Metaraminol
Aka. Aramine, Metaradrine, Pressonex
QUICK REFERENCE
- Draw up into a 10 or 20 mL syringe with concentration of 0.5 mg/mL
- Use aliquots of 1 – 2 mL (0.5 – 1 mg) for adults every 1 – 2 minutes targeting desired MAP
- After bolus, could start infusion
- Can use peripherally
CLASS
- Sympathomimetic amine (direct and indirect)
- Synthetic phenylethylamine derivate
- Vasopressor
CHEMICAL STRUCTURE
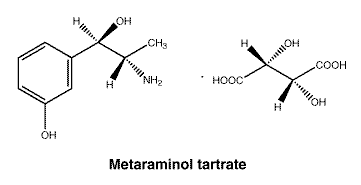
- Phenolic hydroxyl group: Enhances binding to α₁-adrenergic receptors, contributing to vasoconstrictive effects.
- Amino group: Facilitates interaction with adrenergic receptors and contributes to indirect sympathomimetic activity.
- Hydroxyl group on beta carbon of ethylamine side chain: Increases polarity and water solubility, aiding in intravenous administration.
- Methyl group substituent on the alpha carbon of the ethylamine side chain: relative resistance to MAO metabolism, resulting in a longer elimination half-time, and greater degree of indirect sympathomimetic activity (i.e. release of noradenaline from storage sites)
MECHANISM OF ACTION
- Direct effects:
- ɑ1 adrenergic receptor agonist: causes vasoconstriction.
- Mild β-agonist
- Indirect effects:
- stimulates noradrenaline & adrenaline release from intracytoplasmic stores
- Anatomic locations: Acts on vascular smooth muscle cells in peripheral blood vessels.
- Second messenger pathways: Activation of alpha-1 receptors (Gq GPCRs) increases intracellular calcium via the phospholipase C pathway, resulting in smooth muscle contraction.
- Pharmacodynamics:
- Increases systemic vascular resistance (SVR) and increases blood pressure (DBP, SBP, and MAP)
- Positive inotropy
- Variable effect on heart rate ( β-agonist effect counter balanced by reflex bradycardia)
- CO unchanged or slightly decreased (due to increased SVR and afterload)
- Increased coronary blood flow (due to increased DBP and reflex bradycardia), however, coronary vasopasm (ɑ1/2 agonist effect) also reported (Kovoor et al, 2024)
- Rapid onset 1-2 minutes, peak effect 10 min, duration 20-60min
PHARMACEUTICS
- Vial of 10 mg in 1 mL, pre-filled syringe with a concentration of 0.5 mg/mL (commonly a 6 mL syringe in Australia)
- Clear colourless solution
- Keep out of direct light
- Keep below 25oC
- Infusion stable for up to 24 hours
- Excipients include: sodium chloride and sodium metabisulfite
- Diluted for use (usually saline)
- Weak base with pKa 8.6
ADMINISTRATION / DOSING
- Intravenous (IV) peripherally
- Usually prepared in a 0.5 mg / mL concentration, in 10 – 60 mL syringes
- Boluses:
- Adults: 0.5 – 1 mg (1 – 2 mL of standard strength as above) every 1 – 2 min
- Children: 5 – 10 microgs/kg every 1 – 2 min
- Infusion:
- Adults: start at 0.05 mg/kg/h and titrate to effect every 1-2 min (usually 0.5-10 mg/h IV infusion)
- Children: start at 5 microgs/kg/min and titrate to effect every 1-2 min
- With multiple boluses or an infusion, it is recommended to use an arterial line to assist with appropriate titration as well as continuous ECG monitoring
- Metaraminol is compatible with most IV fluids, check for drug specific incompatibilities, although it does include:
- Atropine and furosemide. Check for other less frequently used medications.
- It is preferable to not use via Y-site as it may result in changed infusion rate if using as an infusion (this goes for all vasopressor/-dilator infusions)
- Can be given peripherally IV (if infusion, usually <24h)
- IM or SC routes can also be used (rarely), 2-10mg IM / SC boluses.
INDICATIONS
- Commonly used to offset vasodilatory effects of sedatives/ anaesthetic agents (incl. Neuraxial blockade)
- Empiric treatment of acute hypotension (“push dose pressor”)
- Short-term infusion for vasoplegia/ vasodilation (e.g. mild hypotension due to urosepsis)
CONTRAINDICATIONS
- Hypersensitivity to sulfites
- Concomitant use of halothane or cyclopropane anaesthesia
DRUG-DRUG INTERACTIONS
- Monoamine Oxidase Inhibitors (MAOIs): Risk of hypertensive crisis due to enhanced catecholamine effects (e.g., phenelzine, tranylcypromine, selegiline, linezolid)
- Digoxin: risk of ectopics
- Catecholamines and sympathomimetics: combinatorial effects
ADVERSE EFFECTS
- Common:
- Cardiovascular: Hypertension, reflex bradycardia.
- Headaches, dizziness, nausea & vomiting, tremor
- RESP: slight increase in TV and decrease in RR
- CNS: Decreased cerebral blood flow and oxygen consumption.
- GI: Constriction of mesenteric vessels causing reduced splanchnic and hepatic blood flow.
- RENAL: Reduced renal blood flow.
- OB/GYN: Contraction of pregnant uterus. Reduced uterine artery blood flow.
- METABOLIC: Hyperglycaemia, increased glycogenolysis, inhibits insulin release.
- OTHER: increased body temperature, increased VO2
- Tachyphylaxis can occur with repeated/prolonged administration
- Extravasation injury leading to tissue injury is extremely rare (indeed, metaraminol has also been administered via the SC route!)
- Life-threatening:
- Cardiovascular: Severe hypertension, heart failure (e.g. LVF due to sudden increase in BP), arrhythmias
- Hypersensitivity (e.g. anaphylaxis)
PHARMACOKINETICS
- Pharmacokinetic data are limited
- Absorption
- Oral bioavailability is about 15-20% (although the oral route is not recommended)
- IV onset after 1 – 2 min; dealyed for IM (~10 min) and SC (~5-20 min)
- Distribution
- Limited information. 45% protein binding. Does not cross BBB.
- Metabolism
- Metabolism in the liver (although does not need dose adjustment in hepatic failure)
- Elimination
- T1/2 = 20 – 60 min
- Renal mostly as metabolites (does not need dose adjustment in renal failure), and bile as metabolites
PREGNANCY AND LACTATION
- Pregnancy: Category C. No well controlled studies in pregnant women. Metaraminol may cause fetal hypoxia by constricting the uterine vessels thereby limiting placental perfusion.
- Lactation: Not recommended; not known if secreted into milk and effects on the nursing infant are unknown.
DOSE ADJUSTMENTS IN ORGAN FAILURES
- Renal Impairment: No specific dose adjustment required.
- Liver Impairment: No specific dose adjustment required.
- Renal Replacement Therapy: No specific dose adjustment required.
EVIDENCE AND CONTROVERSIES
- Metaraminol is widely used in critical care settings (especially in the UK and ANZ) despite a paucity of evidence for efficacy and safety (Grauslyte et al, 2022; Anderson & Chatha, 2017)
- Over 10% of critical care patients with hypotension are treated with metaraminol in ANZ ICUs (Zimsen et al ,2024). They tend to have milder illness, metaraminol is started early in their illness and continued for <24h, and 2/3 not require other vasopressors (Zimsen et al, 2024).
TIPS AND PITFALLS
- Median dose equivalence for metaraminol and noradrenaline is 12.5:1 (Costa-Pinto et al, 2024). However, there is significant variance in dose equivalence and conversion-associated hypotension is common.
REFERENCES AND LINKS
CCC Pharmacology Series
Respiratory: Bosentan, Delivery of B2 Agonists in Intubated Patients, Nitric Oxide, Oxygen, Prostacyclin, Sildenafil
Cardiovascular: Adenosine, Adrenaline (Epinephrine), Amiodarone, Classification of Vasoactive drugs, Clevidipine, Digoxin, Dobutamine, Dopamine, Levosimendan, Levosimendan vs Dobutamine, Milrinone, Noradrenaline, Phenylephrine, Sodium Nitroprusside (SNiP), Sotalol, Vasopressin
Neurological: Dexmedetomidine, Ketamine, Levetiracetam, Lignocaine, Lithium, Midazolam, Physostigmine, Propofol, Sodium Valproate, Sugammadex, Thiopentone
Endocrine: Desmopressin, Glucagon Therapy, Medications and Thyroid Function
Gastrointestinal: Octreotide, Omeprazole, Ranitidine, Sucralfate, Terlipressin
Genitourinary: Furosemide, Mannitol, Spironolactone
Haematological: Activated Protein C, Alteplase, Aprotinin, Aspirin, Clopidogrel, Dipyridamole, DOACs, Factor VIIa, Heparin, LMW Heparin, Protamine, Prothrombinex, Tenecteplase, Tirofiban, Tranexamic Acid (TXA), Warfarin
Antimicrobial: Antimicrobial Dosing and Kill Characteristics, Benzylpenicillin, Ceftriaxone, Ciprofloxacin, Co-trimoxazole / Bactrim, Fluconazole, Gentamicin, Imipenem, Linezolid, Meropenem, Piperacillin-Tazobactam, Rifampicin, Vancomycin
Analgesic: Alfentanil, Celecoxib, COX II Inhibitors, Ketamine, Lignocaine, Morphine, NSAIDs, Opioids, Paracetamol (Acetaminophen), Paracetamol in Critical Illness, Tramadol
Miscellaneous: Activated Charcoal, Adverse Drug Reactions, Alkali Therapies, Drug Absorption in Critical Illness, Drug Infusion Doses, Epidural Complications, Epidural vs Opioids in Rib Fractures, Magnesium, Methylene Blue, Pharmacology and Critical Illness, PK and Obesity, PK and ECMO, Sodium Bicarbonate Use, Statins in Critical Illness, Therapeutic Drug Monitoring, Weights in Pharmacology
Toxicology: Digibind, Flumazenil, Glucagon Therapy, Intralipid, N-Acetylcysteine, Naloxone, Propofol Infusion Syndrome
REFERENCES
Journal articles
- Anderson K, Chatha H. BET 3: Peripheral metaraminol infusion in the emergency department. Emerg Med J. 2017 Mar;34(3):190-192. doi: 10.1136/emermed-2017-206590.3. PMID: 28232631; PMCID: PMC5502235.
- Costa-Pinto R, Neto AS, Matthewman MC, Osrin D, Liskaser G, Li J, Young M, Jones D, Udy A, Warrillow S, Bellomo R. Dose equivalence for metaraminol and noradrenaline – A retrospective analysis. J Crit Care. 2024 Apr;80:154430. doi: 10.1016/j.jcrc.2023.154430. PMID: 38245376.
- Kovoor JG, Gorman D, Warwick N, Sivagangabalan G, Kovoor P. Metaraminol-induced coronary vasospasm masquerading as ST-elevation myocardial infarction during general anaesthesia. Br J Anaesth. 2024 May;132(5):998-1000. doi: 10.1016/j.bja.2024.01.045. Epub 2024 Mar 23. PMID: 38521657.
- Grauslyte L, Bolding N, Phull M, Jovaisa T. The Use of Metaraminol as a Vasopressor in Critically Unwell Patients: A Narrative Review and a Survey of UK Practice. J Crit Care Med (Targu Mures). 2022 Aug 12;8(3):193-203. doi: 10.2478/jccm-2022-0017. PMID: 36062042; PMCID: PMC9396948.
- Zimsen T, Quick L, White G, Costa-Pinto R, Whebell S, Meyer J, McCullough J, Shekar K, Laupland KB, Ramanan M, Blank S, Tabah A, Luke S, Garrett P, Attokaran AG, Kumar A, White KC; Queensland Critical Care Research Network (QCCRN). Prevalence and characteristics of metaraminol usage in a large intensive care patient cohort. A multicentre, retrospective, observational study. Crit Care Resusc. 2025 Jun 23;27(2):100112. doi: 10.1016/j.ccrj.2025.100112. PMID: 40642118; PMCID: PMC12242419.
Textbooks
- Australian Injectable Drugs Handbook, 8th Edition. (2025). Retrieved 04 May 2025, from https://aidh.hcn.com.au/
- Australian Medicines Handbook. (2025). Retrieved 04 May 2025, from https://amhonline.amh.net.au/
- Brunton LL, Knollmann BC, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 14th ed. New York, NY: McGraw Hill; 2023.
- eMIMS Elite (2025). Retrieved 04 May 2025, from https://app.emimselite.com.acs.hcn.com.au
- IBM Micromedex. (2025). Retrieved 04 May 2025, from https://www.micromedexsolutions.com
- Scarth E, Smith S. Drugs in Anaesthesia and Intensive Care. 5th ed. Oxford, UK: Oxford University Press; 2016.
- Vanderah TW. Katzung’s Basic and Clinical Pharmacology. 16th ed. New York, NY: McGraw Hill; 2023.
FOAM and web resources
- Deranged Physiology – Metaraminol
- TGA Product Information Sheet – Metaraminol
Cite this article as: Pearlman, J.; Nickson, C.P. (2025, Jul 17). Metaraminol. Life in the Fast Lane. https://litfl.com/metaraminol/

Critical Care
Compendium
FCICM MMed(CritCare) BMed BMedSci
Staff Specialist in Intensive Care at Concord Repatriation General Hospital, and Postgraduate Fellow in Trauma at Royal North Shore Hospital
Grew up on a broadacre farm and found himself in a metropolitan ICU decades later. Always trying to make medical education more interesting and appropriately targeted; pre-hospital and retrieval curious; passionate about equitable access to healthcare; always looking forward to sitting on a tractor at harvest time. Student of LITFL.
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

