Acute Severe Asthma
OVERVIEW
- increased prevalence worldwide
- significant morbidity and mortality -> related to underestimation of severity
- improved outpatient management + more inhaled corticosteroids have meant less serious presentations
- aetiology: ?’hygiene hypothesis’, IgE dependent inflammatory response:
Characteristics:
- reversible obstruction
- inflammation
- mucous formation
Resulting in:
- increased WOB – increased airway resistance and decreased pulmonary compliance -> hypercapnic respiratory failure
- V/Q mismatch – from airway narrowing and closure -> impaired gas exchange and increase WOB to compensate
- adverse cardiorespiratory interactions – increase venous return because of high intrapleural pressures, but also increased afterload -> pulsus paradoxus
HISTORY
- SOB
- cough
- wheeze
- chest tightness
- status asthmaticus = anyone failing to respond to nebulised bronchodilators
- acute severe asthma (90%) – chronic presentation with previous poor control
- hyperacute, fulminating asthma (10%) – onset over<3h
- previous intubations
- previous control
- multiple admissions
- poor psychological circumstances
- poor response to treatments
Triggers
- specific: URTI, housemite, pollen, animal, aspirin, beta-blockers
- non-specific: cold air, exercise, atmospheric pollutants, stress, emotion
EXAMINATION
- RR
- SpO2
- suprasternal retraction
- upright posture
- sweating
Markers of severe episode
- accessory muscle use
- pulsus paradoxus > 25mmHg
- HR >110
- RR > 25-30
- phrases and words
- PEFR < 50%, < 100L/min
- SpO2 < 92%
Markers of imminent respiratory arrest
- altered mental status
- paradoxical respiration
- bradycardia
- quiet chest
- absence of pulsus paradoxus
INVESTIGATIONS
- ABG: initially respiratory alkalosis -> with tiring CO2 rises -> metabolic lactic acidosis from salbutamol/adrenaline (beta adrenergic stimulation -> increases glycolysis and increased pyruvate+lactate production)
- – CXR: perform in severe asthma, LRTI or barotrauma expected
- – monitor K+
- – Mg2+
DIFFERENTIALS TO CONSIDER
- LVF
- anaphylaxis
- aspiration
- upper airway obstruction (vocal cord dysfunction, tracheal stenosis)
- inhaled foreign body
- PE
- hyperventilation syndrome
- pneumothorax
- parodoxical motion of the vocal cords
MANAGEMENT
Established Treatments
- O2 – titrated to SpO2 92%
- Beta-agonists – salbutamol nebulised/MDI/IV – bolus 250mcg (5-10mcg/kg) -> 1-20mcg/min
- Anticholinergics – ipratropium bromide 500mcg Q2-6 hourly nebulized
- Corticosteroids – hydrocortisone 200mg Q6hrly -> prednisone 0.5mg/kg/day
- Aminophylline – 6mg/kg load -> 0.5mg/kg/hr (check levels daily, aim 30-80micromol/L)
Non-established Treatments
- Adrenaline – nebulised 5mg, SC 0.5mg, IV – load with 1mg -> 1-20mcg/min
- MgSO4 – 5-10mmol over 20min (up to 80mmol have been given)
- Heliox – reduces turbulent air flow, 70:30 (He:O2)
- Ketamine – 0.5-2mg/kg/hr
- Inhalational agents – sevoflurane, anaesthetic machine or custom fitted ventilator required
- Leukotriene anatagonists – some benefit in chronic asthma
- BAL – can clear mucous plugging but transiently worsens bronchospasm
RAPID SEQUENCE INTUBATION
- induction agent:
— ketamine preferred due to bronchodilation
— propofol is an alternative, but beware hypotension - consider a ‘delayed sequence intubation’ approach using ketamine and non-invasive ventilation for pre-oxygenation if experienced
- avoid drugs that cause histamine release and may worsen
- intubated asthma patients are prone to post-intubation hypotension due to dynamic hyperinflation (‘stacking’), hypovolaemia, induction drugs and tension pneumothorax (SH!T)
- initially provide gentle BVM post-intubation then transition to mechanical ventilation with appropriate settings (see below) when stable
VENTILATION
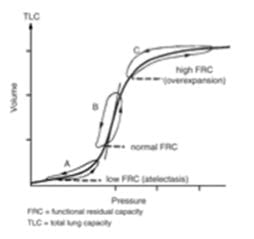
Dynamic Hyperinflation
- slow expiratory airflow -> incomplete exhalation of gas during normal expiratory times -> gas trapping
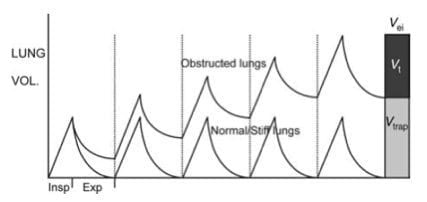
Dynamic Hyperinflation on controlled MV
- the gas trapping = dynamic hyperinflation
- this continues until an equilibrium point is reached where the exhaled volume matches inspired volume to:
(1) increases small-airway calibre (2) increases lung elastic recoil pressure
-> improvement in expiratory airflow -> allows inspired tidal volume to be exhaled in the available expiratory time available
Assessing DHI in the Mechanically Ventilated
- plateau airway pressure (Pplat) = airway pressure after transient expiratory occlusion at the end of inspiration
- inspiratory hold function on ventilator
- this pressure is directly proportional to degree of DHI
- should be maintained at < 25cmH2O
Other techniques:
- end-inspiratory lung volume – not routinely used but is good predictor of complications during MV
- assessment of change in BP and CVP during ventilator disconnection – disconnect for 1-2 min or decrease rate to 4/min
-> increase in MAP and CVP if DHI present
Auto-PEEP or PEEPi
- the gas trapped at the end of expiration exerts a positive pressure on the alveoli (intrinsic positive end-expiratory pressure – PEEPi or auto-PEEP)
- during expiration sequential closure of the most severely obstructed airway occurs with only the less obstructed airway remaining in communication with the airway
-> measured PEEPi underestimates the true magnitude of PEEPi.
-> the only way to infer whether the patient has occult Auto PEEP is the presence of a elevated Pplat and low Auto PEEP
-> there must be occult Auto PEEP that is not accounted for when measuring the end-expiratory pressure from gas trapping.
Assessing PEEPi in the Mechanically Ventilated
- = this is the airway pressure during occlusion of expiratory flow at the end of expiration
- end-expiratory hold function on ventilator
- this measurement is known to underestimated PEEPi as a consequence of small airway closure during expiration (occult PEEPi) -> thus this measurement can only be used to show the presence of DHI but not to regulate mechanical ventilation.)
- ideally should be < 12cmH2O but exact safe level unknown.
Non-invasive Ventilation
Advantages
- helps overcome PEEPi from gas trapping -> reduces inspiratory WOB
- augmentation of inspiration -> decreases WOB, increases TV and minute ventilation
- can decrease expiratory work by opposing dynamic airway compression and allowing more expiration with less gas trapping and hyperinflation
- reduce V/Q mismatch
- decreased hospitalisation rate
- significant increase in FEV1
- significant decrease in hospital admission rates
- titrate to patient comfort and decrease in WOB
Disadvantages
- claustrophobia
- agitation
- gastric distension
- dyssynchrony
- increased expiratory work and hyperinflation
Management
- test patients response by starting with CPAP of 5cmH2O and then titrate IPAP and EPAP to patients comfort.
- there is no role for NIV in patients with respiratory or cardiac arrest or those who are uncooperative or can’t protect their airway
Invasive Ventilation
- life saving but associated with major mortality and morbidity
Indications
- arrest
- severe hypoxia
- altered mental state
- failure to respond to treatment
Procedure
- load with IVF and have inotropes ready to go
- large ETT
- RSI with ketamine/propofol
- slow hand ventilation
- attention to possible complications
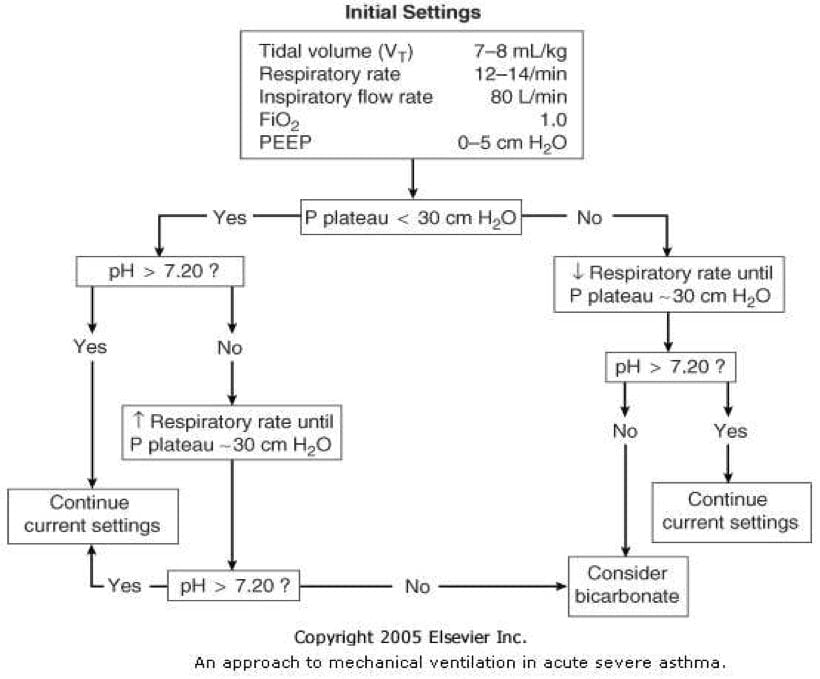
Ventilator settings
- goals: avoid DHI and hypoventilation
- MV 100mL/kg/min (<8L/min in adult)
- TV 6mL/kg
- RR 10
- short inspiratory time (flow rate 80-100L/min) -> high peak airway pressure but low plateau pressure -> decreased barotrauma
- I:E of 1:>4
- hypercapnia will result -> sedation and often paralysis initially
- PEEP
– traditionally no PEEP was used out of fear of exacerbating Auto PEEP
-> but it is now known that PEEP should be set at 60-80% of Auto-PEEP to augment distal airway emptying through splinting airways open
Adjustment of Ventilation
- adjust ventilation to degree of DHI (not PaCO2 or pH)
- if Pplat > 25cmH2O or cardiovascular suppression -> reduce rate
- if Pplat < 25cmH2O -> ventilation can be liberalised with increase in RR and reduction in sedation
- hypercapnia is well tolerated but can consider bicarbonate if pH < 7.1
COMPLICATIONS
HYPOTENSION -> PEA ARREST
- causes:
(1) sedation (2) DHI (3) pneumothorax with tension (4) arrhythmias (5) hypovolaemia (rare) (6) endobronchial intubation (7) myocardial depression from prolonged hypoxia (8) reversal of pleural pressures impairing venous return
-> disconnect from ventilator -> slow RR and load with fluid -> auscultate the chest -> check ETCO2 and ECG -> urgent CXR -> treat cause -> fluids + inotropes -> heliox -> ECMO
PNEUMOTHORAX
-> decrease ventilation to protect other lung -> if hypotensive -> decompress -> if not hypotensive -> urgent CXR as signs not reliable
ACUTE NECROTISING MYOPATHY
- caused by prolonged, deep sedation, steroids +/- paralysis
- results in prolonged weakness and rehabilitation
-> try to avoid!
References and Links
CCC Ventilation Series
Modes: Adaptive Support Ventilation (ASV), Airway Pressure Release Ventilation (APRV), High Frequency Oscillation Ventilation (HFOV), High Frequency Ventilation (HFV), Modes of ventilation, Non-Invasive Ventilation (NIV), Spontaneous breathing and mechanical ventilation
Conditions: Acute Respiratory Distress Syndrome (ARDS), ARDS Definitions, ARDS Literature Summaries, Asthma, Bronchopleural Fistula, Burns, Oxygenation and Ventilation, COPD, Haemoptysis, Improving Oxygenation in ARDS, NIV and Asthma, NIV and the Critically Ill, Ventilator Induced Lung Injury (VILI), Volutrauma
Strategies: ARDSnet Ventilation, Open lung approach, Oxygen Saturation Targets, Protective Lung Ventilation, Recruitment manoeuvres in ARDS, Sedation pauses, Selective Lung Ventilation
Adjuncts: Adjunctive Respiratory Therapies, ECMO Overview, Heliox, Neuromuscular blockade in ARDS, Prone positioning and Mechanical Ventilation
Situations: Cuff leak, Difficulty weaning, High Airway Pressures, Post-Intubation Care, Post-intubation hypoxia
Troubleshooting: Autotriggering of the ventilator, High airway and alveolar pressures / pressure alarm, Ventilator Dyssynchrony
Investigation / Indices: A-a gradient, Capnography and waveforms, Electrical Impedance Tomography, Indices that predict difficult weaning, PaO2/FiO2 Ratio (PF), Transpulmonary pressure (TPP)
Extubation: Cuff Leak Test, Extubation Assessment in ED, Extubation Assessment in ICU, NIV for weaning, Post-Extubation Stridor, Spontaneous breathing trial, Unplanned extubation, Weaning from mechanical ventilation
Core Knowledge: Basics of Mechanical Ventilation, Driving Pressure, Dynamic pressure-volume loops, flow versus time graph, flow volume loops, Indications and complications, Intrinsic PEEP (autoPEEP), Oxygen Haemoglobin Dissociation Curve, Positive End Expiratory Pressure (PEEP), Pulmonary Mechanics, Pressure Vs Time Graph, Pressure vs Volume Loop, Setting up a ventilator, Ventilator waveform analysis, Volume vs time graph
Equipment: Capnography and CO2 Detector, Heat and Moisture Exchanger (HME), Ideal helicopter ventilator, Wet Circuit
MISC: Sedation in ICU, Ventilation literature summaries
Journal articles
- Holley AD, Boots RJ. Review article: management of acute severe and near-fatal asthma. Emerg Med Australas. 2009 Aug;21(4):259-68. doi: 10.1111/j.1742-6723.2009.01195.x. Review. PubMed PMID: 19682010. [Free Full Text]
- Stanley D, Tunnicliffe. Management of life-threatening asthma in adults. Contin Educ Anaesth Crit Care Pain (2008) 8 (3): 95-99. doi: 10.1093/bjaceaccp/mkn012 [Free Full Text]
- Wener RR, Bel EH. Severe refractory asthma: an update. Eur Respir Rev. 2013 Sep 1;22(129):227-35. doi: 10.1183/09059180.00001913. Review. PubMed PMID: 23997049. [Free Full Text]
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
