Bougie
OVERVIEW
- aka Eschmann tracheal tube introducer
- the name “gum elastic bougie” is erroneous – it is not made of resins, it is not elastic and it is not used for dilatation
- bougie is also the name given to devices used for esophageal or urethral dilatation
USES
Bougie-assisted
- tracheal intubation via direct or video laryngoscopy, especially in difficult airways or during CPR
- tracheal intubation via supraglottic airway device
- surgical airway (cricothyrotomy)
- selective endobronchial intubation
- blind digital intubation
- confirmation of endotracheal tube position
- endotracheal tube exchange (a device with a central lumen allowing oxygenation is better for this)
- intercostal catheter insertion (as a potential rescue technique – see below)
DESCRIPTION
- the original Eschmann tracheal tube introducer is a flexible device that is 60 cm (24 in) in length, 15 French (5 mm diameter) with a small “hockey-stick” angle at the far end (the coude tip — usually at 35-40 degrees)
- some types have external distance markings
- some types have a central lumen and port for ventilation
- Sizes of different types range 10 or 15 F (600–700 mm)
METHOD OF INSERTION AND/OR USE
Bougie-assisted Endotracheal Intubation
- the bougie is typically held by the intubator 20- 30 cm proximal to the coude tip
- the bougie should be inserted via the side of the mouth, rather then down the center, so that rotation of the bougie provides better control of the coude tip in the vertical plane
- it is typically inserted directly into the trachea and then used as a guide over which the endotracheal tube can be railroaded (analogous to the Seldinger technique)
- it can be preloaded with an endotracheal tube or an assistant can pass the endotracheal tube over the free end of bougie while the intubator maintains visualisation of the bougie/ cords and ensures the placement of the bougie remains secure
- the assistant should continuously walk their hands down the bougie as the endotracheal tube is advanced over it
- the tracheal tube should be introduced through the cords, over the bougie, using a 90º anti-clockwise rotation to prevent its beveled point from getting caught in the arytenoids
- the user should feel the tip of the bougie ‘click’ as it passes along the tracheal rings
- when used to confirm endotracheal placement the bougie is passed down the endotracheal tube and there should be ‘hold up’ at 30-40cm depth, if this does not occur the bougie is likely to be in the esophagus.
- the bougie may be passed into one of the main bronchi by twisting the angled tip in the preferred direction, this may be useful to facilitate endobronchial intubation (e.g. in massive hemoptysis where other equipment is unavailable)
- the ‘Kiwi grip’ can be used by a solo operator – the bougie is curled upon itself and preloaded with an endotracheal tube (see here and here), as can the ‘pistol grip’ (when the bougie is held together with the laryngoscope in one hand – see here).
Correct use of a bougie is shown below (video by HQMEDED):
Trouble-shooting the use of a bougie is shown below:
Stylets and bougies by Tim Leeuwenberg:
Bougie-assisted surgical airway
- use scalpel to incise through cricothyroid membrane
- pass bougie through incision alongside the scalpel which is used as a guide into the trachea until hold up at at the carina is achieved
- pass endotracheal tube over bougie into trachea
Bougie-assisted blind digital intubation (from Rich, 2008)
PMC2566913 Bougie-assisted digital intubation.
(a) After the epiglottis is identified by palpating it with the long finger of the left hand, the bougie is threaded through the glottis and advanced into the trachea. Tracheal clicking elicits tactile vibrations, which confirm tracheal placement of the bougie.
(b) The bougie is withdrawn slightly so that the 25-cm mark is at the corner of the lip. The endotracheal tube is threaded over the bougie while the bougie is stabilized in place.
(c) With the bougie held in place, the endotracheal tube is turned a quarter turn to the left and then advanced to an appropriate depth.
(d) The tube is held in place while the bougie is withdrawn. Tracheal intubation is then confirmed using capnography or an esophageal detector device.
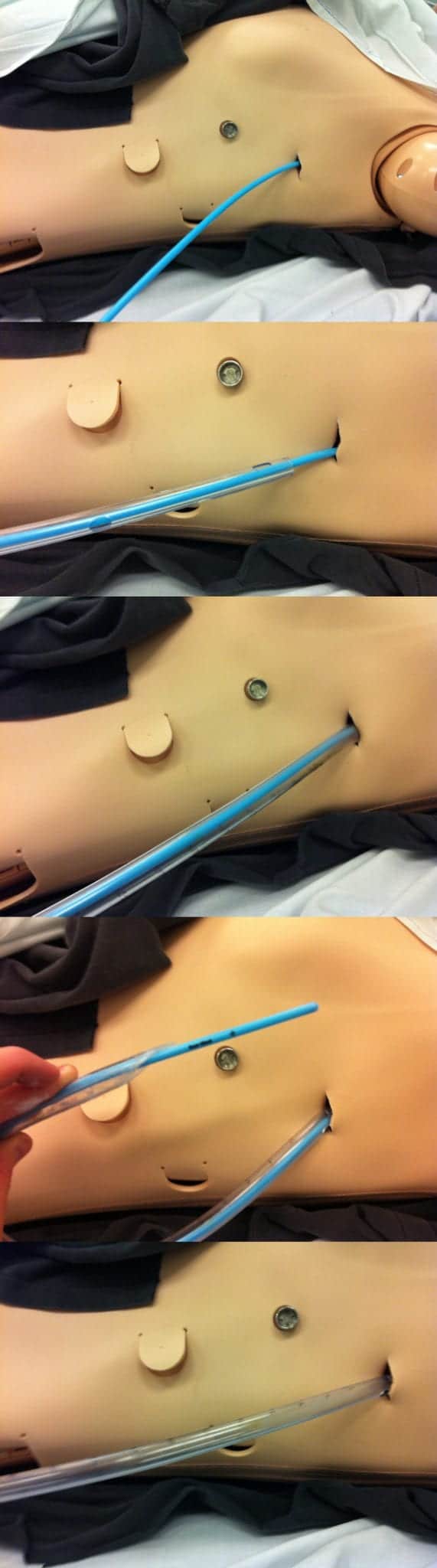
Bougie-assisted intercostal catheter insertion
- bougies can be used as a rescue technique for intercostal catheter insertion when the standard approach is problematic (e.g. in an obese patient where it is easy to lose the tract when inserting the intercostal catheter)
- perform initial steps of intercostal catheter insertion
- insert finger into pleural space, ensuring no adhesions (as per usual technique)
- gently insert bougie tip into pleural space alongside finger
- remove finger, being careful not to advance bougie tip deeper into the pleural cavity
- pass ICC over bougie into pleural space
- remove bougie from within the ICC
- secure ICC, dress and obtain check CXR
- note that this technique has not been validated in terms of efficacy of safety and should be considered a rescue technique only by experienced practitioners
- do not use the bougie as a trocar to puncture the pleura!
COMPLICATIONS
- airway trauma (usually minimal as the bougie is flexible)
- tracheal or bronchial perforation leading to pneumothorax or mediastinal emphysema
- esophageal perforation
- the flexibility of the bougie may make it difficult to control in the hands of novices
- bougie fracture (if reusable or defective)
- transmission of disease (if reusable)
- failure of procedure
OTHER INFORMATION
- bougies come in a range of sizes, shapes and flexibility
- may be disposable (single use) or reusable (multiple use)
- some have a central lumen that facilitates oxygenation (e.g. jet ventilation) and can be used if an airway exchange catheter is unavailable
- A 10 French introducer should be used for endotracheal tube sizes 4.0 to 5.5
- the bougie may be placed in the side of the mouth during preoxygenation with a BVM to assist in rapid insertion
- Light wands can also be used like a bougie – it has a lighted tip and is passed blindly into the airway and neck transillumination produced – a well circumscribed anterior neck glow may indicate translaryngeal placement and a tube passed over the wand into the airway
- the bougie was first described by legendary NZ-born anaesthetist Sir Robert Reynolds Macintosh (from Timaru!)
Demonstration of the pocket bougie, which allows single person bougie-assisted endotracheal intubation:
References and Links
CCC Airway Series
Emergencies: Can’t Intubate, Can’t Intubate, Can’t Oxygenate (CICO), Laryngospasm, Surgical Cricothyroidotomy
Conditions: Airway Obstruction, Airway in C-Spine Injury, Airway mgmt in major trauma, Airway in Maxillofacial Trauma, Airway in Neck Trauma, Angioedema, Coroner’s Clot, Intubation of the GI Bleeder, Intubation in GIH, Intubation, hypotension and shock, Peri-intubation life threats, Stridor, Post-Extubation Stridor, Tracheo-esophageal fistula, Trismus and Restricted Mouth Opening
Pre-Intubation: Airway Assessment, Apnoeic Oxygenation, Pre-oxygenation
Paediatric: Paediatric Airway, Paeds Anaesthetic Equipment, Upper airway obstruction in a child
Airway adjuncts: Intubating LMA, Laryngeal Mask Airway (LMA)
Intubation Aids: Bougie, Stylet, Airway Exchange Catheter
Intubation Pharmacology: Paralytics for intubation of the critically ill, Pre-treatment for RSI
Laryngoscopy: Bimanual laryngoscopy, Direct Laryngoscopy, Suction Assisted Laryngoscopy Airway Decontamination (SALAD), Three Axis Alignment vs Two Curve Theory, Video Laryngoscopy, Video Laryngoscopy vs. Direct
Intubation: Adverse effects of endotracheal intubation, Awake Intubation, Blind Digital Intubation, Cricoid Pressure, Delayed sequence intubation (DSI), Nasal intubation, Pre-hospital RSI, Rapid Sequence Intubation (RSI), RSI and PALM
Post-intubation: ETT Cuff Leak, Hypoxia, Post-intubation Care, Unplanned Extubation
Tracheostomy: Anatomy, Assessment of swallow, Bleeding trache, Complications, Insertion, Insertion timing, Literature summary, Perc. Trache, Perc. vs surgical trache, Respiratory distress in a trache patient, Trache Adv. and Disadv., Trache summary
Misc: Airway literature summaries, Bronchoscopic Anatomy, Cuff Leak Test, Difficult airway algorithms, Phases of Swallowing
LITFL
- Best use for a bougie? (light-hearted look at the myriad uses of a bougie)
- Befriend the bougie!
- Own the Airway!
Journal articles and textbooks
- McCarroll SM, Lamont BJ, Buckland MR, Yates AP. The gum-elastic bougie: old but still useful. Anesthesiology. 1988 Apr;68(4):643-4 PMID: 3354910.
- Reis Lde A, Reis GF, Oliveira MR, Ingarano Lel B. [Bougie]. Rev Bras Anestesiol. 2009 Sep-Oct;59(5):618-23 PMID: 19784519.
- Rich JM. Successful blind digital intubation with a bougie introducer in a patient with an unexpected difficult airway. Proc (Bayl Univ Med Cent). 2008 Oct;21(4):397-9: PMC2566913
FOAM and web resources
- AirwayCam — Bougie and Tube Introducers
- ALIEM — Trick of the Trade: Seldinger chest tube technique using bougie
- Dave on Airways — The bougie – is it immortal? (2014)
- EMCrit Wee – Bougie Prepass and CricCon for Difficult Airway
- EMCrit — A New Bougie for your Pocket by Jim DuCanto
- PHARM — Bougie three ways and Bougie with Kiwi and Pistol grips
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
