Difficult Airway Algorithms
OVERVIEW
- Difficult airway algorithms are useful for considering all the contingencies that may occur during intubation
- All team members must be aware of all of the contingency plans
- All intubation attempts should be considered potential difficult airways
- Algorithms involve a step-wise approach using different techniques for difficult intubation and difficult ventilation
TECHNIQUES
Techniques for difficult intubation
- Alternative laryngoscope blades
- Awake intubation (either video laryngoscope or fiberoptic scope)
- Blind intubation (oral or nasal)
- Fiberoptic intubation
- Intubating stylet or tube changer (e.g. Cook catheter or bougie)
- Laryngeal mask airway as an intubating conduit
- Light wand
- Retrograde intubation
- Invasive airway access
Techniques for Difficult Ventilation
- Esophageal tracheal Combitube
- Intratracheal jet stylet
- Laryngeal mask airway
- Oral and nasopharyngeal airways
- Rigid ventilating bronchoscope
- Invasive airway access
- Transtracheal jet ventilation
- Two-person mask ventilation

Patient safety using RSI hinges on a redundancy of safety.
- Can you intubate? If intubation fails, can you ventilate? Algorithm (above) focuses on the route of intubation and RSI decision.
The colored arrows are contraindications to RSI.
- In cardiac arrest (blue box – patient apneic) muscle relaxants are not needed. When there is obvious oral pathology, or intrinsic laryngo-tracheal pathology (green boxes – patient breathing spontaneously), the redundancy of safety does not exist – avoid RSI.
- When the mouth is blocked (step 2), intubate through the nose or through the neck (cricothyroidotomy). RSI is specifically done to optimize laryngoscopy conditions and permit oral intubation. If it is apparent that the oral route has obvious anatomic problems (not merely potential difficulty), RSI should never be considered.
- When the oral route is impossible, intubation will need to take place through the nose or neck, and this should be done with the patient awake.
- Examples include massive angioedema, advanced Lundwig’s angina, wired jaw, or readily apparent combinations of airway distortion, disproportion, and dysmobility (cervical spine and mandible), that preclude oral intubation. With intrinsic laryngeal pathology (step 3), safest approach is with the patient breathing spontaneously, using fiberoptic intubation, or a surgical airway (tracheotomy) below the level of the lesion.
At step 4, the decision to use RSI is a matter of judgment, not a strict contraindication.
- The four Ds (distortion, disproportion, dysmobility, dentition) may make direct laryngoscopy with standard equipment impossible.
- Is an “awake” approach feasible? Will you be able to rescue ventilate? How fast are intubation and patient control needed? What are the risks of delay vs. the potential risks of RSI?
After crossing the RSI line, patient safety often depends on first pass success at laryngoscopy, since many patients requiring emergent intubation have very short safe apneic periods.
- Pre-oxygenation is only marginally effective in critically ill patients.
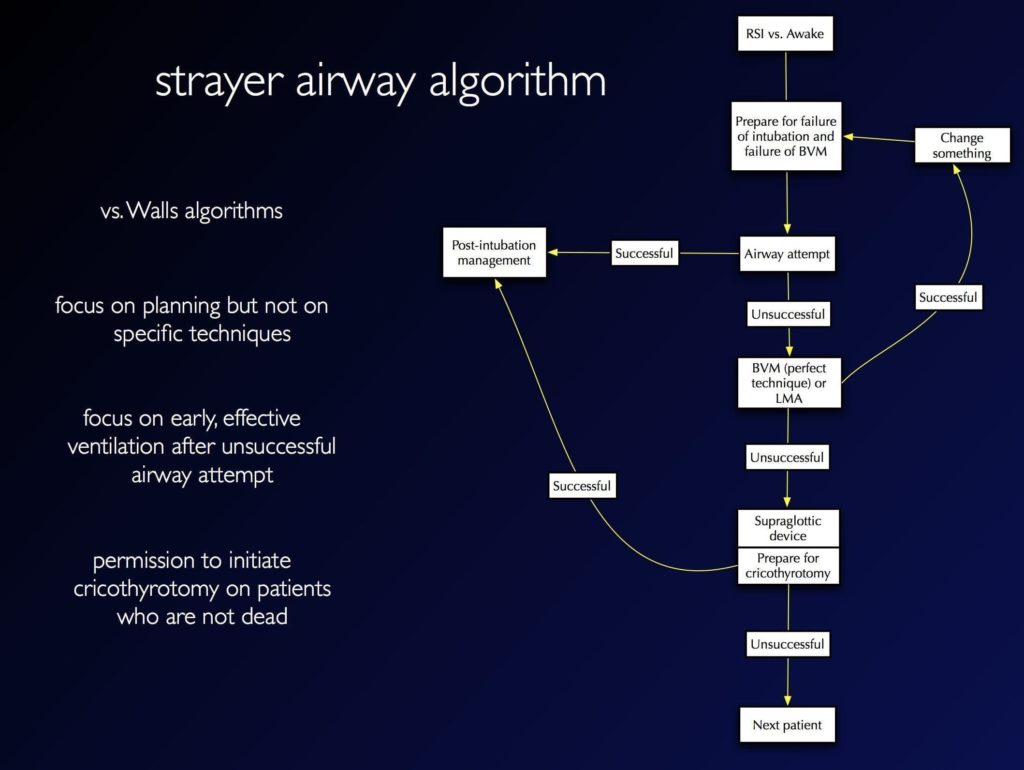
STRAYER AIRWAY ALGORITHM
- RSI vs. Awake – latter preferred if:
- Less urgent intubation
- More difficult airway features
- Low risk of vomiting
- Prepare for failure of intubation and failure of ventilation
- Discuss plan A, B, C, D with team
- Equipment for plan A, B, C, D at bedside
- Airway attempt successful -> post-intubation management
- Airway attempt unsuccessful, able to ventilate -> Plan B/C/D
- change patient position
- change blade
- change modality (e.g. direct vs video laryngoscopy)
- change proceduralist
- Airway attempt unsuccessful, unable to ventilate -> supraglottic airway -> surgical airway if unsuccessful -> post-intubation management
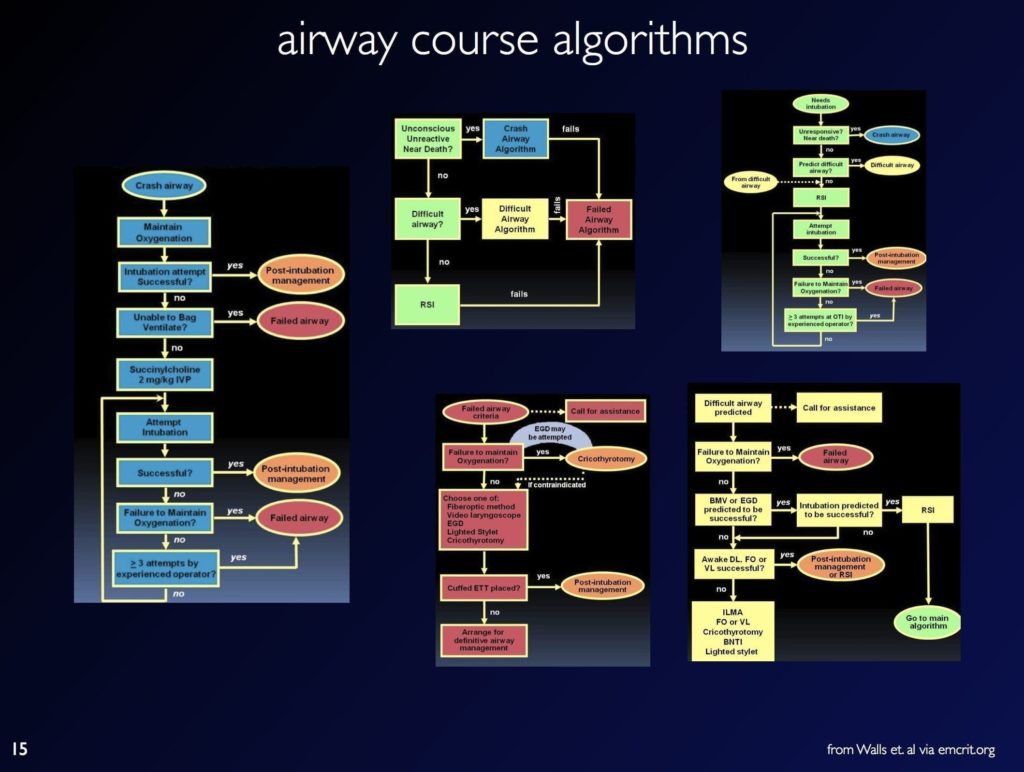
WALLS AIRWAY ALGORITHMS
Ron Wall’s algorithms from his Airway Course and Manual of Emergency Airway Management:
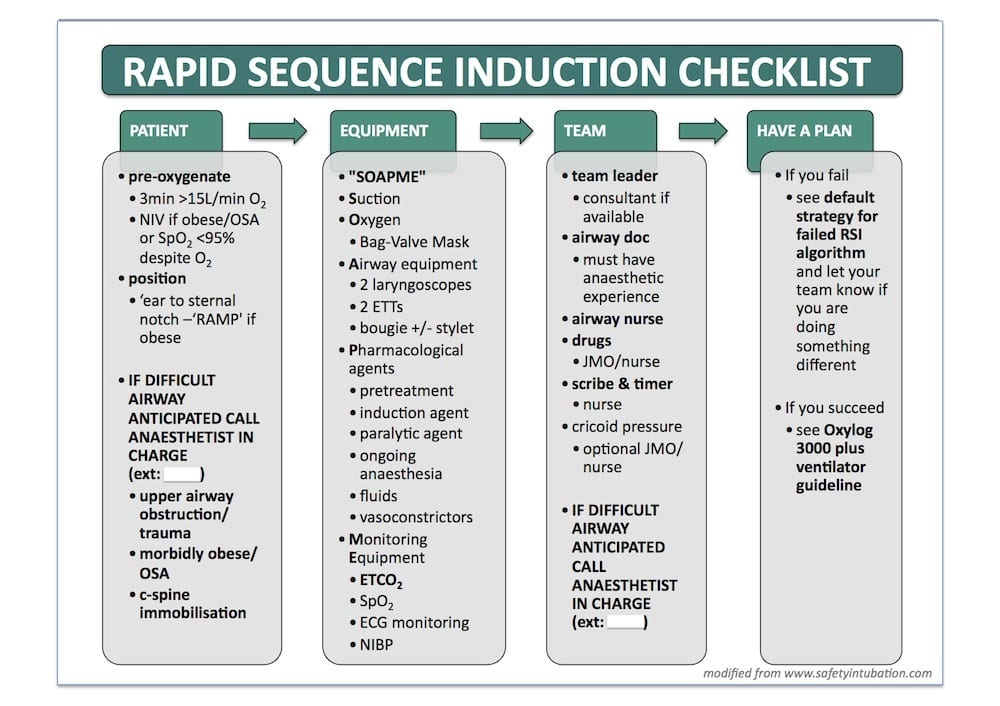
AUSTIN HOSPITAL AIRWAY ALGORITHMS
Algorithms from the Austin Hospital ED, Melbourne, courtesy of George Douros. Here’s the RSI pre-intubation checklist
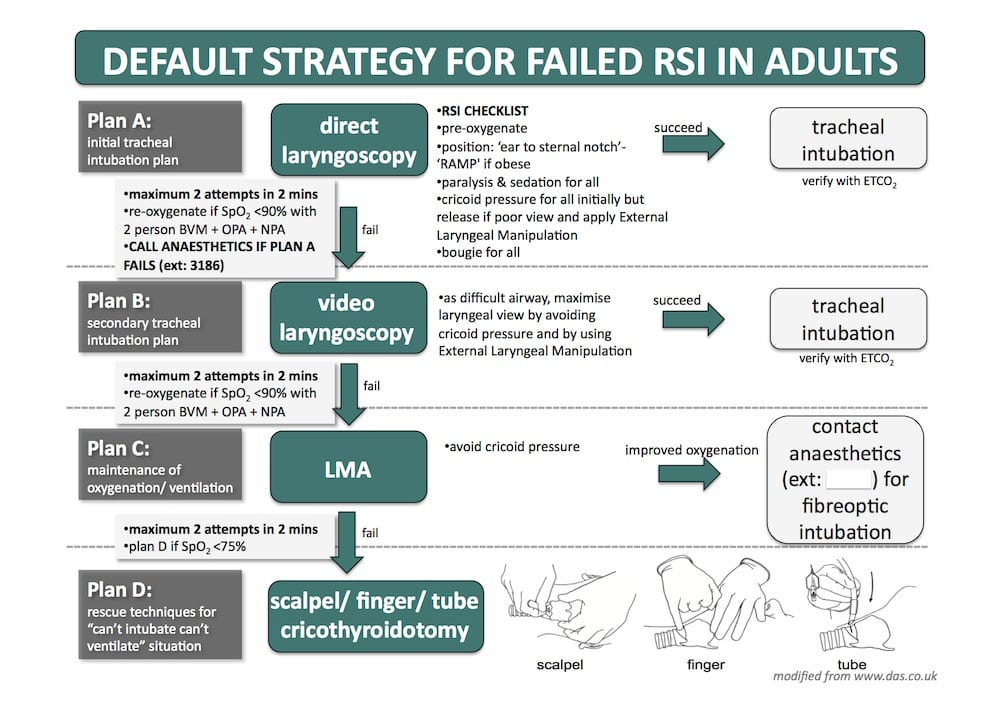
Here’s the difficult airway action plan
THE VORTEX APPROACH
Nicholas Chrimes and Peter Fritz have developed an algorithmic approach to airway management based on a cognitive aid called ‘The Vortex’
DIFFICULT AIRWAY SOCIETY ALGORITHM
The Difficult Airway Society in the UK has comprehensive guidelines for airway management, including multiple algorithms.
- The integrated algorithm can be downloaded here (pdf).
- the Austin Hospital’s algoirthm by George Douros above, is a modified version of the DAS integrated algorithm – note that the option of waking the patient up has been removed for ‘out-of-theatre’ use!
References and Links
CCC Airway Series
Emergencies: Can’t Intubate, Can’t Intubate, Can’t Oxygenate (CICO), Laryngospasm, Surgical Cricothyroidotomy
Conditions: Airway Obstruction, Airway in C-Spine Injury, Airway mgmt in major trauma, Airway in Maxillofacial Trauma, Airway in Neck Trauma, Angioedema, Coroner’s Clot, Intubation of the GI Bleeder, Intubation in GIH, Intubation, hypotension and shock, Peri-intubation life threats, Stridor, Post-Extubation Stridor, Tracheo-esophageal fistula, Trismus and Restricted Mouth Opening
Pre-Intubation: Airway Assessment, Apnoeic Oxygenation, Pre-oxygenation
Paediatric: Paediatric Airway, Paeds Anaesthetic Equipment, Upper airway obstruction in a child
Airway adjuncts: Intubating LMA, Laryngeal Mask Airway (LMA)
Intubation Aids: Bougie, Stylet, Airway Exchange Catheter
Intubation Pharmacology: Paralytics for intubation of the critically ill, Pre-treatment for RSI
Laryngoscopy: Bimanual laryngoscopy, Direct Laryngoscopy, Suction Assisted Laryngoscopy Airway Decontamination (SALAD), Three Axis Alignment vs Two Curve Theory, Video Laryngoscopy, Video Laryngoscopy vs. Direct
Intubation: Adverse effects of endotracheal intubation, Awake Intubation, Blind Digital Intubation, Cricoid Pressure, Delayed sequence intubation (DSI), Nasal intubation, Pre-hospital RSI, Rapid Sequence Intubation (RSI), RSI and PALM
Post-intubation: ETT Cuff Leak, Hypoxia, Post-intubation Care, Unplanned Extubation
Tracheostomy: Anatomy, Assessment of swallow, Bleeding trache, Complications, Insertion, Insertion timing, Literature summary, Perc. Trache, Perc. vs surgical trache, Respiratory distress in a trache patient, Trache Adv. and Disadv., Trache summary
Misc: Airway literature summaries, Bronchoscopic Anatomy, Cuff Leak Test, Difficult airway algorithms, Phases of Swallowing
Journal articles
- Apfelbaum JL, et al; American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013 Feb;118(2):251-70. PMID: 23364566. [Free Full Text]
- Henderson JJ, Popat MT, Latto IP, Pearce AC; Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004 Jul;59(7):675-94. PMID: 15200543.
FOAM and web resources
- Airwaycam.com — Algorithms for Emergency Airway Management
- DIFFICULT AIRWAY SOCIETY (United Kingdom) GUIDELINES
- DAS — Update on new DAS Guidelines 2015
- EMCrit Podcast 47 – Failure to Plan for Failure: A Discussion of Airway Disasters
- EMCrit 92 — EMCrit Intubation Checklist
- Emergency Medicine Updates — Emergency Department Intubation Checklist v13 (2012)
- Emergency Medicine Updates — ED Procedural Sedation and Analgesia Checklist
- Own the Airway! (LITFL collection of online airway videos)
- Project Check — Checklist for Checklist Development
- Resus.ME — Anaesthesia’s dirty laundry – let’s all learn from it
- Resus.ME — Inutbation checklist
- The Vortex Approach
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
