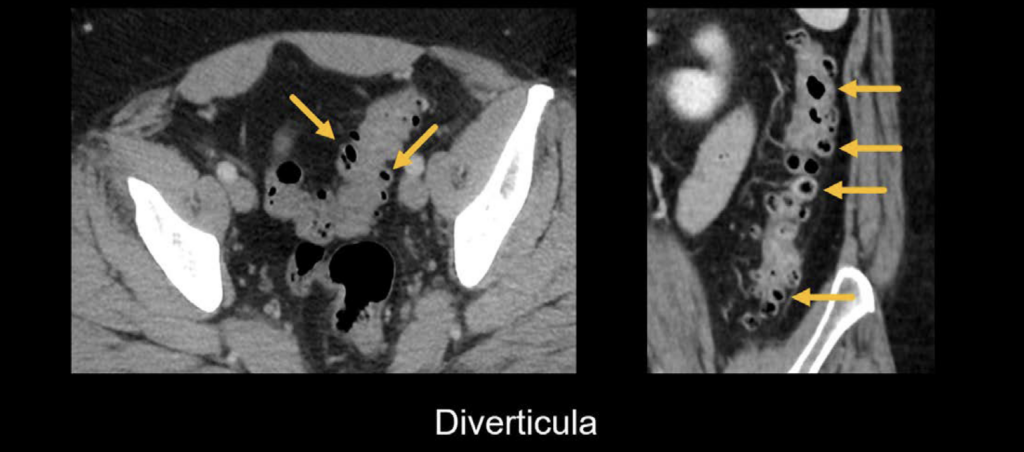
Diverticulosis
The CT images below show examples of diverticulosis, which is characterized by the presence of small, round, air-filled (i.e., dark) outpouchings (i.e., diverticula) projecting from the colon wall.
Uncomplicated diverticulitis
There are three key imaging findings that will help you diagnose diverticulitis:
- The diverticula will appear thickened and enlarged.
- The surrounding fat will appear hazy or stranded, indicating inflammation
- There will be inflammation of the nearby structures in reaction to the diverticulitis. In the example below, the bladder is compressed and mildly thickened as a result of the inflamed sigmoid colon. Notice the hazy fat stranding around the colon in this image as well, further supporting the presence of inflammation.

Clinical Case 1
Scroll through the PACS images for this case and look for the key findings that can indicate diverticulitis.
- Start by scrolling directly to the left lower quadrant, viewing both axial and coronal images side-by-side.
- Follow the descending colon down to the sigmoid colon. Notice there are numerous small outpouchings filled with air in both the sigmoid and descending colon. These are diverticula.
- In the proximal sigmoid colon, notice that there is a focal thickening of the colonic wall and a single, enlarged, and inflamed diverticulum.
- Also notice the haziness of the surrounding fat. These findings are diagnostic for uncomplicated sigmoid diverticulitis
Complicated diverticulitis
What about complicated forms of diverticulitis, as in the case of perforation? If a perforation has occurred, you will see three additional key findings:
- Extraluminal (i.e., free) air. This will look like black dots outside of the bowel and is usually easiest to see on bone or lung windows.
- Peritoneal inflammation This results from the spillage of stool from the perforation. In the example shown next, the small bowel loops are thickened and inflamed, indicating peritonitis
- Abscess formation This typically appears as an enhancing collection of fluid, air, and debris. In the example below, notice how the abscess sits on the bladder and causes the bladder wall to indent and become thickened due to reactive inflammation

Clinical Case 2
Let’s review a case of perforated sigmoid diverticulitis with abscess formation.
- Start in the upper abdomen and choose lung windows. You’ll notice several small locules of free intraperitoneal air, indicating perforation.
- Follow the descending colon down to the sigmoid. This gives you an anatomic anchor point to understand what is going on. On the way, you’ll notice several non-inflamed diverticula.
- Notice how the sigmoid colon is thickened and has surrounding stranding.
- Notice also how there is an enhancing collection outside of the colon wall, which contains dots of air and fluid within. There is also stranding and inflammation surrounding the collection, indicating that it is an abscess. This is caused by perforated sigmoid diverticulitis, which has walled off and formed an abscess.
Other sites of diverticula
Diverticula of the duodenum, jejunum, and caecum
It might be surprising to you to learn that diverticulitis can occur throughout the GI tract, even though the sigmoid colon is the most common location
Below are examples of diverticulitis involving the duodenum, jejunum, and caecum. Notice that the diverticula in the jejunum and duodenum are larger. Be aware that inflamed diverticula in the small bowel can be mistaken for perforation if you are unfamiliar with this diagnosis.

This is an edited excerpt from the Medmastery course Abdominal CT Pathologies by Michael P. Hartung, MD. Acknowledgement and attribution to Medmastery for providing course transcripts
- Hartung MP. Abdominal CT: Common Pathologies. Medmastery
- Hartung MP. Abdominal CT: Essentials. Medmastery
- Hartung MP. Abdomen CT: Trauma. Medmastery
References
- Lam L. CT Case 012. LITFL
- Rippey J. Ultrasound Case 037. LITFL
- Chandru P. General Surgery. Network Five
- Top 100 CT scan quiz. LITFL
Radiology Library: Abdominal CT: Imaging important abdominal structures
- Hartung MP. Abdominal CT: acute appendicitis
- Hartung MP. Abdominal CT: diverticulitis
- Hartung MP. Abdominal CT: small bowel obstruction
- Hartung MP. Abdominal CT: closed loop small bowel obstruction
- Hartung MP. Abdominal CT: enteritis and colitis
- Hartung MP. Abdominal CT: peptic ulcer disease
- Hartung MP. Abdominal CT: peptic ulcer perforation
- Hartung MP. Abdominal CT: bowel perforation
Abdominal CT interpretation
Assistant Professor of Abdominal Imaging and Intervention at the University of Wisconsin Madison School of Medicine and Public Health. Interests include resident and medical student education, incorporating the latest technology for teaching radiology. I am also active as a volunteer teleradiologist for hospitals in Peru and Kenya. | Medmastery | Radiopaedia | Website | Twitter | LinkedIn | Scopus
MBChB (hons), BMedSci - University of Edinburgh. Living the good life in emergency medicine down under. Interested in medical imaging and physiology. Love hiking, cycling and the great outdoors.


