Polymorphic VT and Torsades de Pointes (TdP)
Definitions
Polymorphic ventricular tachycardia (PVT) is a form of ventricular tachycardia in which there are multiple ventricular foci with the resultant QRS complex varying in amplitude, axis, and duration. The most common cause of PVT is myocardial ischaemia/infarction.
Torsades de pointes (TdP) is a specific form of PVT occurring in the context of QT prolongation — it has a characteristic morphology in which the QRS complexes “twist” around the isoelectric line.
- For TdP to be diagnosed, the patient must have evidence of both PVT and QT prolongation
- Bidirectional VT is another specific type of of PVT, most commonly associated with digoxin toxicity
- First described by François Dessertenne (1917-2001) in 1966
Clinical Significance
- TdP is often short lived and self terminating, however can be associated with haemodynamic instability and collapse. TdP may also degenerate into ventricular fibrillation (VF)
- QT prolongation may occur secondary to multiple drug effects, electrolyte abnormalities and medical conditions; these may combine to produce TdP, e.g. hypokalaemia may precipitate TdP in a patient with congenital long QT syndrome
- Recognition of TdP and the risk of TdP allows the instigation of specific management strategies (e.g. magnesium, isoprenaline, overdrive pacing, etc.)
Further review of the causes of QT prolongation
Pathophysiology of TdP
- A prolonged QT reflects prolonged myocyte repolarisation due to ion channel malfunction
- This prolonged repolarisation period also gives rise to early after-depolarisations (EADs)
- EADs may manifest on the ECG as tall U waves; if these reach threshold amplitude they may manifest as premature ventricular contractions (PVCs)
- TdP is initiated when a PVC occurs during the preceding T wave, known as ‘R on T’ phenomenon
- The onset of TdP is often preceded by a sequence of short-long-short R-R intervals, so called “pause dependent” TDP, with longer pauses associated with faster runs of TdP
Electrocardiographic Pearls
- During short runs of TdP or single lead recording the characteristic “twisting” morphology may not be apparent
- Bigeminy in a patient with a known long QT syndrome may herald imminent TdP
- TdP with heart rates > 220 beats/min are of longer duration and more likely to degenerate into VF
- Presence of abnormal (“giant”) T-U waves may precede TdP
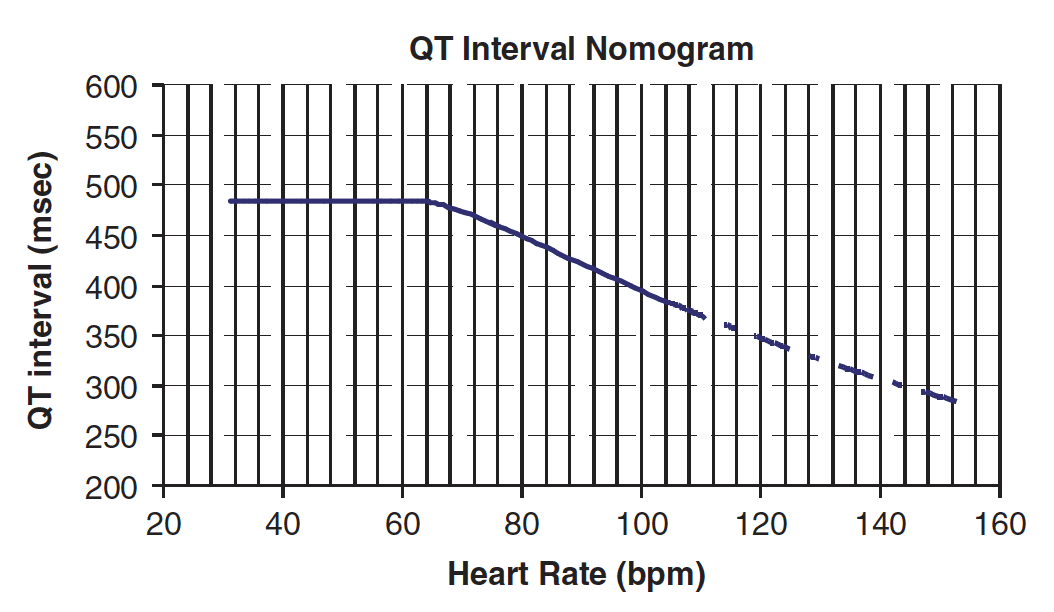
Drug-induced Torsades
- In the context of acute poisoning with QT-prolonging agents, the risk of TdP is better described by the absolute rather than corrected QT
- More precisely, the risk of TdP is determined by considering both the absolute QT interval and the simultaneous heart rate (i.e. on the same ECG tracing)
- These values are then plotted on the QT nomogram (below) to determine whether the patient is at risk of TdP
- A QT interval-heart rate pair that plots above the line indicates that the patient is at significant risk of TdP
ECG Examples
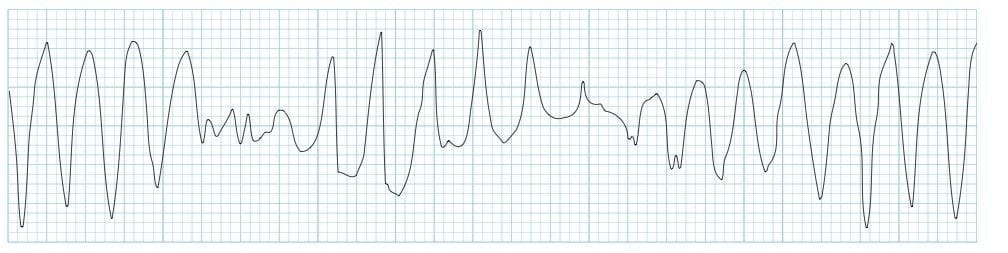
Example 1
Torsades de Pointes:
- Frequent PVCs with ‘R on T’ phenomenon trigger a run of polymorphic VT which subsequently begins degenerates into VF
- QT interval is difficult to see because of artefact but appears slightly prolonged (QTc ~480ms), making this likely to be TdP
- This combination of mildly prolonged QTc and frequent PVCs / bigeminy is commonly seen in acute myocardial ischaemia — these patients are at high risk of deterioration into PVT / VF
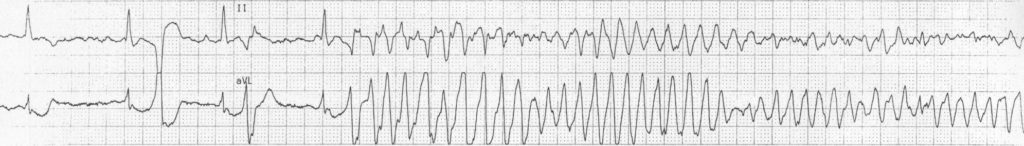
Example 2

TdP secondary to hypokalaemia:
- Sinus rhythm with inverted T waves, prominent U waves and a long Q-U interval due to severe hypokalaemia (K+ 1.7)
- A premature atrial complex (beat #9 of the rhythm strip) lands on the end of the T wave, causing ‘R on T’ phenomenon and initiating a paroxysm of polymorphic VT
- Because of the preceding long QU interval, this can be diagnosed as TdP
Example 3

TdP secondary to hypokalaemia:
- Another ECG from the same patient (K+ still 1.7)
- A brief, self-terminating paroxysm of TdP is again precipitated by a PAC causing ‘R on T’
Example 4
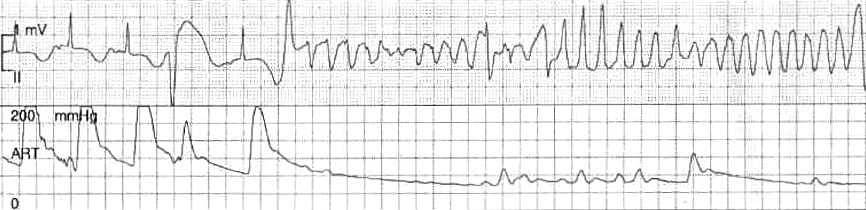
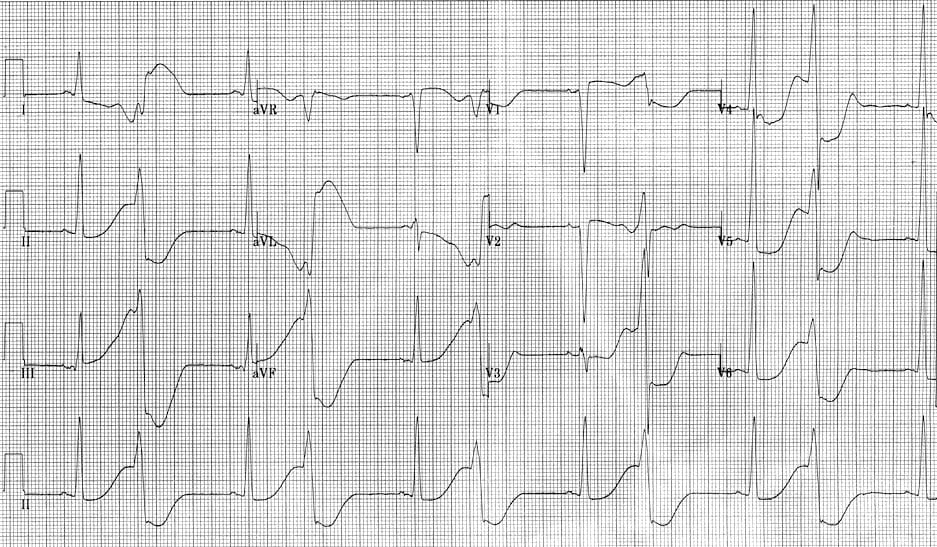
Torsades de Pointes:
- Sinus rhythm, or possibly ectopic atrial rhythm (biphasic / inverted P waves in lead II)
- Prolonged QTc interval of 540 ms (greater than half the R-R interval)
- Ventricular ectopics with ‘R-on-T’ phenomenon — the second PVC initiates a run of TdP
NB. See how the arterial line pressure waveform (lower tracing) is affected by the dysrhythmia. There is a reduced volume pulse during the first PVC as the heart has less time to fill. Subsequently the cardiac output drops away to almost nothing during the run of TdP – this is likely to result in syncope or cardiac arrest.
Example 5
R on T phenomenon:
- There is sinus rhythm with frequent PVCs in a pattern of ventricular bigeminy
- The QT interval is markedly prolonged (at least 600ms), with each PVC falling on the preceding T wave (= ‘R on T’ phenomenon)
- This ECG is extremely high risk for TdP – in fact this patient had a TdP cardiac arrest shortly after this ECG was taken
For the story behind this ECG, check out Cardiovascular Curveball 003.
Torsade(s) de(s) pointe(s)?
The term “torsades de pointes,” while widely adopted, has sparked decades-long debate over its grammatical correctness and original intent in French. François Dessertenne (1917-2001), in his seminal 1966 paper, used “torsades de pointes” six times and “torsade de pointes” once and “les torsades de pointes” thrice— but never “des.” The inconsistency seeded a linguistic tangle still unresolved.
Original Inspiration: Dessertenne likened the ECG pattern to architectural torsades (twisted column motifs) described in the Robert Dictionary, and to the asymmetrical pointed teeth of a comb twisted along its axis — visualising the “twisting” of QRS peaks, the pointes.
Dessertenne held one end of a comb still and rotate the other end along the long axis of the comb. The relative rigidity of the comb stops the rotation before 180°. A 180° rotation would be needed to fully demonstrate how the points of these teeth and the intermediary gap simulated, respectively, the pointed side and the broad side of the asymmetrical electrographic waves that formed the torsades de pointes.
Plural Confusion: Should the phrase be singular (torsade de pointe), plural-singular (torsades de pointes), or fully plural (torsades des pointes)? The eminent French cardiologist Guy Fontaine (1936-2018) posed this question at a dinner party in 1991, in Liège:
- Robert Slama argues for “de pointes” stating an “s” is always needed after “pointe” implying more than one QRS complexes are twisting around the isoelectric line.
- Paul Puech, after consulting the Comité de Défense de la Langue Française supports “de pointe” — focusing on the twisting occurring at the single tip of each QRS.
Finally Mullins (2011) advocated for the fully pluralised “torsades des pointes”, asserting that “each word must be plural,” and noting that Dessertenne originally used les (plural “the”).
In summary – use what you feel best demonstrates the ECG findings, and use it consistently. For my part I am sticking with Dessertenne, his original description and the term he used most often with ‘torsades de pointes‘
Related Topics
- Hypokalaemia
- Hypomagnesaemia
- QT interval
- Drugs causing QT prolongation
- Premature Ventricular Complex
- Ventricular tachycardia (monomorphic VT)
- Ventricular fibrillation
- Cardiovascular Curveball 003
References
- Dessertenne F. La tachycardie ventriculaire à deux foyers opposés variables [Ventricular tachycardia with 2 variable opposing foci]. Archives des Maladies du Cœur et des Vaisseaux 1966; 59(2): 263–272
- Chan A, Isbister GK, Kirkpatrick CM, Dufful SB. Drug-induced QT prolongation and torsades de pointes: evaluation of a QT nomogram. QJM. 2007 Oct;100(10):609-15.
- Kirchhof P, Franz MR, Bardai A, Wilde AM. Giant T-U waves precede torsades de pointes in long QT syndrome: a systematic electrocardiographic analysis in patients with acquired and congenital QT prolongation. J Am Coll Cardiol. 2009 Jul 7;54(2):143-9
- Viskin S. Long QT syndromes and torsades de pointes. Lancet 1999;354:1625-33
- S Viskin, R Fish, D Zeltser, B Belhassen, K Heller, D Brosh, S Laniado, H V Barron. Arrhythmias in the congenital long QT syndrome: how often is torsade de pointes pause dependent? Heart 2000;83:661–666
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


how can we differentiate between pre excited atrial fibrillation and polymorphic vt?