Eponymous foot injuries
Eponymythology: The myths behind the history
Eponymythology of the foot. Associated signs, symptoms, investigation and management of foot injuries. We review related eponyms; the history of their origin; their relevance today; and modern terminology
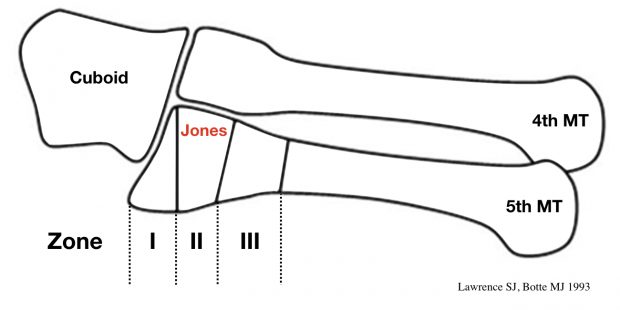
Jones Fracture (1902)

Fracture of the proximal diaphysis of the 5th metatarsal, distal to the tuberosity, without joint involvement caused by foot inversion / twisting and repetitive stress. First described by Robert Jones in 1902 after Jones sustained the injury whilst dancing. He published his case report and that of five similar injuries specifically noting that the fracture is caused by ‘indirect violence’
Whilst dancing, I trod on the outer side of my foot, my heel at the moment being off the ground. Something gave way midway down my foot, and I at once suspected a rupture of the peroneus longus tendon…I hobbled down-stairs to my colleague…to X-ray my foot. This was done, and the fifth metatarsal was found fractured about three-fourths of an inch from its base.
Jones R. 1902: 697
- Sir Robert Jones (1857-1933) was a Welsh General and Orthopaedic Surgeon and part time Roentgenologist.
- Jones R. Fracture of the Base of the Fifth Metatarsal Bone by Indirect Violence. Ann Surg. 1902;35(6):697–700
Jones fracture and current classification

Köhler disease I (1908)

Köhler disease is a rare, self-limiting, avascular necrosis (osteonecrosis) of the navicular bone in children. First described by German radiologist Alban Köhler in 1908 in his MWW article Uber eine häufige, bisher anscheinend unbekannte Erkrankung einzelner kindlicher Knochen [About a common, so far apparently unknown disease of individual children’s bones]
Note: Adult onset osteonecrosis of the tarsal navicular is known as Müller-Weiss syndrome (MWS) or Brailsford disease.
- Alban Köhler (1874 – 1947) was a German Radiologist
- Köhler A. Uber eine häufige, bisher anscheinend unbekannte Erkrankung einzelner kindlicher Knochen. Munchener medizinische Wochenschrift, 1908; 55: 1923-5
- Walther Müller (1888 – 1949); Konrad Weiss (1891 – 1976); and James F Brailsford (1888 – 1961)
- Müller W. Über eine eigenartige doppelseitige Veränderung des Os naviculare pedis beim Erwachsenen. Deutsche Zeitschrift für Chirurgie, Leipzig, 1927; 201: 84-87.
- Weiss K. Über die “Malazie” des Os naviculare pedis. RöFo: Fortschritte auf dem Gebiete der Röntgenstrahlen, 1929; 40: 63-67.
- Brailsford JF. Osteochondritis of the adult tarsal navicular. J Bone Joint Surg Am 1939; 21: 111-120
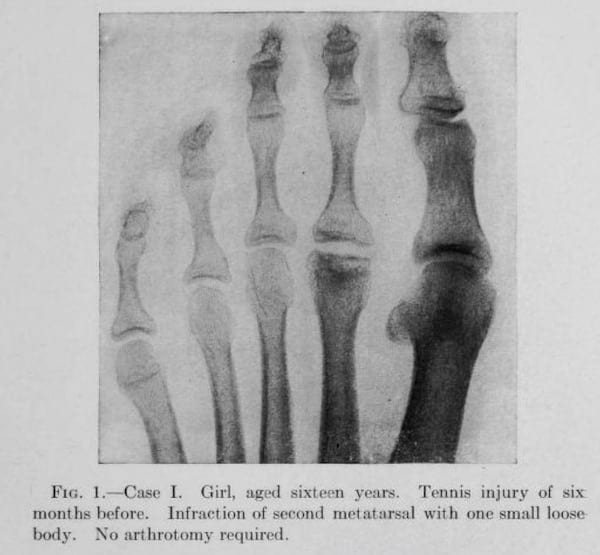
Freiberg infraction (1914)

Osteochondrosis of the metatarsal heads (typically the 2nd metatarsal head) characterized pathologically by subchondral bone collapse, osteonecrosis, and cartilaginous fissures. Freiberg infraction is more common in women and most commonly manifests during adolescence (aged 10-18 years). Bilateral presentation in 10% of cases. Cause unknown and probably multi-factorial. High-heeled shoes have been implicated as a causative factor.
In 1913, Freiberg presented a paper to the Southern Surgical and Gynecological Association. He reported the cases of six young women presenting with a painful limp and discomfort localized to the second metatarsal, the first patient presenting in 1903. Freiberg employed used the term ‘infraction’ as the diagnosis (archaic term for fracture without displacement implying trauma as the cause).
I felt justified in the diagnosis of infraction of the distal end of the second metatarsal, a condition which I have thus far failed to find described in the literature.
Freiberg 1914
Köhler called out Freiberg for an ‘incomplete‘ description of ‘metatarsal infraction‘ lacking mention of the widening of the joint line; thickening of the shaft of the metatarsal and obliteration of the neck. Process often referred to as Köhler disease II
- Albert Henry Freiberg (1868 – 1940) was an American Orthopedic Surgeon.
- Freiberg AH. Infraction of the second metatarsal – a typical injury. Transactions of the Southern Surgical and Gynecological Association 1914; 26: 171-174.
Freiberg original description
Calcaneal angles
Böhler angle (1931)

The angle between line from highest point of anterior process to highest point of posterior facet plus line tangential to superior edge of tuberosity; measured on lateral foot x-ray. Normally 20-40°. If < 20° represents a calcaneal fracture (or more specifically a collapse of the posterior facet)
Normally there exists, between the upper contour of the tuberosity of the os calcis and the line uniting the highest point of the anterior process with the highest point of the posterior articular surface, an angle of thirty to thirty-five degrees. This angle I have named face is driven downward; the the “tuber-joint angle“. In fractures of the os calcis this angle becomes smaller, straight, or even reversed
Böhler 1931
- Lorenz Böhler (1885 – 1973) was an Austrian Physician and Surgeon.
- Böhler L. Diagnosis, pathology and treatment of fractures of the os calcis. J Bone Joint Surg 1931; 13: 75-89
Gissane angle (1946)

Gissane Angle [aka *critical angle; critical angle of Gissane], like the Böhler angle, can be used to help determine the presence of a calcaneus fracture on a radiograph.
The angle is measured on lateral foot radiograph formed by the intersection of the lines drawn along the downward (posterior facet) and the upward (anterior process) slopes of the calcaneal superior surface. Normal range (120-145°).
- William Gissane (1898 – 1981) was an Australian born, British surgeon.
- Gissane W. Discussion on “Fractures of the os calcis” (Proceedings of the British Orthopaedic Association, 1946). J Bone Joint Surg Am 1947; 29: 254–255
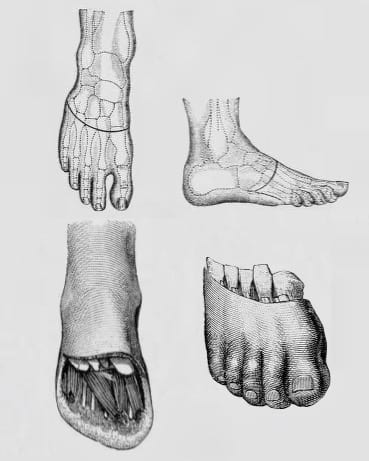
Joints, lines and amputations
Chopart joint (1792)

The mid-tarsal joint is also known as the Chopart joint. Chopart disarticulated this joint when performing forefoot amputations (Chopart amputation). A Chopart fracture-dislocation involves a midtarsal joint (talonavicular and calcaneocuboid) dislocation with associated fractures.
Chopart’s student, Lafiteau provided the first description of Chopart’s method of partial amputation of the foot and Chopart’s joint in Volume IV of Fourcroy ‘La médecine éclairée par les sciences physiques‘ in 1792. The fracture-dislocation was attributed at a later date.
- François Chopart (1743 – 1795) was a French Surgeon.
- Lafiteau. ‘Observation sur une amputation partielle du pied.’ In: Antoine François Fourcroy. La médecine éclairée par les sciences physiques, ou Journal des découvertes relatives aux différentes parties de l’art de guéri. Paris, chez Buisoon, 1792 [Volume IV: 85-86; 87-88].
Chopart amputation Garrè, 1922
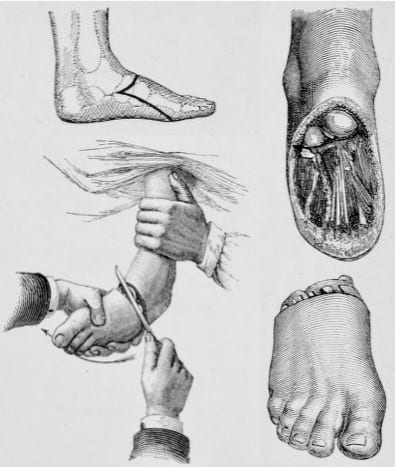
Lisfranc joint (1815)

Lisfranc is eponymously associated with his tarsometatarsal forefoot amputation (Lisfranc amputation). However, Lisfranc was not the first to describe the procedure, with William Hey (1736-1819) first performing the procedure in 1799 and publishing in 1803.
In 1815, Lisfranc described and refined the disarticulation of the forefoot at the tarsometatarsal joint complex which joins the forefoot and midfoot (Lisfranc joint). Lisfranc defined the coup de maître of his disarticulation being the incision of the interosseous ligament (subsequently referred to as the Lisfranc ligament).
The Lisfranc ligament complex includes the dorsal, interosseous, and plantar ligaments which connect C1 (medial cuneiform) to M2 (2nd metatarsal base). Lisfranc injury refers to disruption of the tarsometatarsal joint. Injuries range from sprain (minor diastasis) through to tarsometatarsal fracture-dislocation.
- Jacques Lisfranc de St. Martin (1787 – 1847) was a French Surgeon.
- Hey W. Excision of the metatarsal bones. In: Practical observations in surgery. 1803: 530-537
- Lisfranc J. Nouvelle méthode opératoire pour l’amputation partielle du pied de son articulation tarsométatarsienne. methode precedee des nombreuses modifications qu’a subies celle de Chopart. 1815
Lisfranc’s description of amputation through the tarsal-metatarsal joints requires several pages to describe it, but it took only 1 minute for him to perform it — not too short a time for the unanesthetized patient
Cassebaum WH, 1963
Lisfranc amputation Garrè, 1922
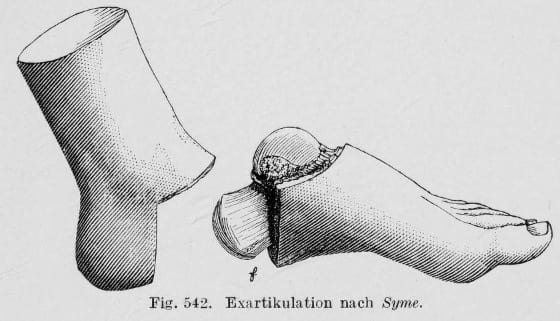
Syme amputation (1831)
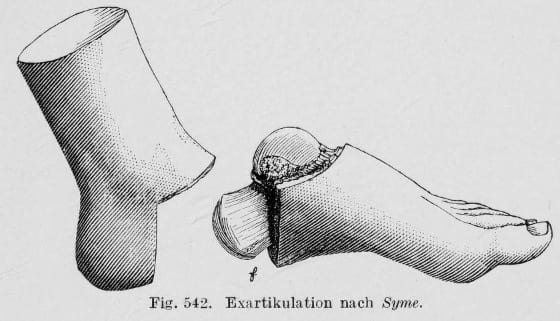
Syme’s amputation involves a disarticulation of the ankle at the tibiotalar joint. The heel pad is conserved and used to cover the distal end of the Tibia. The purported benefit is to allow weight bearing through the limb without the need for a prosthesis. In modern-day it is used chiefly in paediatric patients as the complication and re-amputation rates are lower than in adult populations.
- James Syme (1799–1870) was a Scottish General Surgeon
- Syme J. Treatise on the excision of diseased joints. 1831
Syme amputation (1831)
Considering the great importance of preserving the heel, in respect both of utility and appearance, – to say nothing of the patient’s feelings, who would of course much rather part with the half of his foot than the half of his leg, it seems extraordinary that this operation should not hitherto have been introduced into the practice of British surgery.
James Syme, 1831
Pirogov amputation (1854)
Amputation of the ankle joint in which the posterior process of the calcaneus is retained in the skin flap and opposes the distal cut of the tibia.

- Nikolai Ivanovich Pirogov (Никола́й Ива́нович Пирого́в) (1810 – 1881)
- Pirogov NI. Osteoplastische Verlängerung der Unterschenkelknochen bei der Exarticulation des Fusses. Leipzig, 1854.
More…
Morton metarsalgia (1876)
In 1876 Morton described a series of 15 patients of his own and one of a colleague who all shared the same complaints, which he termed metatarsalgia and which he attributed to an injury to the fourth metatarsophalangeal joint.
- Morton neuroma – benign, perineural fibrotic lesion of a common digital nerve
- Morton neuralgia, metatarsalgia (1876)
Note: In 1835, Filippo Civinini of Pistoja (1805-1844) described in the anatomic letter entitled “Su un nervoso gangliare rigonfiamento alla pianta del piede” (“On the neural ganglion swelling of the foot sole“) – the fusiform (gangliare) swelling (rigonfiamento) in the common plantar digital nerve to the third interspace. However there was no clinical description (metarsalgia) involved in this report.
In 2005 Larson wrote:
Review of the historical writings demonstrates that Morton did not describe a painful condition related to a common plantar digital nerve of any web space but rather a painful condition related to the fourth metatarsophalangeal joint. He treated this painful condition by resection of the joint and the nerves, probably on both sides of that joint.
Larson 2005
- Thomas George Morton (1835 – 1903) was an American surgeon.
- Morton TG. A peculiar and painful affection of the fourth metatarso-phalangeal articulation. American Journal of the Medical Sciences. 1876; 71: 37–45.
References
- Alrasheedi A. Foot Injuries in the Emergency Department. emDOCs
[cite]
Eponym
the person behind the name
Resident medical officer in emergency medicine MB ChB (Uni. Dundee) MRCS Ed. Avid traveller, yoga teacher, polylinguist with a passion for discovering cultures.