Calcium Channel Blocker Toxicity
Reviewed and revised 17 December 2015
OVERVIEW
- Severe calcium channel blocker toxicity is highly lethal, as a result of cardiovascular collapse
- Good outcomes can be achieved through aggressive treatment and provision of circulatory support
MECHANISM OF TOXICITY
Verapamil and diltiazem are the most lethal calcium-channel blockers in overdose:
- bind the alpha-1 sub-unit of L-type calcium channels, preventing the intracellular influx of calcium
- These channels are functionally important in cardiac myocytes, vascular smooth muscle cells, and islet beta cells
In overdose, receptor selectivity may be lost, so even dihydroperidines (e.g. amlodipine) may cause cardiotoxicity in addition to vasodilation in large overdoses.
Cardiac toxicity results from:
- excessive negative inotropy: myocardial depression
- negative chronotropy: sinus bradycardia
- negative dromotropy: atrioventricular node blockade
Effects on vascular smooth muscle tone result in:
- decreased afterload
- systemic hypotension
- coronary vasodilation
Metabolic effects, including hyperglycaemia, also occur:
- hypoinsulinaemia, as insulin release is dependent on calcium influx into islet beta cells through L-type calcium channels
- calcium channel blocker-induced insulin resistance
- calcium channel blockers also impair the cardiac myocyte adaptive response of shifting from using free fatty acids, their favoured “resting state” energy substrate, to carbohydrates, due to:
- impaired uptake of glucose and free fatty acids by cardiac myocytes
- inhibition of calcium-dependent mitochondrial activity required for glucose catabolism
CLINICAL FEATURES
Onset
- The onset of symptoms with standard preparations of calcium channel blockers is typically within 1-2 hours of ingestion
- slow release preparations the onset of significant toxicity may be delayed 12-16 hours with peak effects after 24 hours
Cardiovascular manifestations
- The early signs of toxicity are usually bradycardia, first degree heart block and hypotension
- This may progress to refractory shock and death without appropriate intervention
- Complications may include myocardial ischemia, stroke and non-occlusive mesenteric ischemia
Metabolic manifestations
- hyperglycaemia (severity often correlates with the severity of calcium channel toxicity)
Neurological:
- Seizures and coma are rare and usually signify the presence of a coingestant. However, they can occur as a late feature of toxicity due to cardiovascular collapse, as can focal deficits.
Other:
- pulmonary oedema
- renal failure
- nausea and vomiting
INVESTIGATIONS
Bedside
- ECG: bradycardia, accelerated AV node conduction, 2nd and 3rd degree heart block, sinus arrest with nodal escape, asystole
- hyperglycaemia is a marker of severity
- blood gas: hyperlactaemia, metabolic acidosis, impaired oxygen delivery
Laboratory
- evidence of organ dysfunction due to shock (e.g. increased creatinine)
Imaging
- CXR: pulmonary edema
- Echocardiography: evidence of impaired contractility
Other
- invasive haemodynamic monitoring may help determine the relative contributions of negative inotropy and systemic vasodilation as the cause of circulatory failure and help guide therapies
MANAGEMENT
Resuscitation – address life-threats
- early intubation and ventilation when life-threatening toxicity is anticipated
- Early invasive blood pressure monitoring if evolving hypotension and shock; initiate therapies below
Specific treatment (support cardiovascular system)
- Fluid resuscitation (up to 20 mL/kg crystalloid)
- Calcium
- can be a useful temporising measure to increase HR and BP
- options
- 10% calcium gluconate 60mL IV (0.6-1.0 mL/kg in children)
- 10% calcium chloride 20mL IV (0.2 mL/kg in children) [must be given via CENTRAL VENOUS ACCESS – it burns!]
- repeat boluses can be given up to 3 times
- consider calcium infusion to keep serum calcium >2.0 mEq/L
- Atropine: 0.6mg every 2 min up to 1.8 mg (often ineffective)
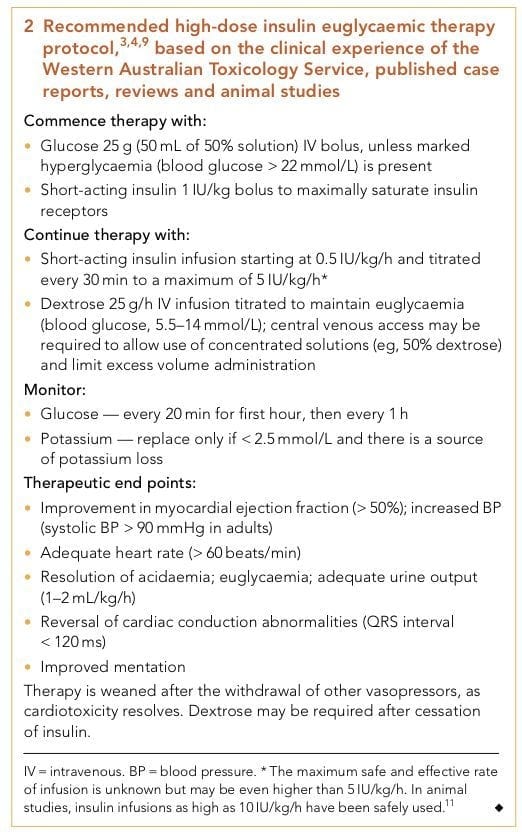
- High dose insulin – euglycaemic therapy (HIET)
- see below
- Vasoactive infusions
- titrate catecholamines to effect (inotropy and chronotropy); options include dopamine, adrenaline and/ or noradrenaline
- if vasoplegic, consider noradrenaline and vasopressin. Consider methylene blue if refractory (to decrease cGMP formation, scavenge nitric oxide, and inhibit nitric oxide synthesis leading to vasoconstriction).
- Sodium bicarbonate
- consider in severe metabolic acidosis
- 50-100 mEq sodium bicarbonate (0.5-1.0 mEq/kg in children)
- Cardiac pacing
- electrical capture may be difficult to achieve and may not improve overall perfusion
- use ventricular pacing to bypass AV blockade, typical with rates not in excess of 60/min
- Intralipid
- consider in refractory cases, as calcium channel blockers lipid soluble agents
- Circulatory support devices
- consider in refractory cases
- VA ECMO or cardiac bypass is preferred to intra-aortic balloon counterpulsation (useful if poor inotropy, will not correct refractory vasoplegia)
High-dose insulin euglycaemic therapy (HIET)
- The place of HIET in the step-wise approach to managing cardiovascular toxicity has evolved
- Formerly considered a last ditch measure, early is use is increasingly advocated. This is important as the beneficial effects of HIET are not immediate
Decontamination
- In the asymptomatic patient who presents early, activated charcoal can be given:
- within 1 h of ingestion for standard release preparations
- within 4 hours of ingestion for SR preparations
- Whole bowel irrigation can also be performed following the administration of activated charcoal if the patient meets these criteria:
- cooperative
- presents within 4 hours of ingestion of >10 tablets of verapamil or diltiazem SR
- no evidence of established toxicity
- However, WBI is not without risks and some experts advise against it’s use.
Enhanced elimination
- nil
Antidotes
- see above (calcium, high-dose insulin euglycaemic therapy)
Disposition
- Any patient manifesting calcium channel toxicity needs HDU/ ICU level care
- Asymptomatic patients with normal vital signs require cardiac monitoring for:
- 4 hours if standard release verapamil or diltiazem
- 16 hours if SR verapamil or diltiazem
- psychiatric assessment if appropriate
FURTHER INFORMATION
- the exact timing of when high dose insulin euglycaemic therapy should be given in the stepwise approach is uncertain
- echocardiography and invasive monitoring are helpful to assess the cardiovascular manifestations of calcium channel toxicity; vasopressors are more likely to be useful if vasodilation is significant whereas insulin and inotropes are more likely to be beneficial when there is impaired contractility
- glucagon has no role in the treatment of calcium channel blocker toxicity
References and Links
CCC Toxicology Series
General
Approach to acute poisoning, ECGs in Tox, Evidenced-based Tox, Toxicology literature summaries, Does anti-venom work?
Toxins / Overdose
Amphetamines, Barbituates, Benzylpiperazine, Beta Blockers, Calcium Channel Blocker, Carbamazepine, Carbon Monoxide, Ciguatera, Citrate, Clenbuterol, Cocaine, Corrosive ingestion, Cyanide, Digoxin, Ethanol, Ethylene Glycol, Iron, Isoniazid, Lithium, Local anaesthetic, Methanol, Monoamine oxidase inhibitor (MAOI), Mushrooms (non-hallucinogenic), Opioids, Organophosphate, Paracetamol, Paraquat, Plants, Polonium, Salicylate, Scombroid, Sodium channel blockers, Sodium valproate, Theophylline, Toxic alcohols, Tricyclic antidepressants (TCA)
Envenomation
Marine, Snakebite, Spider, Tick paralysis
Syndromes
Alcohol withdrawal, Anticholinergic syndrome, Cholinergic syndrome, Drug withdrawals in ICU, Hyperthermia associated toxidromes, Malignant hyperthermia (MH), Neuroleptic malignant syndrome (NMS), Opioid withdrawal, Propofol Infusion Syndrome (PrIS) Sedative toxidrome, Serotonin syndrome, Sympatholytic toxidrome, Sympathomimetic toxidrome
Decontamination
Activated Charcoal, Gastric lavage, GI Decontamination
Enhanced Elimination
Enhanced elimination, Hyperbaric therapy for CO
Antidotes
Antidote summary, Digibind, Glucagon, Flumazenil, HIET – High dose euglycaemic therapy, Intralipid, Methylene Blue, N-Acetylcysteine (NAC), Naloxone
Miscellaneous
Cocaine chest pain, Digoxin and stone heart theory, Hyperbaric oxygen, Hypoxaemia in tox, Liver failure in tox, Liver transplant for paracetamol, Methaemoglobinaemia, Urine drug screen
LITFL
- ECG Library — Beta blocker and calcium channel toxicity
- Toxicology Conundrum 028 — Verapamil overdose
Journal articles
- Bailey B (2003). Glucagon in beta-blocker and calcium channel blocker overdoses: a systematic review. Journal of toxicology. Clinical toxicology, 2003; 41 (5): 595-602 PMID: 14514004
- Greene SL, Gawarammana I, Wood DM, Jones AL, & Dargan PI Relative safety of hyperinsulinaemia/euglycaemia therapy in the management of calcium channel blocker overdose: a prospective observational study. Intensive care medicine, 2007; 33 (11): 2019-24 PMID: 17622512
- Kerns W 2nd Management of beta-adrenergic blocker and calcium channel antagonist toxicity. Emergency medicine clinics of North America, 25 (2) PMID: 17482022
- Levine M, Curry SC, Padilla-Jones A, Ruha AM. Critical care management of verapamil and diltiazem overdose with a focus on vasopressors: a 25-year experience at a single center. Annals of emergency medicine. 2007; 62(3):252-8. 2013. [pubmed]
- Nickson CP, & Little M (2009). Early use of high-dose insulin euglycaemic therapy for verapamil toxicity. The Medical journal of Australia, 191 (6), 350-2 PMID: 19769561 (abstract and pdf link)
- St-Onge M, Dubé PA, Gosselin S, et al. Treatment for calcium channel blocker poisoning: a systematic review. Clinical toxicology (Philadelphia, Pa.). 52(9):926-44. 2014. [pubmed] [free full text]
FOAM and web resources
- EMCrit — EMCrit Podcast 27 – Calcium Channel Blocker Overdose (2010)
- TPR — Is lipid emulsion therapy effective in calcium-channel-blocker and beta-blocker overdose? (2015)
- TPR — There is no real evidence on treating calcium channel blocker overdose (2014)
- TPR — Are vasopressors effective therapy in calcium channel blocker overdose? (2013)
- TPR — Pressors or high-dose insulin for calcium channel blocker overdose? (2013)
- TPR — Is methylene blue beneficial in treating calcium-channel-blocker overdose (2011)
- TPR — Calcium channel blocker toxicity, acidosis, and GI decontamination (2010)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
