High airway and alveolar pressures
Reviewed and revised 22 December 2015
OVERVIEW
High airway pressures are important because they may:
- have adverse effects on the patient
- indicate a deterioration of the patient’s condition
- indicate an equipment problem that needs to be addressed
It is important to distinguish between airway pressure and alveolar pressure
AIRWAY PRESSURE AND ALVEOLAR PRESSURE
Airway pressure
airway pressure = flow x resistance + alveolar pressure
- Thus if flow or resistance is markedly altered, a change in airway pressure will not be indicative of a change in the alveolar pressure
- Airway pressure is more conveniently measured than alveolar pressure
- Peak inspiratory pressure (PIP) is displayed on most ventilators
- A maximum acceptable PIP of <35 cmH20 is widely used
Alveolar pressure
- Alveolar pressure is estimated by determining the inspiratory pause pressure, which corresponds to the plateau pressure
- The inspiratory pause pressure is determined by observing the plateau pressure in an apneic ventilated patient when when the ‘inspiratory pause hold‘ control is activated
- Because flow is reduced to zero, airway pressure and alveolar pressures will equalise and the airway pressure will correspond to the alveolar pressure at full inspiration
airway pressure = 0 x resistance + alveolar pressure = alveolar pressure
- To prevent lung injury, alveolar pressure (aka the plateau pressure) should be kept <30 cmH2O
- High alveolar pressures can be due to excessive tidal volume, gas trapping, PEEP or low compliance as shown by this relationship:
alveolar pressure = (volume/ compliance) + PEEP
PRESSURE-TIME CURVES SHOWING PIP AND PLATEAU PRESSURES IN VOLUME CONTROL VENTILATION
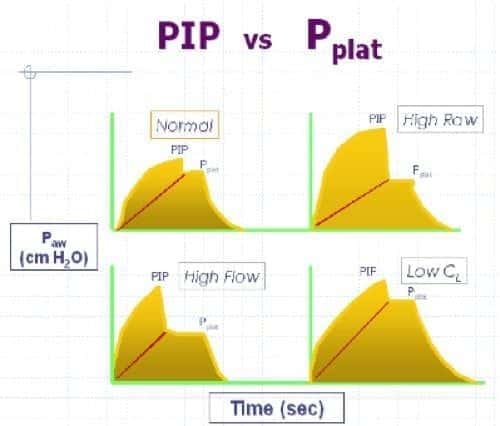
Normal curve – demonstrates normal PIP , Pplat , PTA (transairway pressure), and Ti (inspiratory time). High Raw curve – A significant increase in the PTA is associated with increased airway resistance. High Flow curve – the inspiratory time is shorter than normal, indicating a higher inspiratory gas flow rate. Decreased Lung Compliance curve – An increase in the plateau pressure and a corresponding increase in the PIP is consistent with decreased lung compliance.
EFFECTS OF HIGH PRESSURES
High airway pressure is not necessarily harmful, unless it reflects high alveolar pressure which can have these effects:
- barotrauma may result in acute lung injury (leading to ARDS) or air leaks (e.g. pneumothorax, pneumomediastinum)
- Excessive intrathoracic pressure may also result, with potential hemodynamic consequences (particularly decreased venous return, leading to hypotension and potentially cardiac arrest)
- High airway pressures may result in inadequate ventilation
Ventilator response to high airway pressures:
- Inadequate ventilation can occur because many ventilators are set to terminate the inspiratory flow if the upper pressure limit setting is reached. When this occurs inspiratory volumes are markedly reduced, resulting in low tidal volumes and minute ventilation
- Other ventilators do not do this but will simply hold the airway pressure at the pressure limit, resulting in a smaller reduction in tidal volume
There many also be other consequences of the underlying cause
CAUSES OF HIGH PRESSURES
- Think “Man versus machine”
First, let’s consider the machine:
- Ventilator
- inappropriate settings
- ventilator malfunction
- Circuit
- kinking
- pooling of condensed water vapour
- wet filters causing increased resistance
- Endotracheal tube
- displacement, e.g. endobronchial intubation
- kinking
- obstruction with foreign material
And now the man:
- bronchospasm (e.g. asthma)
- decreased compliance
- lung (e.g. collapse, consolidation, pulmonary edema, ARDS)
- pleural (e.g. pneumothorax, pleural effusion)
- chest wall (e.g. abdominal distention, kyhposcoliosis, obesity)
- patient-ventilator dysynchrony, coughing
APPROACH TO PATIENT WITH HIGH AIRWAY PRESSURES
- Disconnect the patient from the ventilator and manually bag the patient using high-flow oxygen and bag-valve-mask
- While the patient is disconnected from the ventilator assess the “feel” of the lungs while bagging:
- If the patient is not difficult to ventilate then the problem is with the ventilator or the circuit
- If the patient is difficult to ventilate it is a problem with the endotracheal tube or the respiratory system
- For ventilator and circuit problems:
- check the ventilator settings that it is functioning correctly (e.g. on a test lung)
- check the circuit for obstruction or kinking
- For patient or ETT problems:
- examine the patient looking for:
- wheeze
- asymmetrical chest expansion
- evidence of collapse
- evidence of dyssynchrony
- Pass a suction catheter through the ETT to check its patency
- Use ETCO2 and perform a CXR to check ETT position and look for potential causes of decreased compliance
- examine the patient looking for:
If the cause is still not clear measure inspiratory pause pressure to estimate alveolar pressure, in addition to the peak inspiratory pressure that reflects airway pressure.
- If both airway and alveolar pressure are high the problem is due to poor compliance (e.g. pulmonary edema)
- If only the airway pressure is high the problem is one of high resistance (e.g. bronchospasm)
Seek and treat underlying causes
References and Links
CCC Ventilation Series
Modes: Adaptive Support Ventilation (ASV), Airway Pressure Release Ventilation (APRV), High Frequency Oscillation Ventilation (HFOV), High Frequency Ventilation (HFV), Modes of ventilation, Non-Invasive Ventilation (NIV), Spontaneous breathing and mechanical ventilation
Conditions: Acute Respiratory Distress Syndrome (ARDS), ARDS Definitions, ARDS Literature Summaries, Asthma, Bronchopleural Fistula, Burns, Oxygenation and Ventilation, COPD, Haemoptysis, Improving Oxygenation in ARDS, NIV and Asthma, NIV and the Critically Ill, Ventilator Induced Lung Injury (VILI), Volutrauma
Strategies: ARDSnet Ventilation, Open lung approach, Oxygen Saturation Targets, Protective Lung Ventilation, Recruitment manoeuvres in ARDS, Sedation pauses, Selective Lung Ventilation
Adjuncts: Adjunctive Respiratory Therapies, ECMO Overview, Heliox, Neuromuscular blockade in ARDS, Prone positioning and Mechanical Ventilation
Situations: Cuff leak, Difficulty weaning, High Airway Pressures, Post-Intubation Care, Post-intubation hypoxia
Troubleshooting: Autotriggering of the ventilator, High airway and alveolar pressures / pressure alarm, Ventilator Dyssynchrony
Investigation / Indices: A-a gradient, Capnography and waveforms, Electrical Impedance Tomography, Indices that predict difficult weaning, PaO2/FiO2 Ratio (PF), Transpulmonary pressure (TPP)
Extubation: Cuff Leak Test, Extubation Assessment in ED, Extubation Assessment in ICU, NIV for weaning, Post-Extubation Stridor, Spontaneous breathing trial, Unplanned extubation, Weaning from mechanical ventilation
Core Knowledge: Basics of Mechanical Ventilation, Driving Pressure, Dynamic pressure-volume loops, flow versus time graph, flow volume loops, Indications and complications, Intrinsic PEEP (autoPEEP), Oxygen Haemoglobin Dissociation Curve, Positive End Expiratory Pressure (PEEP), Pulmonary Mechanics, Pressure Vs Time Graph, Pressure vs Volume Loop, Setting up a ventilator, Ventilator waveform analysis, Volume vs time graph
Equipment: Capnography and CO2 Detector, Heat and Moisture Exchanger (HME), Ideal helicopter ventilator, Wet Circuit
MISC: Sedation in ICU, Ventilation literature summaries
LITFL
- LITFL Pulmonary Puzzle 014 — Alarmingly high pressures
FOAM and web resources
- Gomersall C. ICU Web — Trouble-shooting mechanical ventilation
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
