Idiopathic Fascicular Left Ventricular Tachycardia
ECG Features of Idiopathic Fascicular Left Ventricular Tachycardia
- Monomorphic ventricular tachycardia eg. fusion complexes, AV dissociation, capture beats
- QRS duration 100 – 140 ms — this is narrower than other forms of VT
- Short RS interval (onset of R to nadir of S wave) of 60-80 ms — the RS interval is usually > 100 ms in other types of VT
- RBBB Pattern
- Axis deviation depending on anatomical site of re-entry circuit (see classification)
Overview
- Fascicular tachycardia is the most common idiopathic VT of the left ventricle
- It is a re-entrant tachycardia, typically seen in young healthy adults without structural heart disease Attacks can be precipitated by exercise, excitement, and infection
- Characterized by a right bundle branch block pattern and left axis deviation
- Verapamil is the first line treatment
AKA: Fascicular tachycardia, Belhassen-type VT, verapamil-sensitive VT or infrafascicular tachycardia.
Idiopathic VT
- 90% of patients presenting with monomorphic VT are secondary to structural heart disease, including ischaemic heart disease, congenital heart disease, valvular dysfunction and myocardial dysfunction
- 10% of cases of monomorphic VT occur in the absence of structural heart disease and are termed idiopathic VT
- 75-90% of idiopathic VT arise from the right ventricle — e.g right ventricular outflow tract tachycardia
- 10-25% of idiopathic VT arise from an ectopic focus within the left ventricle, especially the left posterior fascicle (Fascicular VT). First described as a unique electrophysiologic entity in 1981 by Belhassen et al [Belhassen VT; fascicular or intrafascicular tachycardia; or verapamil sensitive VT; narrow complex VT]
Causes
Usually occurs in young healthy patients (15-40 years of age; 60-80% male). Most episodes occur at rest but may be triggered by exercise, stress and beta agonists. The mechanism is re-entrant tachycardia due to an ectopic focus within the left ventricle.
NB. A similar ECG pattern of fascicular VT may occur with digoxin toxicity, but here the mechanism is enhanced automaticity in the region of the fascicles.
Classification
Fascicular tachycardia can be classified based on ECG morphology corresponding to the anatomical location of the re-entry circuit:
- Posterior fascicular VT (90-95% of cases): RBBB morphology + left axis deviation; arises close to the left posterior fascicle
- Anterior fascicular VT (5-10% of cases): RBBB morphology + right axis deviation; arises close to the left anterior fascicle
- Upper septal fascicular VT (rare): atypical morphology – usually RBBB but may resemble LBBB instead; cases with narrow QRS and normal axis have also been reported. Arises from the region of the upper septum
Diagnosis and Management
- Diagnosis can be difficult and this rhythm is often misdiagnosed as SVT with RBBB; the diagnosis is made by observing specific features of VT, e.g. fusion/capture beats, AV dissociation.
- Idiopathic fascicular tachycardia may prove difficult to treat as it is often unresponsive to adensoine, vagal maneouvers, and lignocaine. However, it characteristically responds to verapamil
- Digoxin-induced fascicular VT is responsive to Digoxin Immune Fab
ECG Examples
Example 1
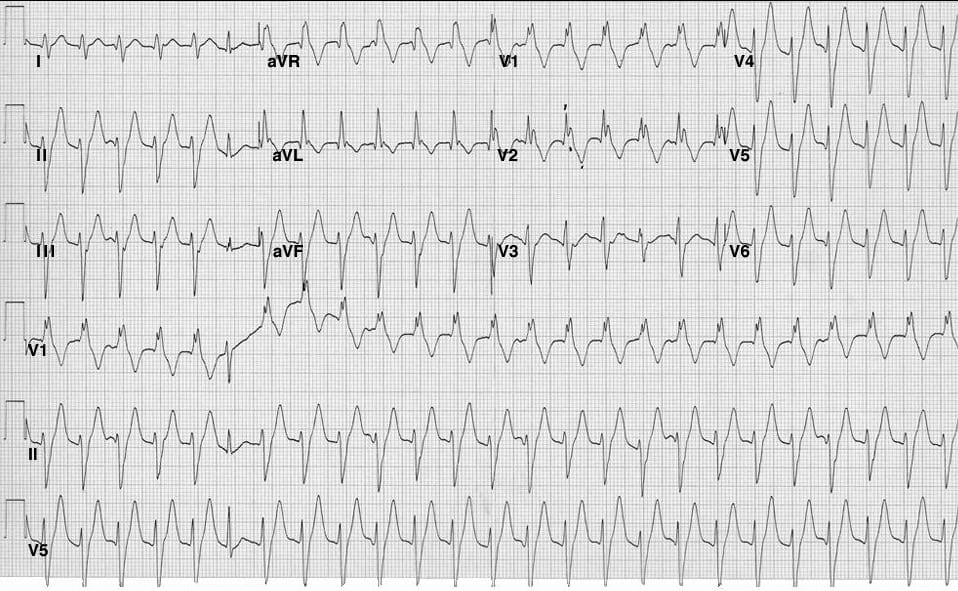
Idiopathic Fascicular VT:
- Broad-complex complex tachycardia with modest increase in QRS width (~120 ms)
- RBBB morphology (RSR’ in V1)
- Left axis deviation (-90 degrees)
- Narrow-complex capture beat (complex #6)
- Several dissociated P waves are seen in the lead II rhythm strip (associated with the 3rd, 10th, 14th, 18th and 22nd QRS complexes)
This rhythm could easily be mistaken for SVT with bifascicular block (RBBB + LAFB) — however, the presence of dissociated P waves and a narrow-complex capture beat indicates that this is fascicular VT arising from the left posterior fascicle.
This ECG is reproduced from Heart Pearls.com
Example 2


Example 3


Related Topics
- Overview of VT
- Right Ventricular Outflow Tract Tachycardia
- Polymorphic VT / Torsades De Pointes
- Bidirectional VT
- Ventricular Flutter
- VT versus SVT with aberrancy
References
- Edhouse J, Morris F. ABC of clinical electrocardiography: Broad complex tachycardia-Part II. BMJ. 2002 Mar 30;324(7340):776-9
- Eynon CA, Howe L, Firoozan S. Fascicular tachycardia: uncommon or just unrecognised? Emerg Med J 2002;19:477–478
- Chiu C, Sequeira IB. Diagnosis and treatment of idiopathic ventricular tachycardia. AACN Clin Issues. 2004 Jul-Sep;15(3):449-61
- Francis J, Venugopal K, Khadar SA, Sudhayakumar N, Gupta AK. Idiopathic Fascicular Ventricular Tachycardia. Indian Pacing Electrophysiol J. 2004 Jul-Sep; 4(3): 98–103
- Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. 1981 Dec;46(6):679-82
- Quimby TW, Clark AA, Fix ML. Idiopathic ventricular tachycardia: Belhassen type. West J Emerg Med. 2010 Sep;11(4):389-90.
- Moreno Reviriego S. Idiopathic fascicular left ventricular tachycardia. An article from the E-Journal of the ESC Council for Cardiology Practice, Dec 2010
- Wieland JM, Marchlinski FE. Electrocardiographic response of digoxin-toxic fascicular tachycardia to Fab fragments: implications for tachycardia mechanism. Pacing Clin Electrophysiol. 1986 Sep;9(5):727-38
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Should example 3 be SVT with bifacicular block (RBBB+Left posterior fascicular block)? Because there is only wide complex QRS in all leads, no narrow complex, also no fusion beats, capture beat are found in all leads. Thank you for your concern