Bilirubin and Jaundice
Bilirubin and Jaundice
Unconjugated hyperbilirubinaemia
- Pre-hepatic (acholuric)
- Hepatocellular
Conjugated hyperbilirubinaemia
- Hepatocellular
- Intrahepatic obstruction
- Extrahepatic obstruction
Note:
- <20% of bilirubin conjugated = Unconjugated hyperbilirubinaemia
- >50% of bilirubin conjugated = Conjugated hyperbilirubinaemia
Unconjugated hyperbilirubinaemia
Classification:
- Pre-hepatic (acholuric) (vast majority. Secondary to increased bilirubin production
- Hepatocellular. Secondary to reduced hepatocyte uptake of bilirubin.
Cause:
- Haemolysis (must be 2 x normal to be significant) – Rarely causes rise over 70 micromol/L
- haemolytic anaemia
- erythroblastosis foetalis
- pernicious of prematurity
- Congenital
- Gilbert disease (GD)
- Crigler-Najjar syndrome (CS)
- Iatrogenic
- Drugs: chloramphenicol, gentamicin, pregnanediol
- Physiological
- Neonatal jaundice and Breast-milk jaundice
Conjugated hyperbilirubinaemia
- Hepatocellular – Diminished hepatocyte function. If severe can be associated with unconjugated hyperbilirubinemia due to total inability to conjugate bilirubin
- hepatitis – Viral, toxic, alcoholic, autoimmune
- cirrhosis
- leptospirosis
- Drugs
- liver parenchymal injury (toxic hepatitis)
- halothane, paracetamol, methyldopa, phenytoin, barbiturates, MAOI, sulphonamides
- Intrahepatic obstruction (hepatic canalicular disorders)
- Hepatitis (viral)
- Cirrhosis (Primary biliary cirrhosis)
- Intrahepatic cholestasis
- Drugs
- indomethacin, erythromycin
- chlorpromazine, isoniazid, flucloxacillin, OCP
- Congenital
- Dubin–Johnson syndrome
- Rotor syndrome
- Extrahepatic obstruction
- Calculi, tumour, scar tissue in common bile duct or hepatic excretory duct
- Gallstones, carcinoma of head of pancreas and lymphoma with extrinsic nodal compression of the porta hepatis are commonest
Serum Bilirubin
Measures unconjugated and conjugated (Normal range: 6-24 micromol/L). Initial result details TOTAL bilirubin measured
- Clinically detectable jaundice
- Conjugated hyperbilirubinaemia – 35 micromol/L
- Unconjugated hyperbilirubinaemia – 45 micromol/L
- Ratio of unconjugated and conjugated helps to determine cause of hyperbilirubinaemia
- Predominantly unconjugated (<20% bilirubin conjugated)
- Predominantly conjugated (>50% bilirubin conjugated)
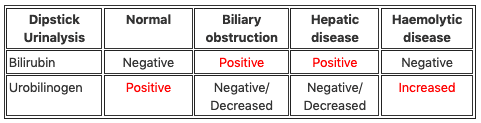
Urine Bilirubin
Ward Test Urine (WTU) or laboratory for may assess urine for Urine bilirubin and Urine urobilinogen
Urine bilirubin:
- Conjugated bilirubin excreted into GIT is reabsorbed in very small amounts
- Kidneys filter soluble form and it appears in urine
- Bilirubin is NOT normally present in urine
- Urine -dark in colour, usually brown with yellow foam
- Presence of bilirubin implies Conjugated hyperbilirubinemia
Urine urobilinogen:
- Normal: 1-4mg/day (compared to 250mg in stool)
- Absence of urobilinogen
- Conjugated – Complete extrahepatic obstruction or Broad spectrum antibiotics destroying intestinal flora
- Low levels of urobilinogen
- Unconjugated – Congenital (Crigler-Najjar syndrome, Gilbert syndrome)
- Conjugated – Complete extrahepatic obstruction
- Increased levels
- Unconjugated – haemolysis, highly alkaline urine or eating bananas up to 48 hours before test
[cite]

Critical Care
Compendium
