Intrinsic PEEP
OVERVIEW
Definition
- Intrinsic PEEP is also known as autoPEEP or PEEPi
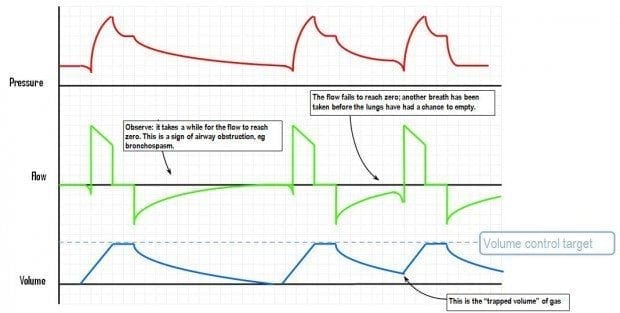
- Intrinsic PEEP occurs when the expiratory time is shorter than the time needed to fully deflate the lungs, preventing the lung and chest wall from reaching an elastic equilibrium point
- This is sometimes referred to as ‘gas trapping’
- ARDS or cardiogenic pulmonary oedema tend to have low levels of PEEPi (e.g. 3-4cmH20)
- asthma or COPD patient have higher levels of PEEPi (e.g. 14cmH2O), which is why they are susceptible to dynamic hyperinflation (‘breath stacking’ from incomplete exhalations) and its complications
MEASUREMENT
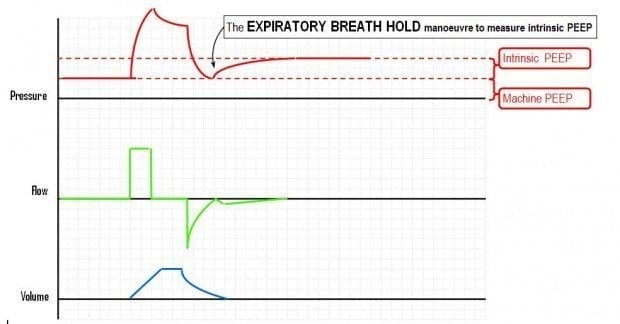
Expiratory hold manoeuvre
- PEEPi is measured by performing an end expiratory pause or hold manoeuvre
- expiratory circuit occlusion for 3-5 seconds allows alveolar pressure to equilibrate with airway pressure
Other methods
- Observe the expiratory flow curve, if there is ‘gas trapping’ the curve may not reach baseline
- Disconnect the circuit from the ETT to observe for a prolonged exhalation and audible wheeze. Resolved hypotension and decreased Pplat on reconnection suggests that dynamic hyperinflation causing high PEEPi was present
Limitations
- at the end of expiration the smaller airways may close preventing the over-pressurised alveoli to which they connect from equilibrating with the rest of the respiratory circuit. Thus the expiratory hold manoeuvre will underestimate the actual PEEPi
- Similarly, failure of the expiratory flow curve to reach baseline is an insensitive test
- Plateau pressure (Pplat) will also tend to increase as PEEPi increases, but this could also occur due to decreased lung compliance so increased PEEPi cannot be assumed
CAUSES OF INCREASED PEEPi
- increased expiratory resistance
- bronchospasm e.g. asthma, COPD
- narrowed/kinked ETT
- inspissated secretions
- exhalation valves
- HME filter
- impaired elastic recoil
- emphysema
- increased minute ventilation
- inadequate expiratory time
CONSEQUENCES OF HIGH PEEPi
Dynamic hyperinflation leads to excessively high PEEPi (‘breath stacking’ resulting in ‘gas trapping’)
- increased intrathoracic volume
-> increased pressures for given tidal volume
-> risk of barotrauma - increased intrathoracic pressure
-> decreased venous return, preload and cardiac output (e.g. hypotension post-intubation in severe asthma)
-> increased inspiratory work to trigger the ventilator
MANAGEMENT
- treat reversible factors (bronchospasm, secretions, expiratory devices)
- prolong expiratory time (decrease I:E ratio, decrease RR, increase inspiratory flow)
- decrease tidal volume
- measure PEEPi (expiratory hold)
- set exogenous PEEP to ~2/3 PEEPi, this will decrease inspiratory triggering work and improve distribution of inspired gas (others prefer a PEEP of zero, or ZEEP)
- if in doubt and dynamic hyperinflation is suspected, disconnect the ETT from the circuit to allow spontaneously exhalation, then reconnect to the ventilator
References and Links
CCC Ventilation Series
Modes: Adaptive Support Ventilation (ASV), Airway Pressure Release Ventilation (APRV), High Frequency Oscillation Ventilation (HFOV), High Frequency Ventilation (HFV), Modes of ventilation, Non-Invasive Ventilation (NIV), Spontaneous breathing and mechanical ventilation
Conditions: Acute Respiratory Distress Syndrome (ARDS), ARDS Definitions, ARDS Literature Summaries, Asthma, Bronchopleural Fistula, Burns, Oxygenation and Ventilation, COPD, Haemoptysis, Improving Oxygenation in ARDS, NIV and Asthma, NIV and the Critically Ill, Ventilator Induced Lung Injury (VILI), Volutrauma
Strategies: ARDSnet Ventilation, Open lung approach, Oxygen Saturation Targets, Protective Lung Ventilation, Recruitment manoeuvres in ARDS, Sedation pauses, Selective Lung Ventilation
Adjuncts: Adjunctive Respiratory Therapies, ECMO Overview, Heliox, Neuromuscular blockade in ARDS, Prone positioning and Mechanical Ventilation
Situations: Cuff leak, Difficulty weaning, High Airway Pressures, Post-Intubation Care, Post-intubation hypoxia
Troubleshooting: Autotriggering of the ventilator, High airway and alveolar pressures / pressure alarm, Ventilator Dyssynchrony
Investigation / Indices: A-a gradient, Capnography and waveforms, Electrical Impedance Tomography, Indices that predict difficult weaning, PaO2/FiO2 Ratio (PF), Transpulmonary pressure (TPP)
Extubation: Cuff Leak Test, Extubation Assessment in ED, Extubation Assessment in ICU, NIV for weaning, Post-Extubation Stridor, Spontaneous breathing trial, Unplanned extubation, Weaning from mechanical ventilation
Core Knowledge: Basics of Mechanical Ventilation, Driving Pressure, Dynamic pressure-volume loops, flow versus time graph, flow volume loops, Indications and complications, Intrinsic PEEP (autoPEEP), Oxygen Haemoglobin Dissociation Curve, Positive End Expiratory Pressure (PEEP), Pulmonary Mechanics, Pressure Vs Time Graph, Pressure vs Volume Loop, Setting up a ventilator, Ventilator waveform analysis, Volume vs time graph
Equipment: Capnography and CO2 Detector, Heat and Moisture Exchanger (HME), Ideal helicopter ventilator, Wet Circuit
MISC: Sedation in ICU, Ventilation literature summaries
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Auto-PEEP does not necessarily equate to dynamic hyperinflation. Longer time constant lung units can have autopeep when expiratory time is too short for the pressure in those lung units to fall to the PEEP at the trachea. This does not mean that the expiratory volume in those lung units is less than the inspiratory volume in those lung units. During general anaesthesia for patients with COPD, it is common to ventilate for hours with auto-PEEP evident on the expiratory flow curve and with no evidence of hyperinflation.