Bifascicular Block
Diagnostic criteria
Clinically, bifascicular block presents with one of two ECG patterns:
*Some authors describe Left bundle branch block (LBBB) as a bifascicular block, as it may indicate LAFB + LPFB. However, clinically the term bifascicular block is reserved for RBBB with either LAFB or LPFB
Electrophysiology
Bifascicular block involves conduction delay below the atrioventricular node in two of the three fascicles:
- Conduction to the ventricles is via the single remaining fascicle
- The ECG will show typical features of RBBB plus either left or right axis deviation.
- RBBB + LAFB is the most common of the two patterns. This is due to a single coronary artery blood supply (LAD) to the anterior fascicle
- RBBB + LPFB is less common due to a dual blood supply (right and left circumflex arteries), and this combination may be associated with more extensive underlying cardiac pathology

Clinical significance
Bifascicular block is often associated with structural heart disease (50-80%) and extensive fibrosis of the conducting system. There is a risk of progression to complete heart block with additional damage to the third remaining fascicle, however clinical context is important:
- Overall rate of progression to complete heart block is 1-4% per year
- In symptom free patients, these figures are ~1% per year
- Patients presenting with syncope have a 17% annual risk of progression
- Syncope or presyncope in the context of a bifascicular block is an indication for admission and monitoring. If other causes of syncope are not identified on work-up, pacemaker insertion is recommended
Main Causes of Bifascicular Block
Causes are similiar to those of RBBB and LAFB/LPFB:
- Ischaemic heart disease (40-60% cases)
- Structural heart disease (50-80% association)
- Aortic stenosis
- Anterior MI (occurs in 5-7% of acute AMI)
- Lenègre-Lev disease
- Congenital heart disease
- Hyperkalaemia (resolves with treatment)
A new-onset bifascicular block in the context of chest pain is highly associated with proximal LAD occlusion, even in the absence of ST-segment changes. In 30% of cases, patients present with no ST elevation and bifascicular block is the only acute ECG finding.
Differential diagnosis
- Masquerading Bundle Branch Block (MBBB) presents with a mixed complete RBBB and complete LBBB pattern similar to a typical bifascicular block pattern. This rare ECG pattern indicates more extensive fibrosis of the conducting system and limited studies demonstrate a poorer prognosis and higher progression to complete heart block
- In the context of RBBB, RAD indicating LPFB may be due to other causes such as right ventricular hypertrophy, and these need to be excluded before the ECG is labelled bifascicular block
ECG examples
Example 1
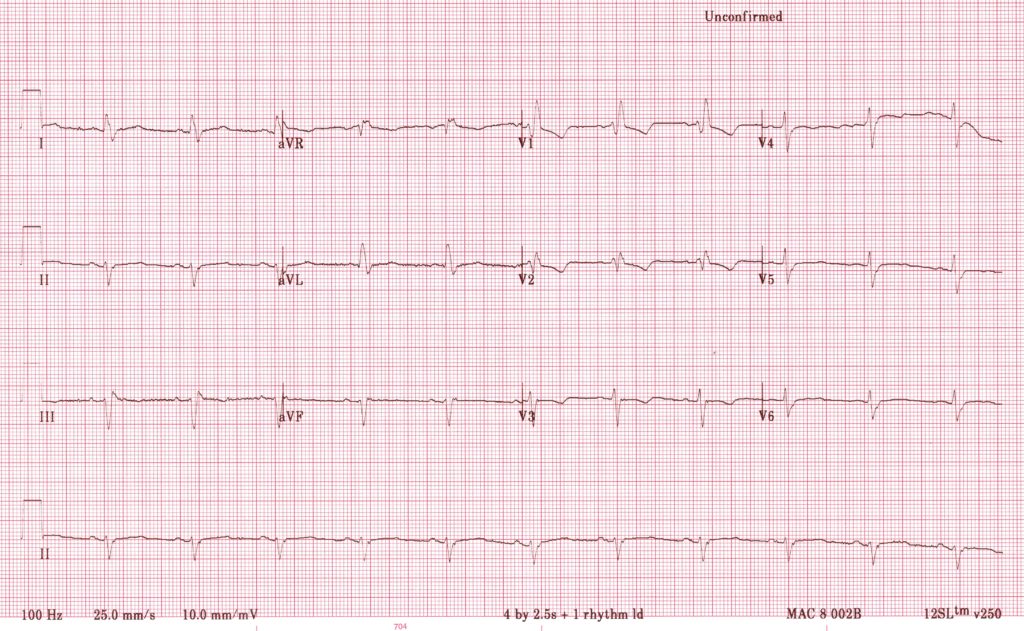
RBBB with LAFB
- RBBB pattern in precordial leads with RSR’ complex in V1-2
- Prominent LAD indicating LAFB
Example 2
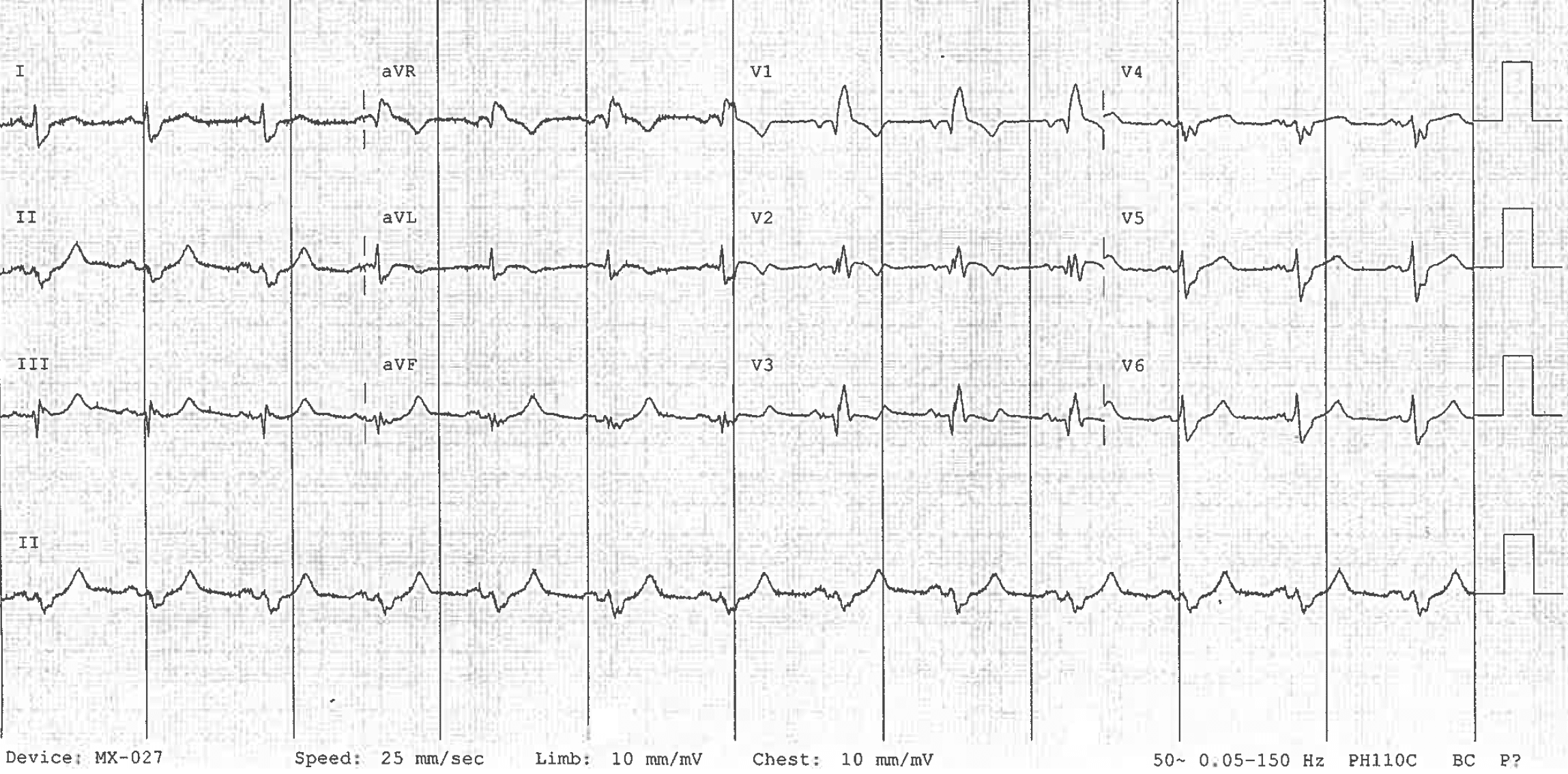
RBBB with LAFB, in the context of chest pain
- RBBB is seen with RSR’ pattern in V1-3 and slurred S waves in lateral leads
- There are concordant ST segment changes best seen in V2, and hyper-acute T waves inferiorly.
- This patient was found to have a 99% proximal LAD occlusion. See OMI: Replacing the STEMI misnomer for further case details
Example 3a
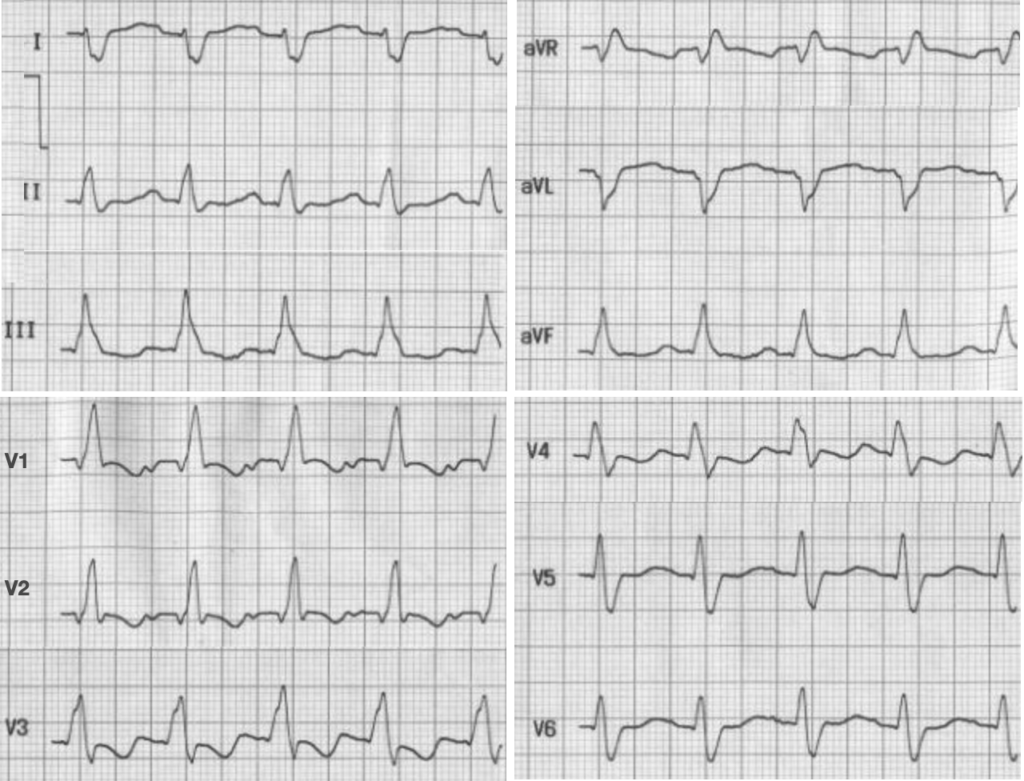
RBBB with LPFB
- RBBB with wide QRS, slurred S wave in lead I and slurred R in V1.
- Right axis deviation (dominant negative deflection in leads I and aVl) with dominant positive deflection in aVf along with rS pattern in lead I and qR pattern leads III and aVf, suggesting left posterior fascicular block.
Example 3b
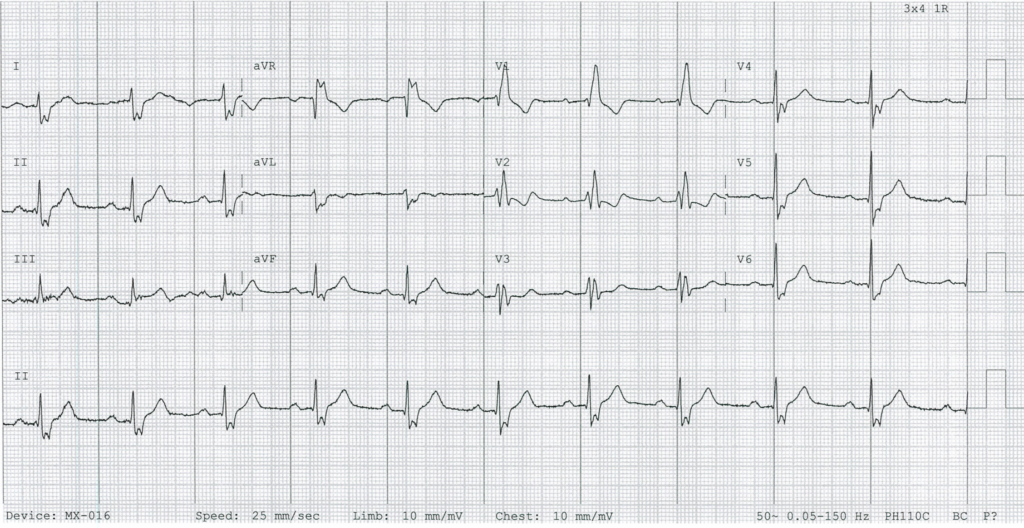
RBBB with LPFB and RAD
Related Topics
- Left anterior fascicular block
- Left bundle branch block
- Left posterior fascicular block
- Right bundle branch block
- Trifascicular block
References
- Olshansky B. Bradyarrhythmias – Conduction System Abnormalities. In: Arrhythmia Essentials 2e, 2017.
- Vijayaraman P. Clinical Cardiac Pacing, Defibrillation and Resynchronisation Therapy 5e, 2017
- Goldberger A. Ventricular Conduction Disturbances.. In: Goldberger’s Clinical Electrocardiography 9e, 2018.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner

