Atrial fibrillation/flutter in pre-excitation
Overview
- Atrial fibrillation (AF) occurs in 20% of patients with Wolff-Parkinson-White (WPW) pattern, and atrial flutter in 7%
- The presence of an accessory pathway (AP) allows for rapid conduction directly to the ventricles, bypassing the AV node
- Ensuing rapid ventricular rates may result in degeneration to ventricular tachycardia (VT) or ventricular fibrillation (VF)
- The administration of AV nodal blocking drugs preferences conduction via the AP, and may precipitate ventricular arrhythmias and cardiac arrest
ECG features of atrial fibrillation in WPW:
- Rate > 200 bpm
- Irregular rhythm, with extremely high rates in some places — up to 300 bpm (this is too rapid to be conducted via the AV node)
- Wide QRS complexes due to abnormal ventricular depolarisation via AP
- Subtle beat-to-beat variation in QRS morphology
- Axis remains stable, unlike Polymorphic VT
Atrial Flutter results in the same features as AF in WPW except the rhythm is regular and may be mistaken for VT.
Management of AF with WPW
In patients that are unstable due to AF, urgent synchronised DC cardioversion is required.
However, it is in the more stable patient that we must be cautioned with the presence of an AP. Treatment with AV nodal blocking drugs (e.g. adenosine, calcium channel blockers, beta blockers) should be avoided for two reasons:
- Most APs have a shorter refractory period than the AV node, hence the ventricular rate can be more rapid if AV conduction occurs preferentially via the AP
- Normally, anterograde conduction occurs via both the AP and AV node, and these wavefronts fuse in the ventricles. Conduction through the AV node is actually a brake on AP conduction, ceasing its propagation path in the ventricle
AV nodal blockade can thus be catastrophic, preferencing conduction via the AP and leading to uninhibited propagation through the ventricles. The result is an increase in ventricular rate and possible degeneration into VT or VF.
The most widely available medical management option in the stable patient is procainamide.
Procainamide: Mechanism of action
- Procainamide is a class I antiarrhythmic that targets the AP
- Prolongs action potential duration in atrial and ventricular myocardium
- No AV nodal blocking effect
- Effective in both reversion, and in slowing ventricular rate
- Safe in children
- Bolus dose followed by infusion
The preferred long-term approach for patients with an AP and recurrent tachyarrhythmias is ablation.
EDExam Video WPW whiteboard session
ECG Examples
Example 1
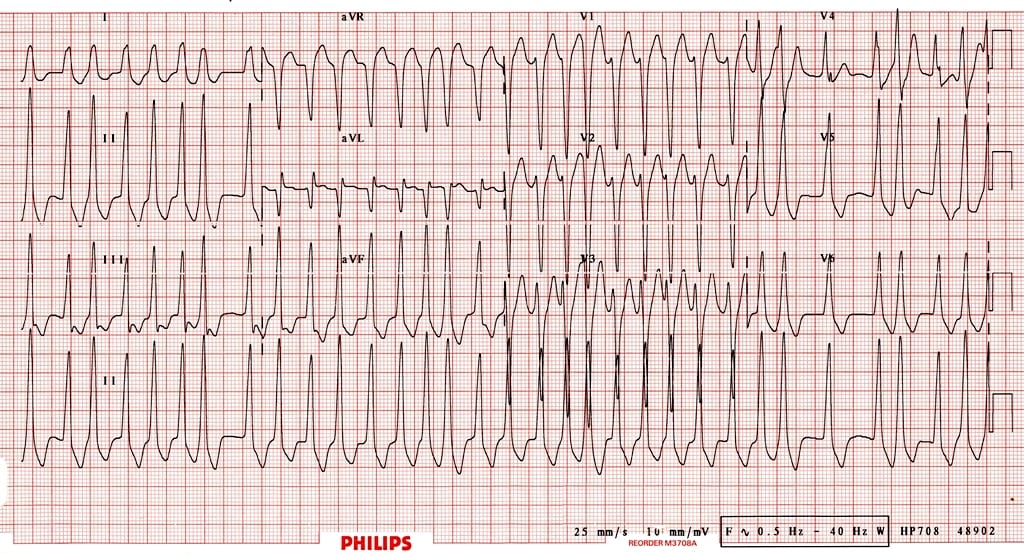
Atrial fibrillation in a patient with WPW:
- Rapid, irregular, broad complex tachycardia (overall rate ~ 200 bpm) with a LBBB morphology (dominant S wave in V1)
- This could easily be mistaken for AF with LBBB
- However, the morphology is not typical of LBBB, the rate is too rapid (up to 300 bpm in places, i.e. too rapid to be conducted via the AV node), and there is a subtle beat-to-beat variation in the QRS width which is more typical of WPW (LBBB usually has fixed width QRS complexes)
Example 2
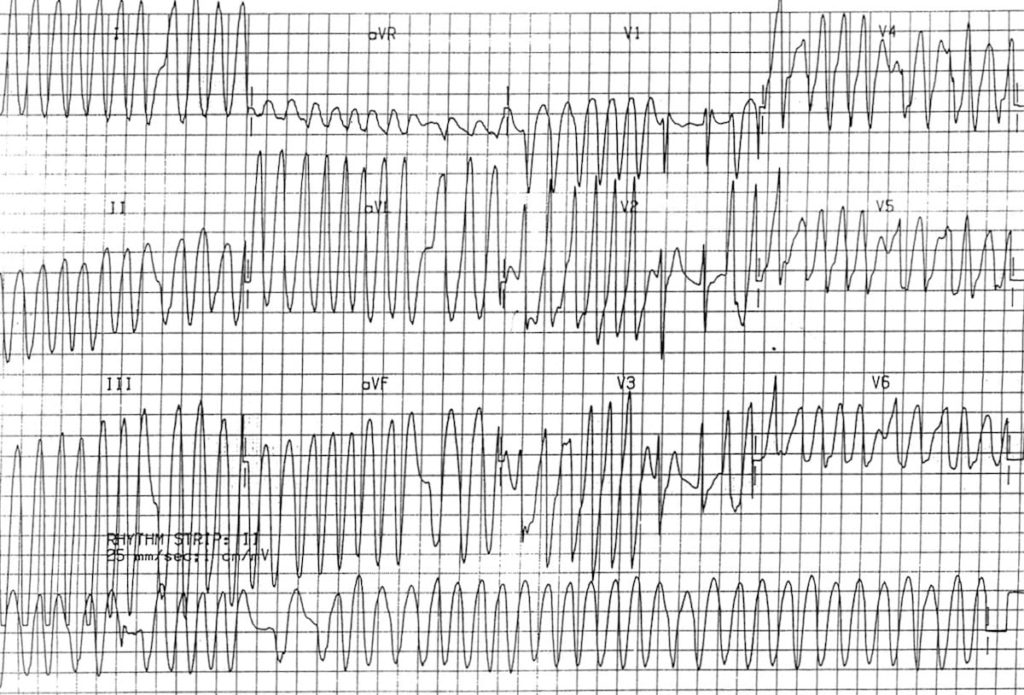
- Another example of AF with WPW resulting in a very rapid (up to 300 bpm in places), irregular broad-complex tachycardia with varying QRS width
- There are two narrow complexes (in V1-3), where the atrial impulses are presumably conducted via the AV node instead of via the AP
- This rhythm is extremely difficult to differentiate from polymorphic VT; however it does not demonstrate the twisting morphology characteristic of torsades de pointes
NB: Regardless of the aetiology, the most appropriate treatment for this rhythm (if sustained) would be immediate electrical cardioversion
Intermittent WPW
Example 3
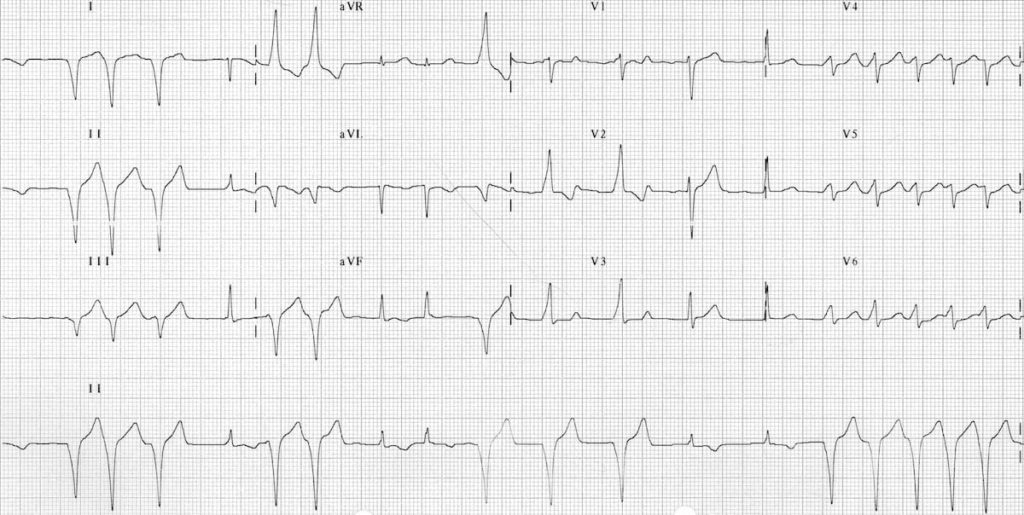
AF with WPW showing intermittent pre-excitation:
- Some of the impulses are transmitted via the AP (= pre-excited beats), producing characteristic delta waves
- Other impulses are transmitted via the AV node, producing narrow QRS complexes
Example 4
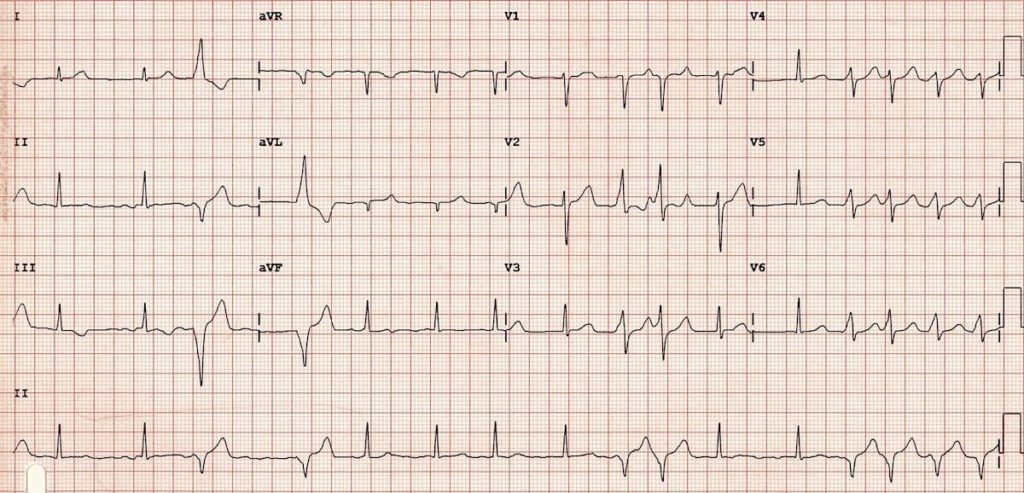
- Another example of AF with WPW with intermittent pre-excitation — characteristic delta waves are best seen in V2
Clinical Cases
- Top 100 ECG – Case 002
- Top 100 ECG – Case 038
- Top 100 ECG – Case 073
- Top 100 ECG – Case 092
- Top 100 ECG – Case 136
Related Topics
- Pre-excitation syndromes
- Pre-excitation with atrial fibrillation/flutter
- Atrioventricular Re-entry Tachycardia (AVRT)
- Supraventricular tachycardia
- VT versus SVT with aberrancy
- ECG Medical Training – WPW Syndrome Part 1
- ECG Medical Training – WPW Syndrome Part 2
Clinical Cases
- Top 100 ECG – Case 002
- Top 100 ECG – Case 038
- Top 100 ECG – Case 073
- Top 100 ECG – Case 092
- Top 100 ECG – Case 136
Related Topics
- Atrial fibrillation
- Atrial flutter
- Pre-excitation syndromes
- Atrioventricular Re-entry Tachycardia (AVRT)
- Supraventricular tachycardia
- VT versus SVT with aberrancy
- Wiesbauer F. Atrial Fibrillation Management Essentials. Medmastery
- ECG Medical Training – WPW Syndrome Part 1
- ECG Medical Training – WPW Syndrome Part 2
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library. Twitter: @rob_buttner


I’m having some difficulty with Example 3; AF with WPW showing intermittant pre-excitation. I was shown this ECG out of context and proceeded to use other methods to differentiate the abberant impulses listed in your article on differentiating SVT w/abberancy vs VT. I found the Axis of these impulses to be extreme (-90 to -150) with an initial R wave in aVR (Verecki) and the R-to-S nadir >100ms in v4-v6 (Brugada) – which are all said to suggest ventricular origin. After being corrected, I can see the purported delta-waves, but I’m curious how we definitively define these as delta-waves in the absence of PR interval to reference, and how can it be definitively distinguished from Josephson’s sign (with slurring but not notching)?