Sinus Node Dysfunction (Sick Sinus Syndrome)
Sinus Node Dysfunction Overview
A disease characterized by abnormal sinus node functioning with resultant bradycardia and cardiac insufficiency. May be multi-factorial in origin. Causes can be considered either intrinsic or extrinsic.
Intrinsic Causes
- Idiopathic Degenerative Fibrosis (commonest).
- Ischaemia.
- Cardiomyopathies.
- Infiltrative Diseases e.g. sarcoidosis, haemochromatosis.
- Congenital abnormalities.
Extrinsic Causes
- Drugs e.g. digoxin, beta-blockers, calcium channel blockers.
- Autonomic dysfunction.
- Hypothyroidism.
- Electrolyte abnormalitites — e.g. hyperkalaemia.
ECG in Sinus Node Dysfunction
ECG abnormalities can be variable and intermittent. Multiple ECG abnormalities can be seen in sinus node dysfunction including:
- Sinus Bradycardia.
- Sinus Arrhythmia — associated with sinus node dysfunction in the elderly in the absence of respiratory pattern association.
- Sinoatrial Exit Block.
- Sinus Arrest — pause > 3 seconds.
- Atrial fibrillation with slow ventricular response.
- Bradycardia – tachycardia syndrome.
Bradycardia – tachycardia syndrome
- Alternating bradycardia with paroxysmal tachycardia, often supraventricular in origin.
- On cessation of tachyarrhythmia may be a period of delayed sinus recovery e.g. sinus pause or exit block.
- If significant this period of delayed recovery may result in syncope.
Clinical Manifestations
- Commonly seen in the elderly but sinus node dysfunction can affect all age groups.
- Symptoms are due to decreased cardiac output and end-organ hypoperfusion associated with cardiac rhythm abnormality.
- Wide range of clinical symptoms including syncope, near-syncope, dizziness, fatigue and palpitations.
Treatment
- Correction / removal of extrinsic causes e.g. non-essential drugs.
- Pacemaker insertion – requires correlation of both ECG abnormalities and clinical symptoms.
Recommendation for Pacing in Sinus Node Dysfunction
Class I – Evidence and/or agreement that permanent pacing is useful and effective.
- Sinus node dysfunction with documented symptomatic bradycardia, including frequent sinus pauses that produce symptoms. In some patients, bradycardia is iatrogenic and will occur as a consequence of essential long-term drug therapy of a type and dose for which there are no acceptable alternatives.
- Symptomatic chronotropic incompetence.
Class IIa – Conflicting evidence/ divergence of opinion but weight of evidence / opinion in favour
- Sinus node dysfunction occurring spontaneously or as a result of necessary drug therapy, with heart rate less than 40 bpm when a clear association between significant symptoms consistent with bradycardia and the actual presence of bradycardia has not been documented.
- Syncope of unexplained origin when major abnormalities of sinus node function are discovered or provoked in electrophysiological studies.
Class IIb – Conflicting evidence/divergence of opinion where usefulness / efficacy is less well established
- In minimally symptomatic patients, chronic heart rate less than 40 bpm while awake.
Class III – Permanent pacing is not useful/effective and in some cases may be harmful.
- Sinus node dysfunction in asymptomatic patients, including those in whom substantial sinus bradycardia (heart rate less than 40 bpm) is a consequence of long-term drug treatment.
- Sinus node dysfunction in patients with symptoms suggestive of bradycardia that are clearly documented as not associated with a slow heart rate.
- Sinus node dysfunction with symptomatic bradycardia due to nonessential drug therapy.
ECG Examples
Example 1
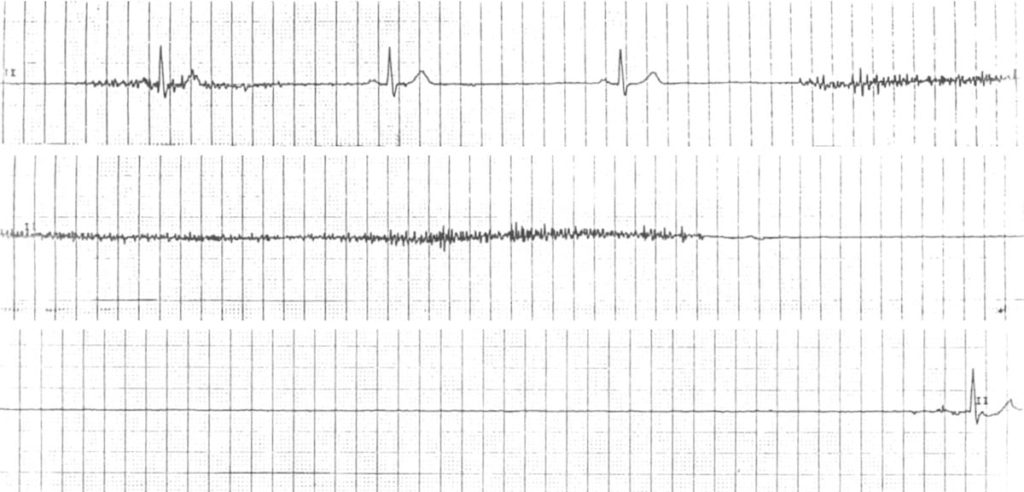
Sinus arrest:
- Prolonged absence of sinus node activity (absent P waves) > 3 seconds.
Example 2
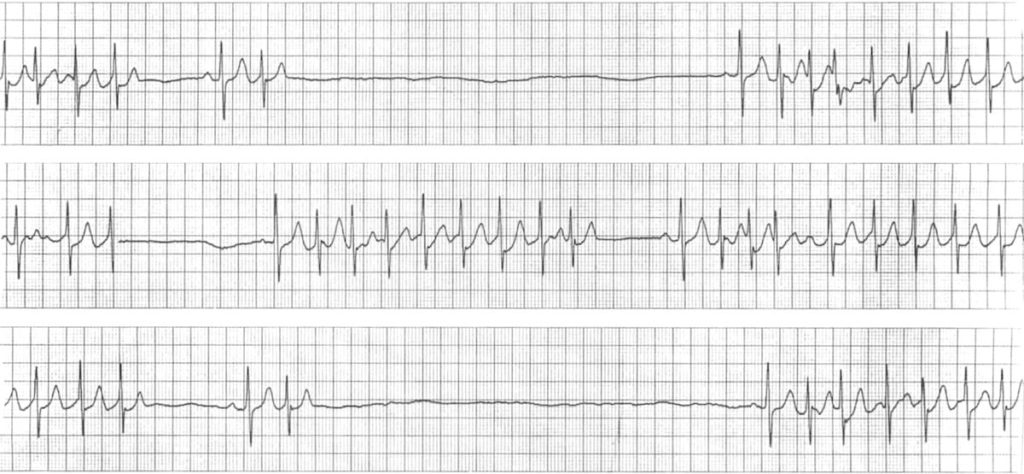
Bradycardia-tachycardia syndrome:
- Runs of tachycardia interspersed with long sinus pauses (up to 6 seconds).
- The sinus rate is extremely slow, varying from 40 bpm down to around 10 bpm in places.
- Sinus beats are followed by paroxysms of junctional tachycardia at around 140 bpm.
Related Topics
References
- Da Costa D, Brady WJ, Edhouse J. Bradycardias and atrioventricular conduction block. BMJ. 2002 Mar 2;324(7336):535-8
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner

