Pulmonary mechanics
OVERVIEW
Determining compliance and resistance within a respiratory system is important during the management of mechanical ventilation. Measurements that help us determine these include:
- -> tidal volume
- -> peak inspiratory flow rate
- -> peak airway pressure
- -> end-inspiratory plateau pressure
- -> end-expiratory pressure in circuit
- -> occult end-expiratory pressure measured during an end-expiratory pause maneuver.
COMPLIANCE
- change in volume/change in pressure
- can be static (when there is no air flow) or dynamic (during breathing – where airflow resistance becomes a factor)
- normal dynamic compliance during mechanical ventilation – 50-100mL/cmH2O
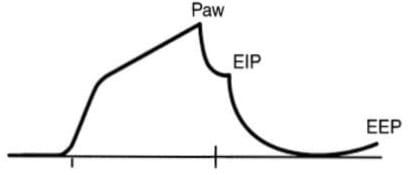
- when paralysed and mechanically ventilated, peak airway pressure = the force required to overcome resistive and elastic recoil of the lung and chest wall
- to distinguish resistive from elastic recoil-related pressures requires an introduction of an end-inspiratory circuit occlusion after VT delivery.
- peak pressure will decrease down to a stable plateau pressure (3 second hold) -> this corresponds to the elastic recoil pressure
“Quasi-static” Compliance = VT/Pplat – PEEPtotal
- when patient spontaneously breathing -> compliance becomes uncertain
- can decrease the pause time to 1 second but is difficult to measure
RESISTANCE
- Flow = change in pressure/resistance
- Resistance = change in pressure/flow
Respiratory system resistance
= Paw – Pplat/Peak inspiratory flow rate
- peak inspiratory flow rate = preocclusion flow rate and is expressed in terms of cmH20/L/second
- resistance is expressed as cmH20/L/second
- respiratory resistance can only be accurately determined with a constant inspiratory flow (square wave) pattern -> usually set at 1L/second when measuring resistance -> this happens to be a standard setting for patient comfort.
NORMAL AND PATHOLOGICAL STATES
- in mechanically ventilated, normal patients: compliance = 50-100mL/cmH20, resistance = 1-8cmH20/L/s
- ARDS or cardiogenic pulmonary oedema: low compliance (around 40mL/cmH2O), and elevated resistance (15cmmH2O/L/s).
- COPD or asthma: high compliance (66mL/cmH2O) and higher resistance (25cmH2O/L/s).
- restrictive lung disease = decreased compliance -> small, rapid breaths -> decrease WOB
- obstructive lung disease = increased compliance -> large, slow breaths -> decreased WOB
VIDEOS
Dr Eric Strong on Normal Lung Mechanics
Dr Eric Strong on Monitoring Lung Mechanics
References and Links
CCC Ventilation Series
Modes: Adaptive Support Ventilation (ASV), Airway Pressure Release Ventilation (APRV), High Frequency Oscillation Ventilation (HFOV), High Frequency Ventilation (HFV), Modes of ventilation, Non-Invasive Ventilation (NIV), Spontaneous breathing and mechanical ventilation
Conditions: Acute Respiratory Distress Syndrome (ARDS), ARDS Definitions, ARDS Literature Summaries, Asthma, Bronchopleural Fistula, Burns, Oxygenation and Ventilation, COPD, Haemoptysis, Improving Oxygenation in ARDS, NIV and Asthma, NIV and the Critically Ill, Ventilator Induced Lung Injury (VILI), Volutrauma
Strategies: ARDSnet Ventilation, Open lung approach, Oxygen Saturation Targets, Protective Lung Ventilation, Recruitment manoeuvres in ARDS, Sedation pauses, Selective Lung Ventilation
Adjuncts: Adjunctive Respiratory Therapies, ECMO Overview, Heliox, Neuromuscular blockade in ARDS, Prone positioning and Mechanical Ventilation
Situations: Cuff leak, Difficulty weaning, High Airway Pressures, Post-Intubation Care, Post-intubation hypoxia
Troubleshooting: Autotriggering of the ventilator, High airway and alveolar pressures / pressure alarm, Ventilator Dyssynchrony
Investigation / Indices: A-a gradient, Capnography and waveforms, Electrical Impedance Tomography, Indices that predict difficult weaning, PaO2/FiO2 Ratio (PF), Transpulmonary pressure (TPP)
Extubation: Cuff Leak Test, Extubation Assessment in ED, Extubation Assessment in ICU, NIV for weaning, Post-Extubation Stridor, Spontaneous breathing trial, Unplanned extubation, Weaning from mechanical ventilation
Core Knowledge: Basics of Mechanical Ventilation, Driving Pressure, Dynamic pressure-volume loops, flow versus time graph, flow volume loops, Indications and complications, Intrinsic PEEP (autoPEEP), Oxygen Haemoglobin Dissociation Curve, Positive End Expiratory Pressure (PEEP), Pulmonary Mechanics, Pressure Vs Time Graph, Pressure vs Volume Loop, Setting up a ventilator, Ventilator waveform analysis, Volume vs time graph
Equipment: Capnography and CO2 Detector, Heat and Moisture Exchanger (HME), Ideal helicopter ventilator, Wet Circuit
MISC: Sedation in ICU, Ventilation literature summaries
Journal articles
- Bersten AD. A simple bedside approach to measurement of respiratory mechanics in critically ill patients. Crit Care Resusc. 1999 Mar;1(1):74-84. PubMed PMID: 16599866. [Free Full Text]
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
