Rapid Sequence Intubation (RSI)
Reviewed and revised 18 June 2015
OVERVIEW
- Rapid sequence intubation (RSI) is an airway management technique that produces inducing immediate unresponsiveness (induction agent) and muscular relaxation (neuromuscular blocking agent) and is the fastest and most effective means of controlling the emergency airway
- the cessation of spontaneous ventilation involves considerable risk if the provider does not intubate or ventilate the patient in a timely manner
- RSI is particularly useful in the patient with an intact gag reflex, a “full” stomach, and a life threatening injury or illness requiring immediate airway control
- ‘modified’ RSI is a term sometimes used to describe variations on the ‘classic’ RSI approach (e.g. ventilation during apnea, titration of induction agents); modified approaches tend to trade an increased risk of aspiration for other benefits (e.g. prevent respiratory acidosis due to apnea from compounding severe metabolic acidosis)
INDICATIONS FOR INTUBATION AND MECHANICAL VENTILATION
Indications
- A – airway protection and patency
- B – respiratory failure (hypercapnic or hypoxic), increase FRC, decrease WOB, secretion management/ pulmonary toilet, to facilitate bronchoscopy
- C – minimise oxygen consumption and optimize oxygen delivery (e.g. sepsis)
- D – unresponsive to pain, terminate seizure, prevent secondary brain injury
- E — temperature control (e.g. serotonin syndrome)
- F — For humanitarian reasons (e.g. procedures) and for safety during transport (e.g. psychosis)
The decision to perform RSI in the ‘out of theatre’ setting involves weighing the pros and cons:
FOR RSI
- Lack of airway protection despite patency (swallow, gag, cough, positioning , and tone)hypoxia
- hypoventilation
- need for neuroprotection (e.g. target PaCO2 35-40 mmHg)
- impending obstruction (e.g. airway burn, penetrating neck injury)
- prolonged transfer
- combativeness
- humane reasons (e.g. major trauma requiring multiple interventions)
- cervical spine injury (diaphragmatic paralysis)
AGAINST RSI
- urgent need to OT and theatre is available anatomically or pathologically difficult airway (e.g. congenital deformity, laryngeal fracture)
- close proximity to OT
- paediatric cases (especially <5 years of age)
- hostile environment
- poorly functioning team
- lack of requisite skills among team
- emergency surgical airway is not possible (e.g. neck trauma, tumour)
FACTORS THAT MAKE EMERGENCY INTUBATION DIFFICULT
RSI is useful if the following are present (from Richard Levitan’s Airwaycam.com):
- Dynamically deteriorating clinical situation, i.e., there is a real “need for speed”
- Non-cooperative patient
- Respiratory and ventilatory compromise
- Impaired oxygenation
- Full stomach (increased risk of regurgitation, vomiting, aspiration)
- Extremely short safe apnea times
- Secretions, blood, vomitus, and distorted anatomy
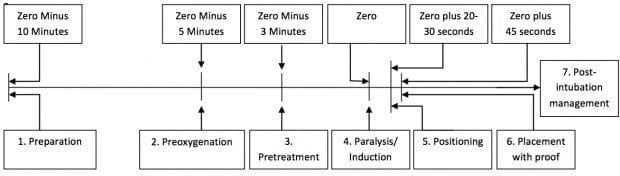
PROCESS OF RSI
Remembered as the 9Ps:
- Plan
- Preparation (drugs, equipment, people, place)
- Protect the cervical spine
- Positioning (some do this after paralysis and induction)
- Preoxygenation
- Pretreatment (optional; e.g. atropine, fentanyl and lignocaine)
- Paralysis and Induction
- Placement with proof
- Postintubation management
Some add a 10th P for (cricoid) pressure after pretreatment but this procedure is optional and has many drawbacks (see Cricoid Pressure)
Ideally, minimise instrumentation and suctioning prior to intubation to avoid stimulation of the patient’s gag reflex.
ROLES DURING RSI
The airway team should be a minimum of 3 people:
- airway proceduralist
- airway assistant
- drug administrator
The team leader may perform one of the above roles if necessary, but should ideally be a separate stand alone role.
Other roles include:
- person to perform MILS if indicated
- person to perform cricoid pressure (if deemed necessary)
- scribe
In the event of a failed airway, another person may take on the role of the airway proceduralist and role re-allocation must be clearly communicated to the team.
PREPARATION FOR RSI
Preparation requires control over:
- self
- patient
- others
- environment
Maintain a ‘sterile cockpit environment’ when communicating the airway plan to the team, ideally through use of a ‘call and response’ checklist— otherwise one of these two mnemonics will help:
- SOAPME
- O2 MARBLES
SOAPME
- Suction
— at least one working suction, place it between mattress and bed - Oxygen
— NRBM and BVM attached to 15 LPM of O2, preferably with nasal prongs for apneic oxygenation - Airways
— 7.5 ET tube with stylet fits most adults, 7.0 for smaller females, 8.0 for larger males, test balloon by filling with 10 cc of air with a syringe
— Stylet – placed inside ET tube for rigidity, bend it 30 degrees starting at proximal end of cuff (i.e. straight to cuff, then 30 degree bend)
— Blade – Mac 3 or 4 for adults – curved blade
— Miller 3 or 4 for adults – straight blade
— Handle – attach blade and make sure light source works
— Backups – ALWAYS have a surgical cric kit available!
— have video laryngoscope, LMA and bougie at bedside - Pre-oxygenate – 15 LPM NRBM
- Monitoring equipment/Medications
— Cardiac monitor, pulse ox, BP cuff opposite arm with IV
— Medications drawn up and ready to be given - End Tidal CO2
O2 MARBLES is an alternative for the equipment and planning:
- Oxygen
- masks (NP, NRB, BVM); monitoring
- airway adjuncts (e.g. OPA, NPA, LMA); Ask for help and difficult airway trolley
- RSI drugs; Resus drugs
- BVM; Bougie
- Laryngoscopes; LMA
- ETTs; ETCO2
- Suction; State Plan
IDEAL RSI INDUCTION AGENT
Does not exist (unfortunately!), but if it did it would:
- smoothly and quickly render the patient unconscious, unresponsive and amnestic in one arm/heart/brain circulation time
- provide analgesia
- maintain stable cerebral perfusion pressure and cardiovascular haemodynamics
- be immediately reversible
- have few, if any, side effects
DRUG DOSAGES FOR RSI
Regarding doses given below:
- doses shown are for intravenous (IV) administration
- IBW = ideal body weight, TBW = total body weight
- doses may need to be adjusted in the hypotensive or shocked patient (see Intubation, Hypotension and Shock)
Induction agents
- Ketamine 1.5-2 mg/kg IBW
- Etomidate 0.3-0.4 mg/kg TBW
- Fentanyl 2-10 mcg/kg TBW
- Midazolam 0.1-0.3 mg/kg TBW
- Propofol 1-2.5 mg/kg IBW + (0.4 x TBW) (others simply use 1.5 mg/kg x TBW as the general guide)
- Thiopental 3-5 mg/kg TBW
Neumuscular blockers:
- Suxamethonium 1-2 mg/kg TBW
- Rocuronium 0.6-1.2 mg/kg IBW
- Vecuronium 0.15-0.25 mg/kg IBW
INDUCTION AGENTS
Ketamine
- Dose: 1.5 mg/kg IV (4mg/kg IM)
- Onset: 60-90 sec
- Duration: 10-20 min
- Use: any RSI, especially if hemodynamically unstable (OK in TBI, does not increase ICP despite traditional dogma) or if reactive airways disease (causes bronchodilation)
- Drawbacks: increased secretions, caution in cardiovascular disease (hypertension, tachycardia), laryngospasm (rare), raised intra-ocular pressure
Thiopentone
- Dose: 3-5 mg/kg IV TBW
- Onset: 30-45 sec
- Duration: 5-10 min
- Use: any RSI if haemodynamically stable, status epilepticus
- Drawbacks: histamine release, myocardial depression, vasodilation, hypotension, must NOT be injected intra-arterially due to risk of distal ischaemia, contra-indicated in porphyria
Propofol
- Propofol 1-2.5 mg/kg IBW + (0.4 x TBW) (others simply use 1.5-2.5 mg/kg x TBW as the general guide)
- Onset: 15-45 seconds
- Duration: 5 – 10 minutes
- Use: Haemodynamically stable patients, reactive airways disease, status epilepticus
- Drawbacks: hypotension, myocardial depression, reduced cerebral perfusion, pain on injection, variable response, very short acting
Fentanyl
- Dose IV 2-10 mcg/kg TBW
- Onset: <60 seconds (maximal at ~5 min)
- Duration: dose dependent (30 minutes for 1-2 mcg/kg, 6h for 100 mcg/kg)
- Use: may be used in a low dose as a sympatholytic premedication (e.g. TBI, SAH, vascular emergencies); may used in a’modified’ RSI approach in low doses or titrated to effect in cardiogenic shock and other hemodynamically unstable conditions
- Drawbacks: respiratory depression, apnea, hypotension, slow onset, nausea and vomiting, muscular rigidity in high induction doses, bradycardia, tissue saturation at high doses
Midazolam
- Dose: 0.3mg/kg IV TBW
- Onset: 60-90 sec
- Duration: 15-30 min
- Use: not usually recommended for RSI, some practitioners use low doses of midazolam and fentanyl for RSI of shocked patients
- Drawbacks: respiratory depression, apnea, hypotension, paradoxical agitation, slow onset, variable response
Etomidate
- 0.3mg/kg IV
- onset: 10-15 seconds
- Use: suitable for most situations including haemodynamically unstable, other than sepsis or seizures
- Drawbacks: adrenal suppression, myoclonus, pain on injection, not available in Australia
PARALYTIC AGENTS
Suxamethonium (aka succinylcholine)
- Dose: 1.5 mg/kg IV (2 mg/kg IV if myasthenia gravis) and 4 mg/kg IM (in extremis)
- Onset: 45-60 seconds
- Duration: 6-10 minutes
- Use: widely used unless conra-indicated; ideal if need to extubate rapidly following an elective procedure or to assess neurology in an intubated pateint
- Drawbacks: numerous contra-indications (hyperkalemia, malignant hyperthermia, >5d after burns/ crush injury/ neuromuscular disorder), bradycardia (esp after repeat doses), hyperkalemia, fasciculations, elevated intra-ocular pressure, will not wear off fast enough to prevent harm in CICV situations
Rocuronium
- Dose: 1.2 mg/kg IV IBW
- Onset: 60 seconds
- Use: can be used for any RSI unless contra-indication or require rapid recovery for extubation after elective procedure or neurological assessment; ensures persistent ideal conditions in CICV situation (i.e. immobile patient for cricothyroidotomy) – can be reversed by sugammadex
- Drawbacks: allergy (Rare)
Vecuronium
- Dose: 0.15 mg/kg IV (may be preceded by a 0.01 mg/kg IV priming dose 3 minutes earlier)
- Osent: 120-180 econds
- Duration: 45-60 minutes
- Use: not recommended for RSI, unless no suxamethonium or rocuronium cannot be used – can be reversed by sugammadex
- Drawbacks: allergy (rare), slow onset, long duration
PRETREATMENT AGENTS
RSI IN DIFFICULT SETTINGS
Ensure 360 degree access to the patient
- consider ‘scoop and run’ (e.g. from prehospital envirnoment to ED, or from ward to recovery/ ICU)
- RSI is rarely practical in the position that the patient is found, whether that be prehospital or on the ward
- airway equipment (e.g. prehospital ‘kit dump’), monitors and the airway assistant are typically on the patient’s right
RSI in an ambulance
- intubation of a patient on the ground:
- best eye line for intubator if intubator is lying prone
- prone intubator is at a mechanical disadvanatge, this can be overcome by perfroming intubatiion with the patient in the left lateral position- but this is more technically challenging and the intubator should have left elbow padding
- ideally avoid intubation on the ground
- can place patient on spine board or equivalent and raise
- can perform with intubator kneeling (use knee pads)
RSI in aircraft
- have a low threshold for RSI prior to take off
- in aircraft there is variable access to the airway and the whole patient so intubation should be avoided if possible
- in confined space aircraft, the approach is to pre-oxyegnate and then land for RSI (PALM may be performed if needed)
- in non-confined space airacraft landing may still be the preferred option
- intubation in an aircraft may be needed in certain settings (e.g. resuce from a hostile environment)
RSI in a ward environment
- consider transfer to recovery/ ICU for RSI
- exercise crowd control
- adjust and move beds and other equipment as required
- ensure access to the patient
- consider the needs of other patients nearby
References and Links
CCC Airway Series
Emergencies: Can’t Intubate, Can’t Intubate, Can’t Oxygenate (CICO), Laryngospasm, Surgical Cricothyroidotomy
Conditions: Airway Obstruction, Airway in C-Spine Injury, Airway mgmt in major trauma, Airway in Maxillofacial Trauma, Airway in Neck Trauma, Angioedema, Coroner’s Clot, Intubation of the GI Bleeder, Intubation in GIH, Intubation, hypotension and shock, Peri-intubation life threats, Stridor, Post-Extubation Stridor, Tracheo-esophageal fistula, Trismus and Restricted Mouth Opening
Pre-Intubation: Airway Assessment, Apnoeic Oxygenation, Pre-oxygenation
Paediatric: Paediatric Airway, Paeds Anaesthetic Equipment, Upper airway obstruction in a child
Airway adjuncts: Intubating LMA, Laryngeal Mask Airway (LMA)
Intubation Aids: Bougie, Stylet, Airway Exchange Catheter
Intubation Pharmacology: Paralytics for intubation of the critically ill, Pre-treatment for RSI
Laryngoscopy: Bimanual laryngoscopy, Direct Laryngoscopy, Suction Assisted Laryngoscopy Airway Decontamination (SALAD), Three Axis Alignment vs Two Curve Theory, Video Laryngoscopy, Video Laryngoscopy vs. Direct
Intubation: Adverse effects of endotracheal intubation, Awake Intubation, Blind Digital Intubation, Cricoid Pressure, Delayed sequence intubation (DSI), Nasal intubation, Pre-hospital RSI, Rapid Sequence Intubation (RSI), RSI and PALM
Post-intubation: ETT Cuff Leak, Hypoxia, Post-intubation Care, Unplanned Extubation
Tracheostomy: Anatomy, Assessment of swallow, Bleeding trache, Complications, Insertion, Insertion timing, Literature summary, Perc. Trache, Perc. vs surgical trache, Respiratory distress in a trache patient, Trache Adv. and Disadv., Trache summary
Misc: Airway literature summaries, Bronchoscopic Anatomy, Cuff Leak Test, Difficult airway algorithms, Phases of Swallowing
Journal articles
- Bernhard M et al. The First Shot Is Often the Best Shot: First-Pass Intubation Success in Emergency Airway Management. Anesth Analg. 2015; 121(5):1389-93. PMID 26484464
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010 May 1;110(5):1318-25. doi: 10.1213/ANE.0b013e3181d5ae47. Epub 2010 Mar 17. PMID: 20237045. [Free Full Text]
- Stept WJ, Safar P. Rapid induction-intubation for prevention of gastric-content aspiration. Anesth Analg. 1970 Jul-Aug;49(4):633-6. PMID: 5534675.
- Stewart JC, Bhananker S, Ramaiah R. Rapid-sequence intubation and cricoid pressure. Int J Crit Illn Inj Sci [serial online] 2014
FOAM and web resources
- Airwaycam.com
- ALIEM — Paucis Verbis card: Rapid Sequence Intubation
- EM Lyceum — Rapid Sequence Intubation, Episode 1 and RSI Episode 2: Induction, “Answers”
- Emergency Medicine News — The Ten Ps of Rapid Sequence Intubation by Darren Braude
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Dr. Nickson
My name is Barbara Thomas, a graduate student at Simmons University. My colleagues, Jessica, Scott, and I are working on a retrospective study considering the use of succinylcholine verses rocuronium , wich is most effective in first pass rsi in flight medicine. We are having a hard time finding new material. Most everything is dated. Any idea of where to look other than Cochran’s, and the flight sites. Thank you, I much appreciate your input.
Barbara Thomas
Fantastic Chaps
Is the midazolam dose correct? Should it be 0.03mg/kg?
Hi Jon,
Yes, these are the correct dosing suggestions. 0.03mg/kg would only be 3mg in me (100kg adult) which will probably be good for some pre-op anxiolysis / anterograde amnesia for me!
In paediatrics (not my speciality, but from what I can find with my drug reference manual):
– Neonatal: Loading dose should not be used. Can use for infusion post induction
– Non-neonatal: 0.05-0.15mg/kg IV
I guess in an RSI, do you really want to use midazolam though? Is the onset of 3-5mins going to be fast enough?
Food for thought!
James
what O2 level is indication for intubation?
Hi A,
Great question. Unfortunately it’s a complex answer (such is medicine).
There may be patients who have totally normal oxygen saturations, but require intubation for airway protection (e.g. airway swelling, markedly reduced GCS or head injuries), for humane reasons (e.g. severe pain from significant burns or trauma etc.), neurological states to facilitate safe procedures / scans / retrievals, and for many other reasons (e.g. preparing for surgery in critically unwell patients etc. etc.)
Honing down on the breathing part of the primary survey, some people may have normal oxygen saturations but their Fraction of Inspired Oxygen (FiO2) or the amount of supplemental oxygen they are receiving may be very high or escalating. Trajectory is really important with these patients, as well as the speed of their trajectory. We saw during COVID a number of patients who had oxygen saturations in the mid-high 80s who were stable, otherwise fit and healthy, and were able to avoid intubation with appropriate positioning and self-prone techniques with supplemental oxygen and non-invasive support…
So unfortunately there is a lot of nuance into what the threshold of “low” oxygen saturations or FiO2 would be (and they are also quite subjective thresholds) to trigger a patient to be intubated. These nuances will also be significantly affected by skill-mix of the clinicians, location (e.g. rural/remote/primary retrieval), country of work, resources etc. etc.
I’m sorry my answer cannot be more clear cut! Perhaps there are others who would like to comment and add in their own or their institution’s thresholds for intubation?
Thanks for commenting and adding to the discussion,
James
You may be interested in this post written during the COVID pandemic discussing “silent hypoxaemia” and deciding when to intubate: https://litfl.com/silent-hypoxaemia-and-covid-19-intubation/
The decision is always nuanced and rarely based on “O2 levels” alone, as James has explained.
Chris