Wolff–Parkinson–White syndrome
Wolff-Parkinson-White (WPW) Syndrome is a combination of the presence of a congenital accessory pathway and episodes of tachyarrhythmia.
WPW syndrome is characterized by a double stimulation of the ventricles. A premature conduction wave via accessory pathways (pre-excitation) stimulates the portions of the ventricles nearest the atrium; then the ventricles depolarize as a result of the conduction wave which proceeds normally through the atrioventricular (AV) node.
The clinical significance of this syndrome depends on the appearance of (supraventricular) reentry tachycardias.
History of Wolff–Parkinson–White syndrome
1909 – Retrospective review of published case reports looking for evidence of ventricular preexcitation shows the earliest example of WPW published is from August Hoffmann (1862-1929) published in MMW 1909; 56(2): 2259-2262
1913 – Albert Frank Stanley Kent (1863-1958) described, in the human heart, a communication between the right atrium and ventricle, in the lateral aspect.
The muscular connection between auricle and ventricle in the heart of man is not single and confined to the A.V. bundle, but it is multiple. One point at which a muscular connection between auricle and ventricle exists is situated at the right margin of the heart. The coordinated action of the chambers of the heart is to some extent dependent upon the integrity of muscular connections other than that which exists in the A.V. bundle. It is proposed, for purposes of identification, to refer to the connection described as the “right lateral auriculo-ventricular” connection.
Kent AFS 1913
The short PR interval and slurred initial portion of the QRS complex were first noted by:
1913 – Cohn and Fraser – Paroxysmal tachycardia and the effect of stimulation of the vagus nerve by pressure. Heart. 1913

1915 – Frank Norman Wilson (1890–1952) published a case in which ‘the vagus influenced the form of the ventricular complex of the electrocardiogram‘
1921 – Alfred M. Wedd (1887–1967) described 6 cases of Paroxysmal tachycardia with reference to nomotopic tachycardia and role of extrinsic cardiac nerves. Two of the cases displayed short PR, slurred upstroke of the QRS, later to be identified as the delta wave.

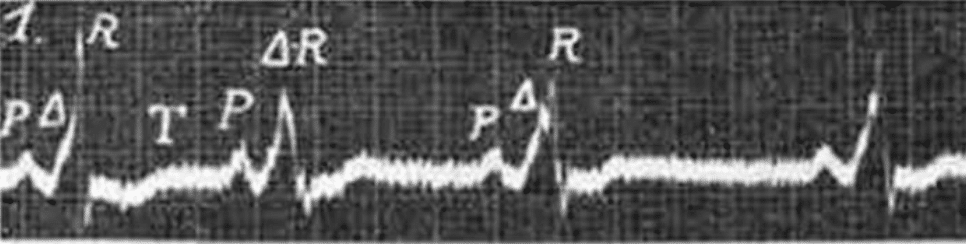
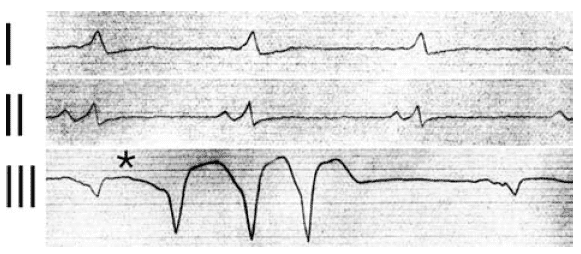
1929 – Francis Bach (1900-1975) published the case of paroxysmal tachycardia of forty-eight years’ duration and right branch bundle block. The patient had been reviewed by Bach in 1928, but was initially reviewed by Sir James Mackenzie and Dr. Parkinson at the London Hospital in 1914. The initial ECG post tachycardia resolution from 1914 in which ‘wave in Lead II is quite atypical‘ is shown:

- Walter Wile Hamburger [Med Clin North Am, 1929]
1928 – On April 2 a young man was referred to Paul Dudley White because his physician was perplexed by the occurrence of paroxysmal atrial fibrillation in a healthy individual. White was preparing for visits to overseas medical centers and took the ECGs with him.
- Vienna: the tracing was deemed to represent nothing more unusual than bundle-branch block and atrioventricular (AV) nodal rhythm
- London: Parkinson was interested and found a further seven cases to add to the four from Boston.
1930 – Wolff L, Parkinson J, and White PD publish the eleven cases as definitive description of the syndrome – ‘Bundle Branch Block with Short P-R Interval in Healthy Young People Prone to Paroxysmal Tachycardia.’ A review of the literature confirmed and acknowledged the previously described cases as above. Wolff, Parkinson, and White erroneously thought that the wide QRS complex was caused by a type of bundle-branch block.
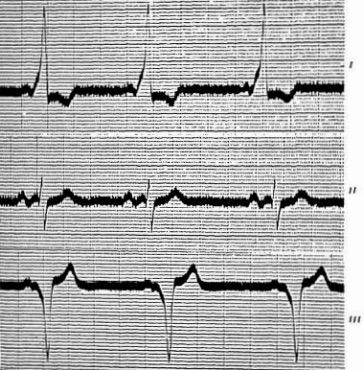
1933 – Charles C. Wolferth (1887-1965) and Francis Clark Wood (1901-1990) suggested that the abnormal slurring of the initial part of the QRS complex, and prolongation of the QRS complex were not due to bundle-branch block but to:
…an actual acceleration of the passage of the impulse from the auricle to a section of the ventricle…in keeping with the possibility that an accessory pathway of AV conduction such as described by Kent (1913) between the right auricle and right ventricle could be responsible for the phenomenon manifested by these cases
Wolferth CC, Wood FC. 1933
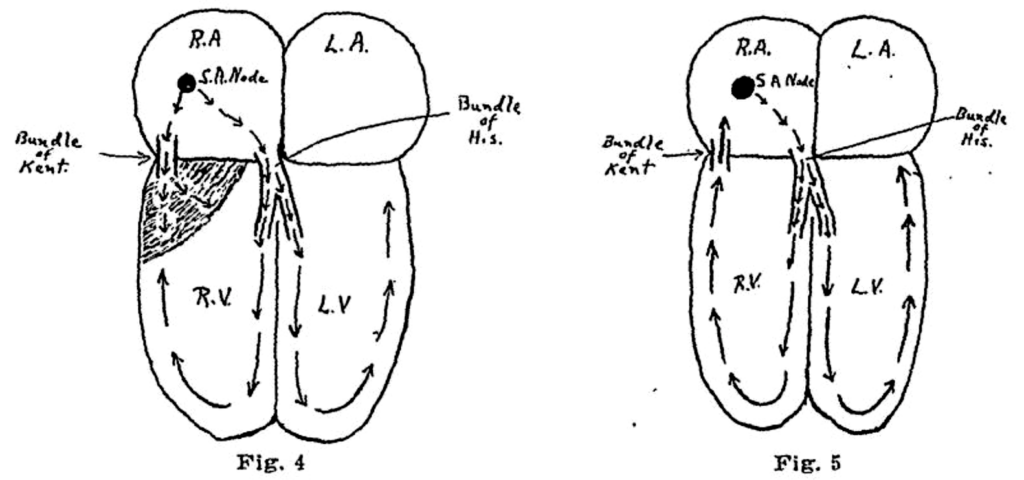
Fig 4. Schematic representation to illustrate the hypothesis of premature transmission of the impulse through the bundle of Kent to the right ventricle. The shaded area represents the section which is activated before the impulse reaches the ventricles through the bundle of His. This mechanism would account for the short PR interval, the widening of the QRS complex and the slurring of the initial deflection.
Fig 5. Schematic representation showing the path of an impulse which might be responsible for exciting a paroxysm of supraventricular tachycardia or auricular fibrillation. Wolferth CC, Wood FC. 1933
1944 – Marcel Segers with colleagues J. Lequime and H. Denolin are credited with proposing the Δ to represent the triangle shape at the base of the upsloping QRS complex. They described the ‘… deformation of the PQ segment is the result of a supplementary electrical deflection that we propose to call Δ‘ . This became more commonly described as the ‘delta wave‘
However, Segers et al actually proposed that the Δ wave was a discrete a discrete and autonomous wave between P and Q. They did state that the wave could fuse with the base of QRS complex (figure C) to form a slurred upstroke, and attributed the Δ wave fusion with the bundle branch phenomenon of WPW (Figure D)

Schéma a: Onde Δ représentée par une simple inclinaison du segment PQ.
Schéma b ; Tracé avec onde Δ complètement autonome : le point Q se marque nettement après Δ , et dans ces conditions les intervalles PQ et QRS gardent en réalité une valeur normale.
Schéma c : Tracé avec onde Δ formant un « pied » accolé à QRS : l’onde Q correspond au point d’inflexion séparant Δ et R. Le pointillé montre l’évolution de l’onde Δ se poursuivant pendant toute la durée du complexe ventriculaire, selon l’hypothese de Eckey et Schäfer; cette onde diphasique viendrait se superposer au complexe ventriculaire normal et déterminerait ainsi le décalage de ST et la déformation de T.
Schéma d: Les ondes Δ et QRS sont complètement fusionnées en un complexe unique et élargi du type bloc de branche (syndrome de Wolff, Parkinson et White); le point Q et le sommet R ne sont plus visibles et l’onde T se présente en « forme d’escalier »
Diagram a: Δ wave represented by a simple tilt of the PQ segment.
Diagram b; Plot with completely autonomous Δ wave: the Q point is clearly marked after Δ , and under these conditions the PQ and QRS intervals actually keep a normal value.
Diagram c: Plot with Δ wave forming a “foot” attached to QRS: the Q wave corresponds to the point of inflection separating Δ and R. The dotted line shows the evolution of the Δ wave continuing throughout the duration of the complex ventricular, according to the hypothesis of Eckey and Schäfer; this diphasic wave would come to be superimposed on the normal ventricular complex and would thus determine the shift of ST and the deformation of T.
Diagram d: Δ and QRS waves are completely fused into a single, enlarged bundle-branch block-like complex (Wolff-Parkinson-White syndrome); the Q point and the R vertex are no longer visible and the T wave appears in a “staircase shape”
1951 – White appreciated that the conduction disturbance was not due to bundle branch block, but rather to rapid conduction of the depolarizing impulse from the atrium to one or the other ventricles as proposed by Wolferth and Wood in 1933. He recorded a case and his thoughts in the fourth edition of his single-authored book, Heart Disease in which he refers to the conduction disorder as “An odd electrocardiograhic anomaly, probably congenital in origin…”
The functional aspects of this reentrant pathway were confirmed by electrophysiological studies in the 1960s with subsequent correction of this disorder by surgical interruption of the pathway, or, as is now done, by catheter directed radiofrequency ablation.
Associated Persons
- August Hoffmann (1862-1929)
- Wilhelm His Jr. (1863–1934)
- Albert Frank Stanley Kent (1863-1958)
- Louis Wolff (1898-1972)
- Sir John Parkinson (1885-1976)
- Paul Dudley White (1886-1973)
- Charles Christian Wolferth (1887-1965)
- Francis Clark Wood (1901-1990)
References
Historical references
- Gaskell WH. On the Innervation of the Heart, with especial reference to the Heart of the Tortoise. J Physiol. 1883 Aug; 4(2-3): [43]-127, 230-1-230-14
- His Jr W. Die Thätigkeit des embryonalen Herzens und deren Bedeutung für die Lehre von der Herzbewegung beim Erwachsenen. Arbeiten aus der medicinischen Klinik zu Leipzig. Herausgegeben von H. Curschmann. 1893; 14 – 49. [The activity of the embryonic human heart and its significance for understanding of the heart movement in the adult Translated Bast TH, Gardner WD Journal of the History of Medicine and Allied Sciences, 1949; 4(3): 289–318.] [Bundle of His]
- Hoffmann A. Die Arythmie des Herzens im Elektrokardiogramm. Münchener medizinische Wochenschrift. 1909; 56: 2259-2262
- Cohn AE, Fraser FR. Paroxysmal tachycardia and the effect of stimulation of the vagus nerve by pressure. Heart. 1913; 14(5): 93-105.
- Hoffmann A. Die Elektrographie als Untersuchungsmethode des Herzens und ihre Ergebnisse: insbesondere für die Lehre. 1914
- Kent AFS. The right lateral auriculo-ventricular junction of the heart. Journal of Physiology 1914; 48(supp): 22-24 [Bundle of Kent]
- Kent AFS. A lecture on some problems in cardiac physiology: Delivered before the University of London, June 18th, 1914. Br Med J. 1914 Jul 18;2(2794):105-106 [Bundle of Kent]
- Wilson FN. A case in which the vagus influenced the form of the ventricular complex of the electrocardiogram. 1915. [Reprint: Ann Noninvasive Electrocardiol. 2002 Apr;7(2):153-73]
- Wedd, A.M. Paroxysmal tachycardia with reference to nomotopic tachycardia and role of extrinsic cardiac nerves. Arch Intern Med. 1921;27:571–590
- Bach F. Paroxysmal Tachycardia of Forty-eight years’ Duration and right Branch Bundle Block. Proc R Soc Med. 1929 Feb;22(4):412-4
- Hamburger WW. Bundle branch block. Four cases of intraventricular block showing some interesting and unusual clinical features. Med Clin North Am 1929; 13: 343-362
- Wolff L, Parkinson J, White PD. Bundle-branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia. American Heart Journal. 1930; 5: 685-704 [Reprint: Ann Noninvasive Electrocardiol. 2006 Oct;11(4):340-53. PMID 17040283]
- Wolferth CC, Wood FC. The mechanism of production of short P-R intervals and prolonged QRS complexes in patients with presumably undamaged hearts: hypothesis of an accessory pathway of auriculoventricular conduction (bundle of Kent). American Heart Journal. 1933; 8: 297-311.
- Segers PM, Lequime J, Denolin H. L’activation ventriculaire précoce de certains cœurs hyperexeitables. Étude de I’onde Δ de I’électrocardiogramme. Cardiologia. 1944; 8(3-4):113-167. [Delta wave]
Eponymous term review review
- Wellens HJ, Schuilenberg RM, Durrer D. Electrical stimulation of the heart in patients with Wolff-Parkinson-White syndrome, type A. Circulation. 1971 Jan;43(1):99-114
- Hurst JW. Naming of the waves in the ECG, with a brief account of their genesis. Circulation. 1998 Nov 3;98(18):1937-42
- Von Knorre GH. The earliest published electrocardiogram showing ventricular preexcitation. Pacing Clin Electrophysiol. 2005 Mar;28(3):22830
- Moss, AJ. History of Wolff-Parkinson-White Syndrome: Introductory Note to a Classic Article by Louis Wolff, M.D., John Parkinson, M.D., and Paul D. White, M.D. Ann Noninvasive Electrocardiol. 2006 Oct;11(4):338-9
- Scheinman MM. The History of the Wolff–Parkinson–White Syndrome. Rambam Maimonides Med J. 2012 Jul; 3(3): e0019
- ECG Library – Pre-excitation Syndromes. LITFL
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
[cite]
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner