Atrioventricular Re-entry Tachycardia (AVRT)
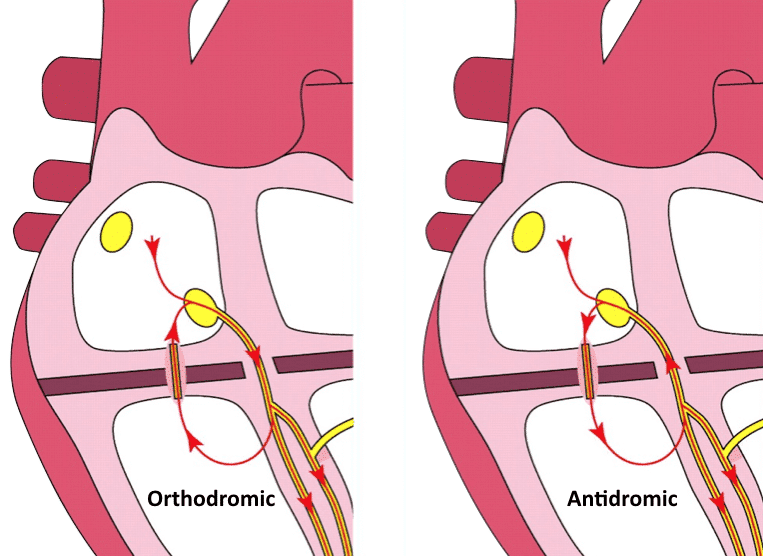
Atrioventricular Re-entry Tachycardia (AVRT) is a form of paroxysmal supraventricular tachycardia that occurs in patients with accessory pathways, usually due to formation of a re-entry circuit between the AV node and accessory pathway. ECG features depend on the direction of conduction, which can be orthodromic or antidromic.
Antidromic AVRT: Retrograde conduction through AV node
- In orthodromic AVRT, anterograde conduction is via the AV node, producing a regular narrow complex rhythm (in the absence of pre-existing bundle branch block)
- In antidromic AVRT, anterograde conduction is via the accessory pathway (AP), producing a regular wide complex rhythm. This can be difficult to distinguish from ventricular tachycardia (VT)
- Often triggered by premature atrial or premature ventricular beats
- In both forms, the features of pre-excitation are lost
Tachyarrhythmias in pre-excitation can also be facilitated by direct conduction from the atria to the ventricles via the AP, bypassing the AV node. This is seen with atrial fibrillation or atrial flutter in conjunction with WPW, and is discussed further here.
Orthodromic AVRT
In orthodromic AVRT, anterograde conduction occurs via the AV node, resulting in a normal direction of ventricular depolarisation. This can occur in patients with a concealed pathway (AP that conducts retrograde only, not evident on sinus rhythm ECG).
ECG features of AVRT with orthodromic conduction:
- Rate usually 200-300 bpm
- Retrograde P waves are usually visible, with a long RP interval
- QRS < 120ms unless pre-existing bundle branch block, or rate-related aberrant conduction
- QRS alternans: phasic variation in QRS amplitude associated with AVNT and AVRT, distinguished from electrical alternans by a normal QRS amplitude
- Rate-related ischaemia is common
Orthodromic AVRT, or just AVNRT?
This rhythm can appear very similar to AVNRT, but the RP interval can assist us to differentiate:
- In typical AVNRT, retrograde P waves occur early, so we either don’t see them (buried in QRS) or partially see them (pseudo R’ wave at terminal portion of QRS complex)
- In AVRT, retrograde P waves occur later, with a long RP interval > 70 msec
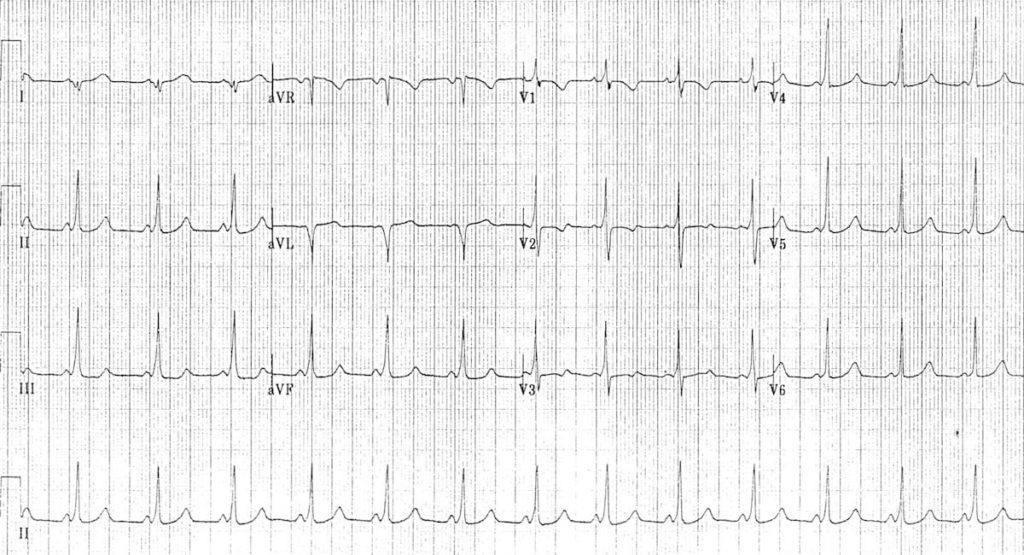
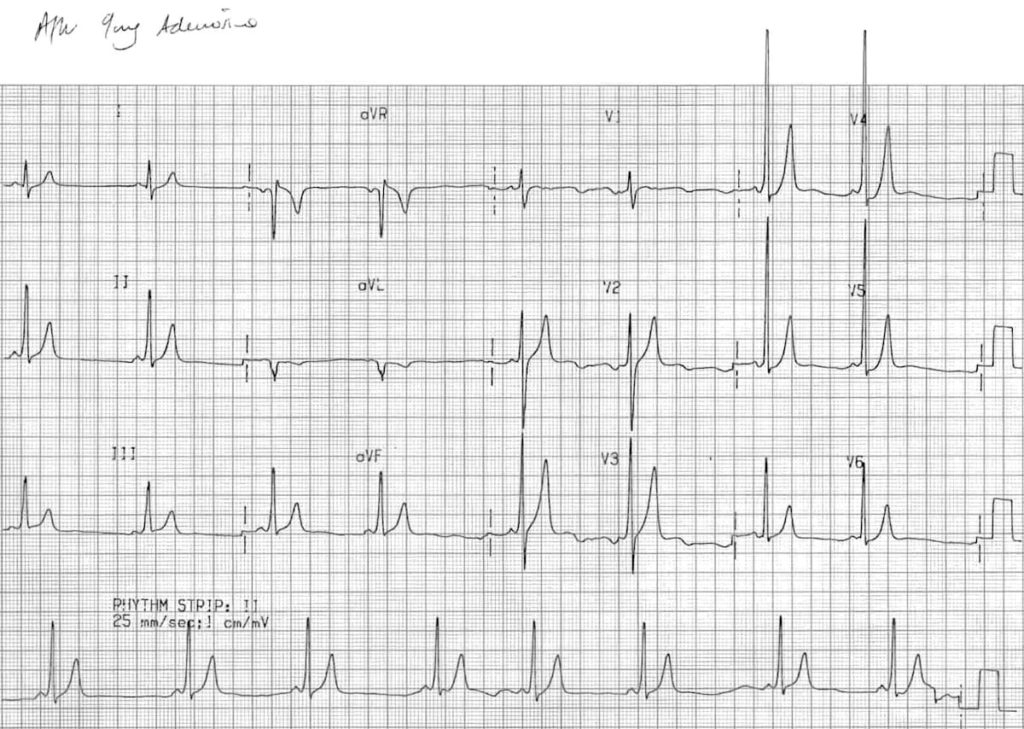
In the above example, look closely at V1 — P waves are evident as a small notch at the beginning of the T wave, with a long RP interval, indicating this is likely orthodromic AVRT.
Fortunately, treatment is fairly similar for both.
Treatment of orthodromic AVRT
- As always, patients that are unstable due to this rhythm require urgent DC cardioversion
- The anterograde portion of conduction is typically the “weak link” of the re-entry circuit. Management options in the stable patient therefore target slowing conduction through the AV node
- A stepwise approach similar to AVNRT can be employed, beginning with vagal manoeuvres followed by adenosine and/or verapamil
Note that with administration of any AV nodal blocking drug, there is a very small but significant risk of inducing AF. If verapamil is used, patients should be observed for at least 4 hours to ensure AF does not develop as a consequence of AV nodal blockade
See what happened when our patient above was given adenosine
Antidromic AVRT
Antidromic AVRT is rare, and makes up only 5% of tachyarrhythmias in patients with WPW. As the name suggests, it involves anterograde conduction via the AP. Retrograde conduction is usually via the AV node, but can also be via another AP. The abnormal direction of ventricular depolarisation results in a broad complex tachycardia, which can be easily mistaken for VT.
ECG features of AVRT with antidromic conduction:
- Rate usually 200-300 bpm
- Wide QRS complexes due to abnormal ventricular depolarisation via AP
Treatment of antidromic AVRT
- This rhythm can be difficult to distinguish from VT, and if there is any doubt, we should presume a diagnosis of VT and treat accordingly
- In stable patients, drug therapy should be targeted at the AP
- Procainamide (class I) would be our first line antiarrhythmic. Ibutilide (class III) and amiodarone are second-line options, but their effectiveness is less established
- DC cardioversion may still be required if drug therapy fails
The re-entry circuit involves the AV node — why can’t we use AV nodal blocking agents?
- Antidromic AVRT is often associated with a rapidly conducting anterograde AP
- AV blockade through adenosine may interrupt this re-entry circuit, but as stated above, with administration of any AV nodal blocking agent there is a small risk of inducing AF
- If this occurs it will likely precipitate cardiac arrest due to rapid conduction via the AP
- As such, in a stable patient drug therapy should be targeted at the AP
For discussion on differentiating wide complex tachycardias see here, here, and here
More ECG Examples
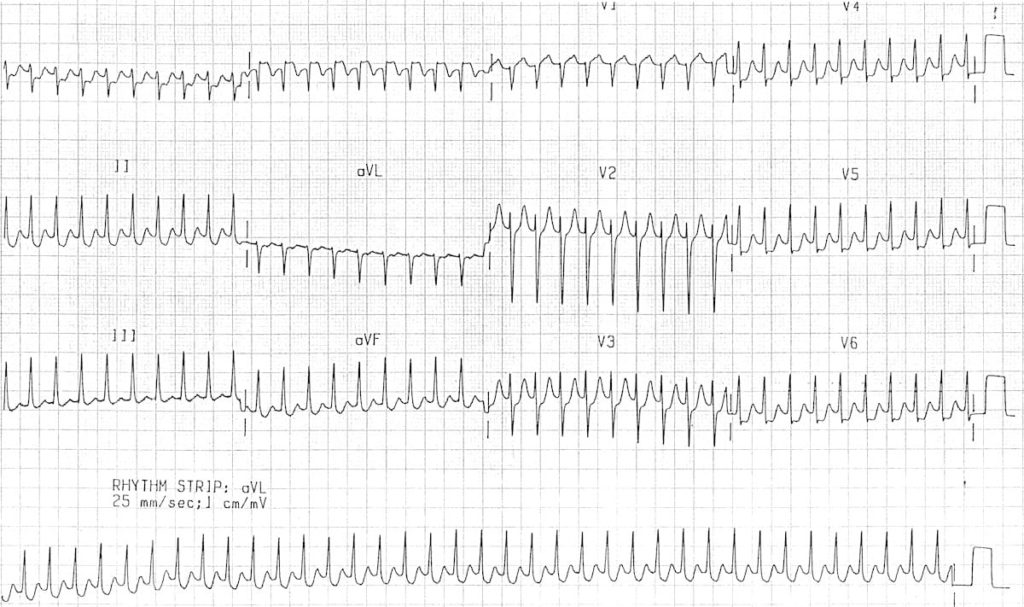
Example 1A
Orthodromic AVRT:
- Regular, narrow complex tachycardia at 180 bpm
- The QRS complexes are narrow because impulses are being transmitted in an orthodromic direction (A -> V) via the AV node
- Retrograde P waves are visible in V1 (see first beat), and quite clearly in lead III (notch at beginning of T wave), with a long RP interval
Example 1B
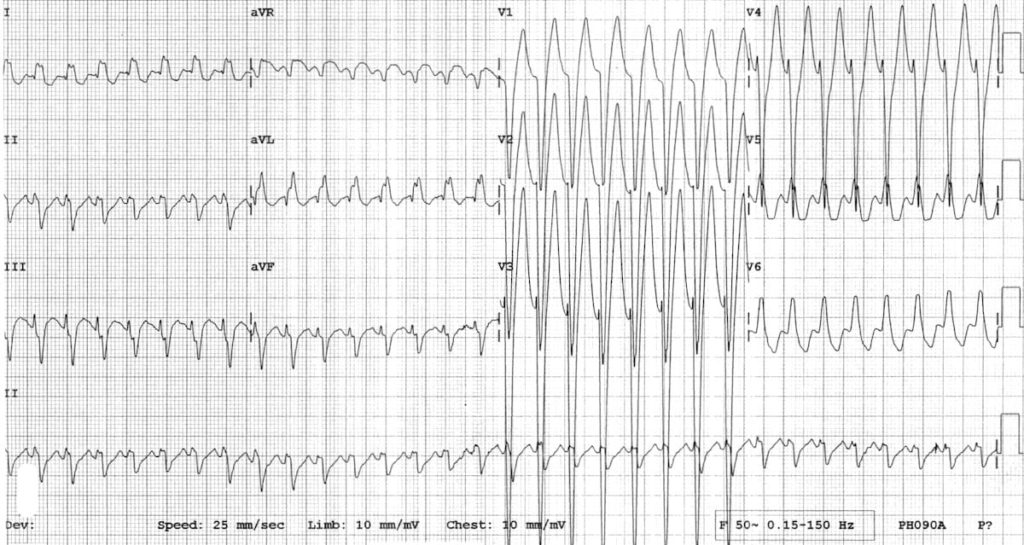
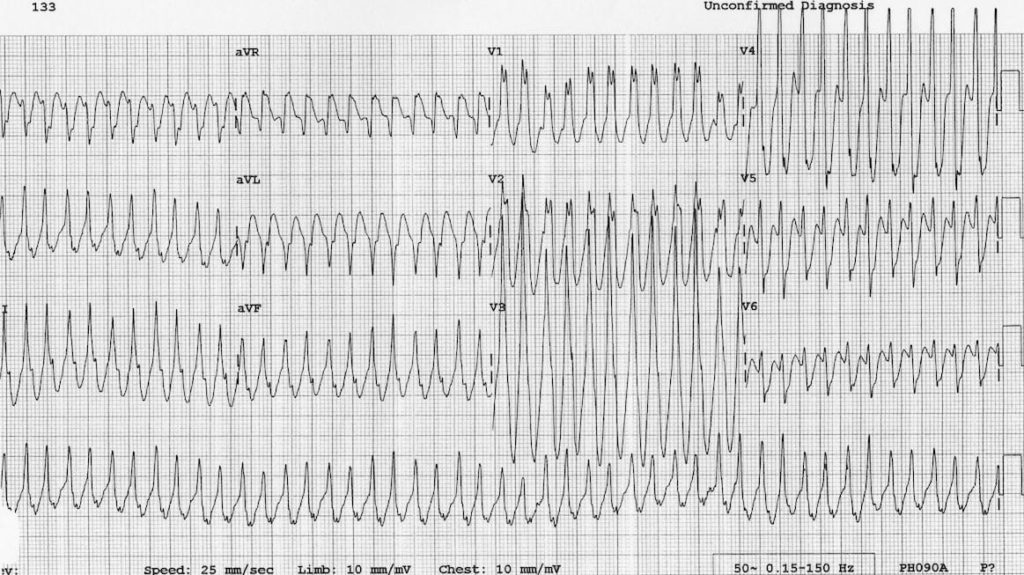
Example 2A
Antidromic AVRT in a 5-year old boy with WPW:
- Regular, broad complex tachycardia at ~280 bpm; this would be very difficult to distinguish from VT
- However, given the child’s age, VT is very unlikely: > 95% of broad complex tachycardias in children are actually some form of SVT with aberrancy
- This rhythm resolved with vagal manoeuvres
Read more about differentiating VT from SVT with aberrancy.
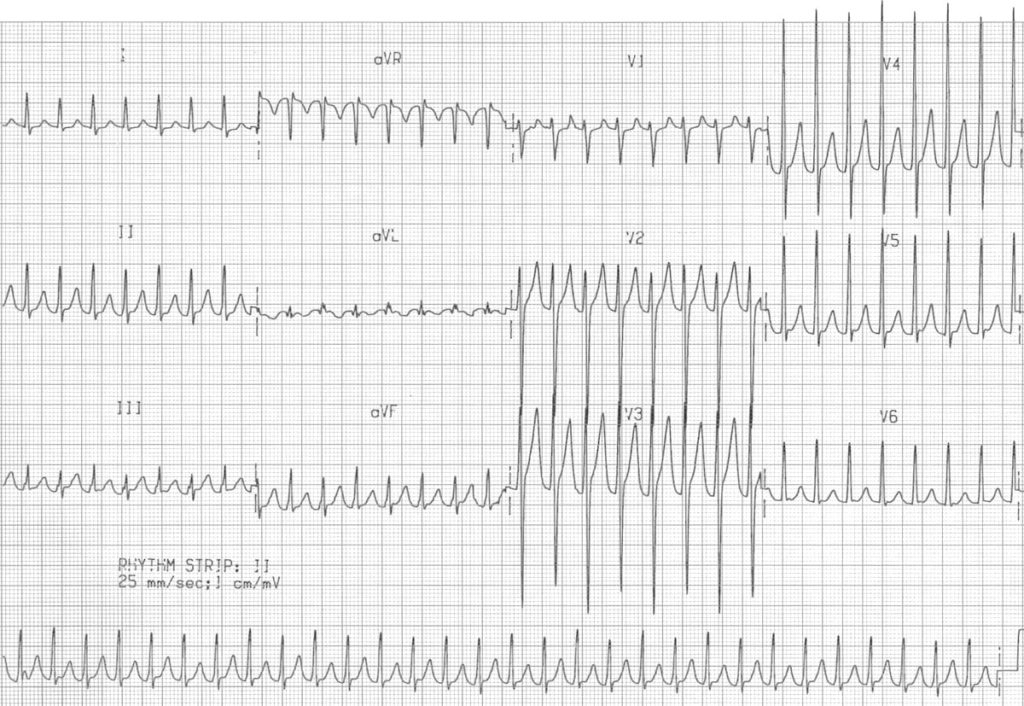
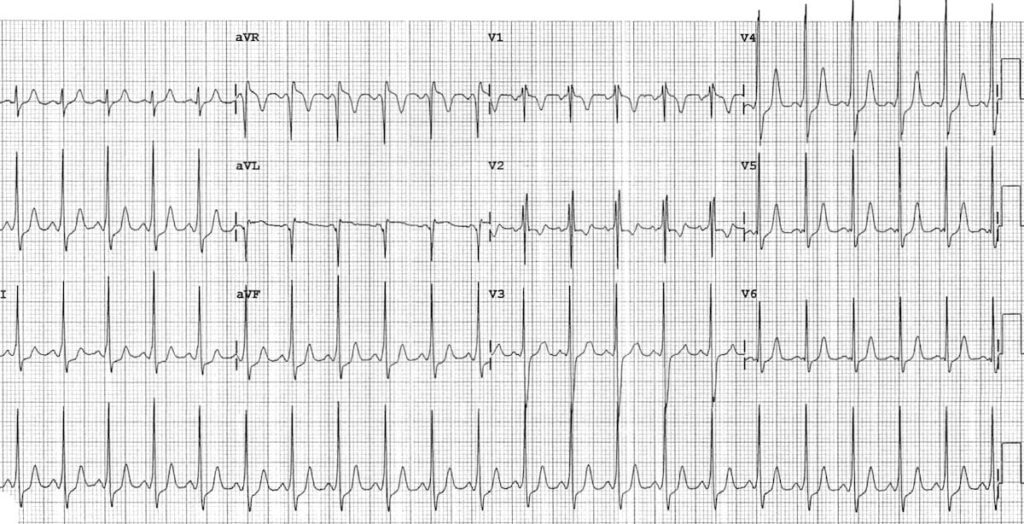
Example 2B
Baseline ECG of the same patient — note that ECG changes are more subtle than in adults:
- PR interval is short even allowing for the patient’s age
- The QRS complexes do not appear particularly broad — however, there is definite slurring of the upstroke of each R wave, most obvious in inferior leads
- The RSR’ pattern with T wave inversion in V1-2 is a normal variant in children of this age; this is still a Type B pattern due to absence of a dominant R wave in V1
- There are pseudo-infarction Q waves in lead aVL simulating lateral infarction
For more information on interpretation of the paediatric ECG, check out our Guide to Paediatric ECG Interpretation.
Clinical Cases
- Top 100 ECG – Case 002
- Top 100 ECG – Case 038
- Top 100 ECG – Case 073
- Top 100 ECG – Case 092
- Top 100 ECG – Case 136
Related Topics
- Pre-excitation syndromes
- Pre-excitation with atrial fibrillation/flutter
- Atrioventricular Re-entry Tachycardia (AVRT)
- Supraventricular tachycardia
- VT versus SVT with aberrancy
- ECG Medical Training – WPW Syndrome Part 1
- ECG Medical Training – WPW Syndrome Part 2
Clinical Cases
- Top 100 ECG – Case 002
- Top 100 ECG – Case 038
- Top 100 ECG – Case 073
- Top 100 ECG – Case 092
- Top 100 ECG – Case 136
Related Topics
- Pre-excitation syndromes
- Pre-excitation with atrial fibrillation/flutter
- Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
- Supraventricular tachycardia
- VT versus SVT with aberrancy
- ECG Medical Training – WPW Syndrome Part 1
- ECG Medical Training – WPW Syndrome Part 2
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner