Accelerated Idioventricular Rhythm (AIVR)
Accelerated Idioventricular Rhythm (AIVR) Overview
AIVR, also known as Accelerated Ventricular Rhythm, results when the rate of an ectopic ventricular pacemaker exceeds that of the sinus node. Often associated with increased vagal tone and decreased sympathetic tone.
ECG Features of AIVR
- Regular rhythm
- Rate typically 50-120 bpm
- Three or more ventricular complexes; QRS duration > 120ms
- Fusion and capture beats
Pathophysiology
- Proposed mechanism is enhanced automaticity of ventricular pacemaker, although triggered activity may play a role, particularly in ischaemia and digoxin toxicity
- AIVR is classically seen in the reperfusion phase of an acute STEMI, e.g. post thrombolysis
- Usually a well-tolerated, benign, self-limiting arrhythmia
Ventricular Rate
Note that the rate of AIVR distinguishes it from others rhythms of similar morphology:
- Rates < 50 bpm are consistent with a Ventricular Escape Rhythm
- Rates > 110 bpm are consistent with Ventricular Tachycardia
Causes of Accelerated Idioventricular Rhythm (AIVR)
There are multiple causes of AIVR including:
- Reperfusion phase of acute myocardial infarction (MI) — most common cause
- Beta-sympathomimetics such as isoprenaline or adrenaline
- Drug toxicity, especially digoxin, cocaine and volatile anaesthetics such as desflurane
- Electrolyte abnormalities
- Cardiomyopathy, congenital heart disease, myocarditis
- Return of spontaneous circulation (ROSC) following cardiac arrest — this probably relates to reperfusion of acute MI as underlying cause of arrest
- Athletic heart
Management
- AIVR is a benign rhythm in most settings and does not usually require treatment
- Usually self limiting and resolves when sinus rate exceeds that of the ventricular foci
- Administration of anti-arrhythmics may cause precipitous haemodynamic deterioration and should be avoided
- Treat the underlying cause: e.g. correct electrolytes, restore myocardial perfusion
- Patients with low cardiac output states (e.g. severe biventricular failure) may benefit from restoration of AV synchrony to restore atrial kick – in this case atropine may be trialed in an attempt to increase sinus rate and AV conduction
Isorhythmic AV dissociation
This refers to AV dissociation with sinus and ventricular complexes occurring at identical rates. This is in contrast to complete heart block, where the atrial rate is usually faster than the ventricular rate.
Isorhythmic AV dissociation is usually due to functional block at the AV node due to retrograde ventricular impulses. These ventricular impulses depolarise the AV node, leaving it refractory to incoming sinus impulses (= “interference-dissociation”). Identical rates in isorhythmic AV dissociation can create the illusional of an association between the two chambers.
ECG Examples
Example 1a
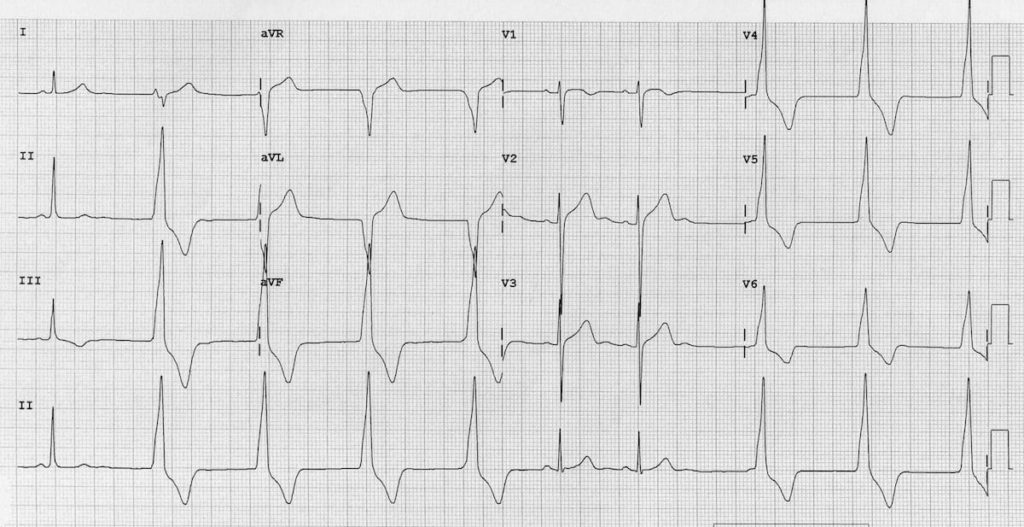
- Ventricular rhythm at 60 bpm
- Multiple sinus capture beats
Competing sinus and idioventricular pacemakers are present. There is an underlying sinus arrhythmia, with sinus capture occurring when the sinus rate exceeds the idioventricular rate.
This patient was a healthy 36-year old marathon runner with presumably very high resting vagal tone causing sinus bradycardia and sinus arrhythmia.
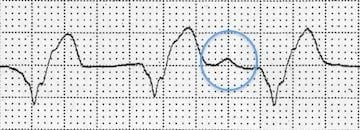
Example 1b
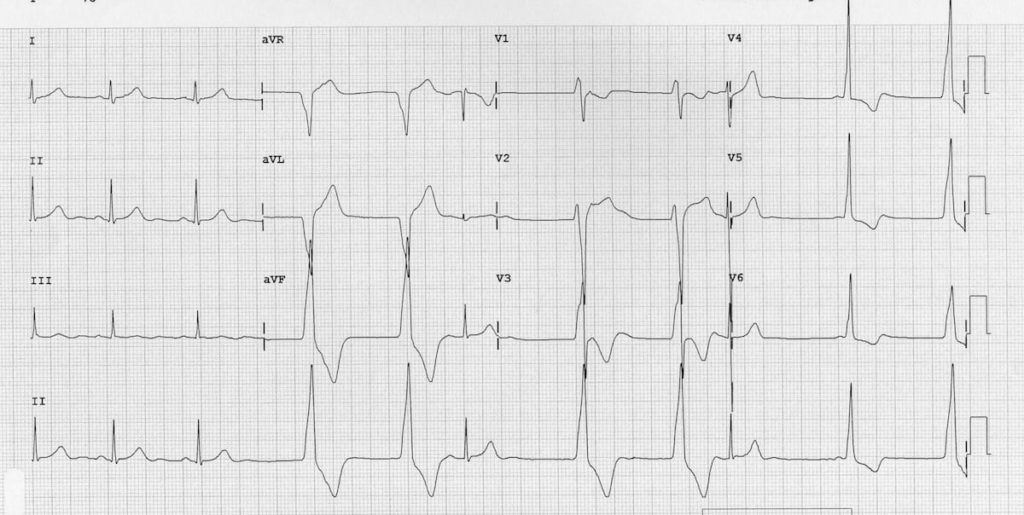
Another ECG from the same patient showing:
- AIVR at 60 bpm
- Isorhythmic AV dissociation with frequent sinus capture beats
- A fusion beat
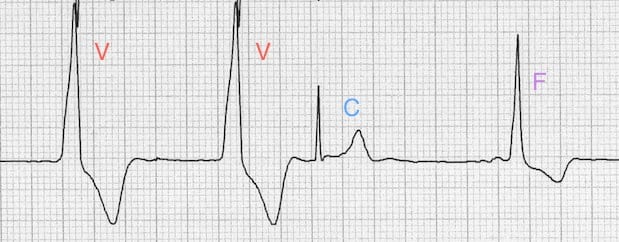
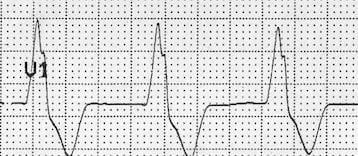
Example 2
- Ventricular rhythm at 75 bpm
- AV dissociation — a dissociated P wave is seen in the rhythm strip (after 9th complex), another in lead aVL. Elsewhere, dissociated P waves cause intermittent deformation of the QRS complexes
- The taller left rabbit ear sign is present — there is a notched R wave in V1 with a taller initial R wave; this is highly specific for a ventricular origin of the QRS complexes
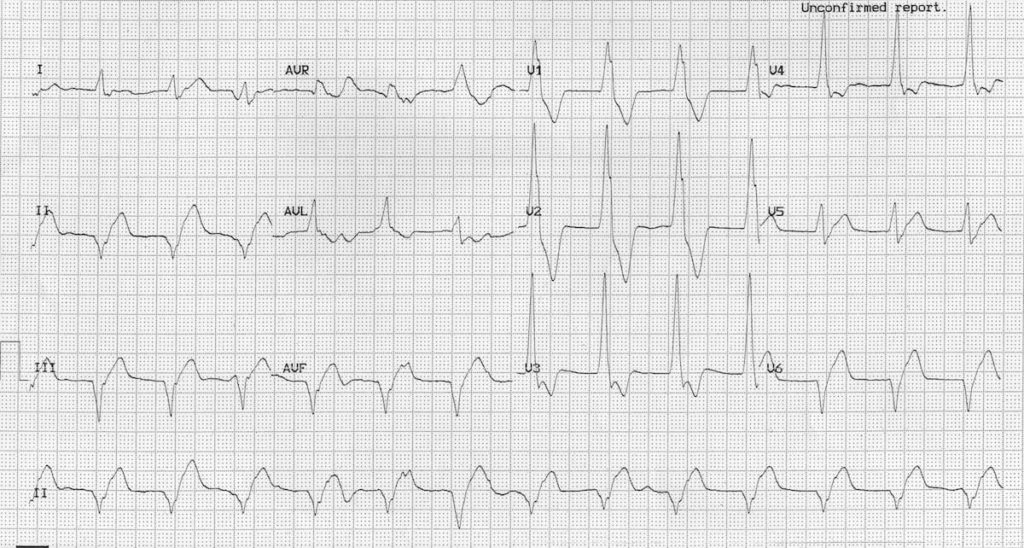
Example 3
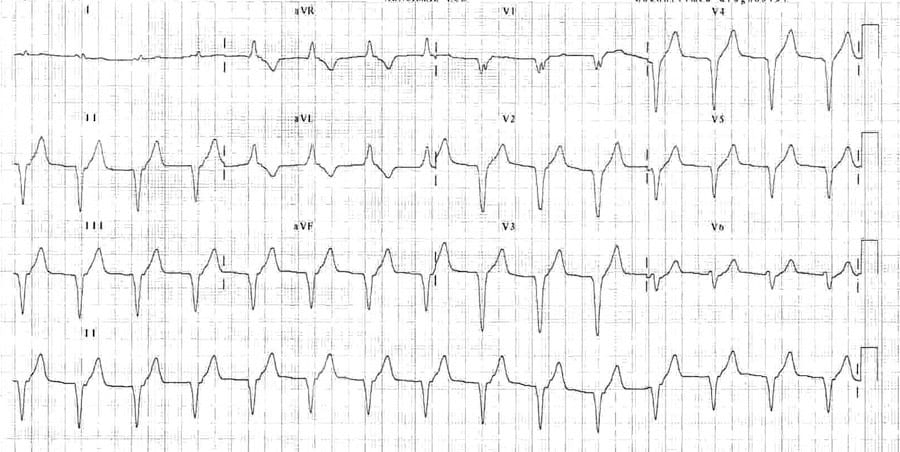
- Broad complex at 90 bpm
- No visible P waves
This dysrhythmia occurred following reperfusion from an anterior STEMI.
Related Topics
References
- Dr Smith’s ECG Blog – AIVR cases
- Riera AR, Barros RB, de Sousa FD, Baranchuk A. Accelerated idioventricular rhythm: history and chronology of the main discoveries. Indian Pacing Electrophysiol J. 2010;10(1):40-48.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Hi guys
Recently came across this to add to your list of causes for AIVR
Freire, G., Dubrow, I. Accelerated Idioventricular Rhythm in Newborns: A Worrisome But Benign Entity with or without Congenital Heart Disease. Pediatr Cardiol 29, 457–462 (2008). https://doi.org/10.1007/s00246-007-9024-z
Cheers
J
[…] https://litfl.com/accelerated-idioventricular-rhythm-aivr/ […]