Capnography Waveform Interpretation
OVERVIEW
- Capnography waveform interpretation can be used for diagnosis and ventilator-trouble shooting
- The CO2 waveform can be analyzed for 5 characteristics:–Height–Frequency–Rhythm–Baseline–Shape
NORMAL CAPNOGRAM
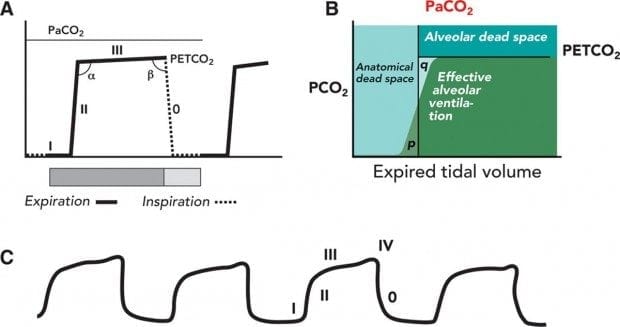
4 phases
- Phase I (inspiratory baseline) reflects inspired gas, which is normally devoid of carbon dioxide.
- Phase II (expiratory upstroke) is the transition between VDana, which does not participate in gas exchange, and alveolar gas from the respiratory bronchioles and alveoli.
- Phase III is the alveolar plateau. Traditionally, PCO2 of the last alveolar gas sampled at the airway opening is called the PETCO2.
- Phase 0 is the inspiratory downstroke, the beginning of the next inspiration
Other features:
- Normal end-tidal PCO2 is approximately: 38 mmHg or 5%
- the alpha angle is the transition from Phase II to Phase III
- the beta angle is the transition from Phase III to Phase 0 (the start of inspiration)
- an additional phase IV (terminal upstroke before phase 0) may be seen in pregnancy
ETCO2 only represents alveolar CO2 when a relatively horizontal plateau phase (phase III) is seen.
FLAT ETCO2 TRACE
- Ventilator disconnection
- Airway misplaced – extubation, oesophageal intubation
- Capnograph not connected to circuit
- Respiratory/Cardiac arrest
- Apnoea test in brain death dead patient
- Capnongraphy obstruction
INCREASED ETCO2
CO2 Production
- Fever
- Sodium bicarbonate
- Tourniquet release
- Venous CO2 embolism
- Overfeeding
Pulmonary perfusion
- Increased cardiac output
- Increased blood pressure
Alveolar ventilation
- Hypoventilation
- Bronchial intubation
- Partial airway obstruction
- Rebreathing
Apparatus malfunctioning
- Exhausted CO2 absorber
- Inadequate fresh gas flows
- Leaks in ventilator tubing
- Ventilator malfunctioning
DECREASED ETCO2
CO2 production
- Hypothermia
Pulmonary perfusion
- Reduced cardiac output
- Hypotension
- Hypovolaemia
- Pulmonary embolism
- Cardiac arrest
Alveolar ventilation
- Hyperventilation
- Apnoea
- Total airway obstruction (note high airway pressures)
- Extubation
Apparatus malfunctioning
- Circuit disconnection (note low airway pressures)
- Leaks in sampling tube
- Ventilator malfunctioning
SUDDEN DROP IN ETCO2 TO ZERO
- Kinked ET tube
- CO2 analyzer defective
- Total disconnection
- Ventilator defective
SUDDEN CHANGE IN BASELINE (NOT TO ZERO)
- Calibration error
- CO2 absorber saturated (check capnograph with room air)
- Water drops in analyzer or condensation in airway adapter
SUDDEN INCREASE IN ETCO2
- ROSC during cardiac arrest
- correction of ET tube obstruction
ELEVATED INSPIRATORY BASELINE
- CO2 rebreathing (e.g. soda lime exhaustion)
- Contamination of CO2 monitor (sudden elevation of base line and top line)
- Inspiratory valve malfunction (elevation of the base line, prolongation of down stroke, prolongation of phase III)
IMPORTANT PATTERNS TO RECOGNISE
See Figure 2 of Kodali 2013 and Interpret your capnogram at Capnography.com
- esophageal intubation (<6 waveforms of decreasing height)
- right main bronchus intubation (ETCO2 can increase, decrease or stay the same, can also cause a bifid capnogram)
- curare cleft (partially paralysed patient on mechanical ventilation)
- cardiogenic oscillations
- camel hump (seen in patients in lateral position)
- Rebreathing capnogram of Mapleson D circuit
- phase IV in pregnancy
- Dilution of expiratory gases by the forward flow of fresh gases during the later part of expiration when expiratory flow rate decreases below the forward gas flow rate
- sometimes see reverse phase 3 slope seen in patients with emphysema (alveolar destruction leads to rapid delivery of CO2 to airways)
- Sticking inspiratory valve
- expiratory valve malfunction
- mandatory versus spontaneously triggered breaths
- dual capnogram in lung transplants
- air leak
- malignant hyperthermia
- air / oxygen dilution during mask sampling of spontaneously breathing patients
References and Links
Introduction to ICU Series
Introduction to ICU Series Landing Page
DAY TO DAY ICU: FASTHUG, ICU Ward Round, Clinical Examination, Communication in a Crisis, Documenting the ward round in ICU, Human Factors
AIRWAY: Bag Valve Mask Ventilation, Oropharyngeal Airway, Nasopharyngeal Airway, Endotracheal Tube (ETT), Tracheostomy Tubes
BREATHING: Positive End Expiratory Pressure (PEEP), High Flow Nasal Prongs (HFNP), Intubation and Mechanical Ventilation, Mechanical Ventilation Overview, Non-invasive Ventilation (NIV)
CIRCULATION: Arrhythmias, Atrial Fibrillation, ICU after Cardiac Surgery, Pacing Modes, ECMO, Shock
CNS: Brain Death, Delirium in the ICU, Examination of the Unconscious Patient, External-ventricular Drain (EVD), Sedation in the ICU
GASTROINTESTINAL: Enteral Nutrition vs Parenteral Nutrition, Intolerance to EN, Prokinetics, Stress Ulcer Prophylaxis (SUP), Ileus
GENITOURINARY: Acute Kidney Injury (AKI), CRRT Indications
HAEMATOLOGICAL: Anaemia, Blood Products, Massive Transfusion Protocol (MTP)
INFECTIOUS DISEASE: Antimicrobial Stewardship, Antimicrobial Quick Reference, Central Line Associated Bacterial Infection (CLABSI), Handwashing in ICU, Neutropenic Sepsis, Nosocomial Infections, Sepsis Overview
SPECIAL GROUPS IN ICU: Early Management of the Critically Ill Child, Paediatric Formulas, Paediatric Vital Signs, Pregnancy and ICU, Obesity, Elderly
FLUIDS AND ELECTROLYTES: Albumin vs 0.9% Saline, Assessing Fluid Status, Electrolyte Abnormalities, Hypertonic Saline
PHARMACOLOGY: Drug Infusion Doses, Summary of Vasopressors, Prokinetics, Steroid Conversion, GI Drug Absorption in Critical Illness
PROCEDURES: Arterial line, CVC, Intercostal Catheter (ICC), Intraosseous Needle, Underwater seal drain, Naso- and Orogastric Tubes (NGT/OGT), Rapid Infusion Catheter (RIC)
INVESTIGATIONS: ABG Interpretation, Echo in ICU, CXR in ICU, Routine daily CXR, FBC, TEG/ROTEM, US in Critical Care
ICU MONITORING: NIBP vs Arterial line, Arterial Line Pressure Transduction, Cardiac Output, Central Venous Pressure (CVP), CO2 / Capnography, Pulmonary Artery Catheter (PAC / Swan-Ganz), Pulse Oximeter
CCC Ventilation Series
Modes: Adaptive Support Ventilation (ASV), Airway Pressure Release Ventilation (APRV), High Frequency Oscillation Ventilation (HFOV), High Frequency Ventilation (HFV), Modes of ventilation, Non-Invasive Ventilation (NIV), Spontaneous breathing and mechanical ventilation
Conditions: Acute Respiratory Distress Syndrome (ARDS), ARDS Definitions, ARDS Literature Summaries, Asthma, Bronchopleural Fistula, Burns, Oxygenation and Ventilation, COPD, Haemoptysis, Improving Oxygenation in ARDS, NIV and Asthma, NIV and the Critically Ill, Ventilator Induced Lung Injury (VILI), Volutrauma
Strategies: ARDSnet Ventilation, Open lung approach, Oxygen Saturation Targets, Protective Lung Ventilation, Recruitment manoeuvres in ARDS, Sedation pauses, Selective Lung Ventilation
Adjuncts: Adjunctive Respiratory Therapies, ECMO Overview, Heliox, Neuromuscular blockade in ARDS, Prone positioning and Mechanical Ventilation
Situations: Cuff leak, Difficulty weaning, High Airway Pressures, Post-Intubation Care, Post-intubation hypoxia
Troubleshooting: Autotriggering of the ventilator, High airway and alveolar pressures / pressure alarm, Ventilator Dyssynchrony
Investigation / Indices: A-a gradient, Capnography and waveforms, Electrical Impedance Tomography, Indices that predict difficult weaning, PaO2/FiO2 Ratio (PF), Transpulmonary pressure (TPP)
Extubation: Cuff Leak Test, Extubation Assessment in ED, Extubation Assessment in ICU, NIV for weaning, Post-Extubation Stridor, Spontaneous breathing trial, Unplanned extubation, Weaning from mechanical ventilation
Core Knowledge: Basics of Mechanical Ventilation, Driving Pressure, Dynamic pressure-volume loops, flow versus time graph, flow volume loops, Indications and complications, Intrinsic PEEP (autoPEEP), Oxygen Haemoglobin Dissociation Curve, Positive End Expiratory Pressure (PEEP), Pulmonary Mechanics, Pressure Vs Time Graph, Pressure vs Volume Loop, Setting up a ventilator, Ventilator waveform analysis, Volume vs time graph
Equipment: Capnography and CO2 Detector, Heat and Moisture Exchanger (HME), Ideal helicopter ventilator, Wet Circuit
MISC: Sedation in ICU, Ventilation literature summaries
Journal articles
- Blanch L, Romero PV, Lucangelo U. Volumetric capnography in the mechanically ventilated patient. Minerva Anestesiol. 2006 Jun;72(6):577-85. PMID: 16682932.
- Kodali BS. Capnography outside the operating rooms. Anesthesiology. 2013 Jan;118(1):192-201. PMID: 23221867.
- Thompson JE, Jaffe MB. Capnographic waveforms in the mechanically ventilated patient. Respir Care. 2005 Jan;50(1):100-8; discussion 108-9.PMID: 15636648.
FOAM and web resources
- Capnography.com (the neon e-bible of capnography!)
- KI Doc — So much hot gas – ETCO2 for non-anaesthetists (2013)
- Smalhout B. A Quick Guide to Capnography (2004)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

[…] https://litfl.com/capnography-waveform-interpretation/ […]