Pharmacokinetics and ECMO
OVERVIEW
- ECMO support has potential implications for pharmacotherapy in the critically ill, the significance of which are poorly defined
- Pharmacokinetic effects of ECMO vary with:
- different drugs and drug characteristics
- different types and compositions of ECMO circuit components
- The effect of ECMO on pharmacokinetics may contribute to
- therapeutic failure
- drug toxicity, and/or
- antimicrobial resistance
CHARACTERISTICS OF PATIENTS RECEIVING ECMO
- severe critically illness, with either respiratory failure (VV-ECMO) or circulatory failure (VA-ECMO), or both
- multi-organ dysfunction syndrome (MODS) is common (including AKI and the need for RRT)
- presence of an extracoporeal circuit (oxygenator, pump, circuit tubing and cannulae)
- drug sequestration in extracorporeal circuit
- increased volume of distribution and hemodilution
- altered blood flow (may be non-pulsatile in VA-ECMO; regional differences)
- SIRS response to extracoporeal circuit
- often receiving multiple medications, with potential for drug interactions
PHARMACOKINETIC EFFECTS OF ECMO
Mixing of priming volume with the patient’s own blood volume increase effective circulating volume
- causes acute hemodilution and decrease in total blood concentration of drugs
- pharmacological impact depends on:
- apparent volume of distribution (Vd) of the drugs
- degree of protein binding, and
- the extent of equilibration between tissue and plasma concentrations on initiation of ECMO
- Drugs with small Vd (e.g. gentamicin) are significantly affected compared to drugs with large Vd (e.g. amiodarone)
- Depletion of plasma protein (e.g. albumin) may affect plasma and tissue protein binding and plasma concentrations of drugs (typically transient due to administration of albumin and blood products)
Changes in blood flow affect clearance of drugs during ECMO
- Non-pulsatile flow in VA-ECMO can alter perfusion of tissues, reduce capillary circulation and aerobic metabolism
- Kidneys interpret pulseless blood flow as hypotension thus activating the renin-angiotensin system (leads to reduced urine production and impaired sodium excretion)
- Regional blood flow changes in the liver can affect drug clearance (especially those with a high extraction ratio e.g. propranolol)
- Decreased pulmonary blood flows, especially during VA ECMO, may affect sequestration and metabolism of many sedative and analgesic drugs by the lungs
- SIRS response to ECMO results in autonomic, endocrine and local cytokine factors that alter tissue distribution of drugs as well as clearance
Drug adsorption to components of the ECMO circuit
- Drug properties may influence the degree of binding to the circuit components
- Important drug properties include:
- molecular size
- degree of ionization
- lipophilicity
- plasma protein binding
- the circuit may continue to release the sequestrated molecules once a particular drug infusion is ceased
- it is unclear how priming of a circuit with different fluids affects drug sequestration
- Centrifugal pump circuits with hollow-fibre membrane oxygenators show less absorption for all drugs, most pronounced for lipophilic drugs
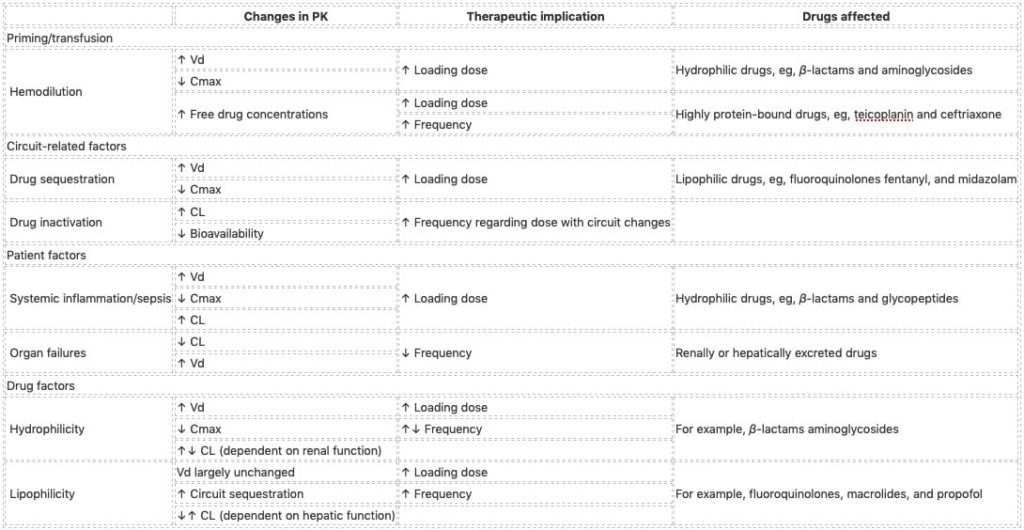
Summary table from Shekar et al (2012):
SPECIFIC DRUGS
Some examples:
- Antifungals — voriconazole is sequestered; caspofungin is usual dose
- Sedatives — Midazolam hashigher Vd and CL on ECMO, absorptive drug loss could be a cause of higher dose requirements. Propofol, which is lipophilic and highly protein bound, is significantly sequestered in the circuit
- Analgesics — fentanyl extensively binds to ECMO circuit after 24h, requiring higher doses; morphine preferred for longer term use
DRUG DOSING CONSIDERATIONS
From Erstad (2015):
- Drug dosing recommendations for an adult on ECMO are unlikely to be evidenced-based
- Data from neonatal case reports, case series or studies may not apply to adults
- Data from one drug may not be applicable to another even from the same class
- Drug regimen recommendations in critical care guidelines may not apply to patients on ECMO
- Organ dysfunction apart from the lung and heart complicate interpretation of literature
- The contribution of distinct physicochemical properties of drugs to sequestration is unclear
- Hydrophilicity or lipophilicity appear to be important factors affecting pharmacokinetics
- The therapeutic actions of drugs are not consistently predictable by pharmacokinetics
- The design and properties of the equipment change over time with implications for dosing
- The priming solution such as blood or blood-derived products may affect dosing
Therapeutic implications
- pharmacokinetic effects of ECMO are less problematic for drugs that can be titrated to endpoints (e.g. vasopressors, sedation), but are problematic for those that cannot (e.g. antibiotics)
- use therapeutic drug monitoring to individualise pharmacotherapy of ECMO patients if possible
References and Links
CCC Pharmacology Series
Respiratory: Bosentan, Delivery of B2 Agonists in Intubated Patients, Nitric Oxide, Oxygen, Prostacyclin, Sildenafil
Cardiovascular: Adenosine, Adrenaline (Epinephrine), Amiodarone, Classification of Vasoactive drugs, Clevidipine, Digoxin, Dobutamine, Dopamine, Levosimendan, Levosimendan vs Dobutamine, Milrinone, Noradrenaline, Phenylephrine, Sodium Nitroprusside (SNiP), Sotalol, Vasopressin
Neurological: Dexmedetomidine, Ketamine, Levetiracetam, Lignocaine, Lithium, Midazolam, Physostigmine, Propofol, Sodium Valproate, Sugammadex, Thiopentone
Endocrine: Desmopressin, Glucagon Therapy, Medications and Thyroid Function
Gastrointestinal: Octreotide, Omeprazole, Ranitidine, Sucralfate, Terlipressin
Genitourinary: Furosemide, Mannitol, Spironolactone
Haematological: Activated Protein C, Alteplase, Aprotinin, Aspirin, Clopidogrel, Dipyridamole, DOACs, Factor VIIa, Heparin, LMW Heparin, Protamine, Prothrombinex, Tenecteplase, Tirofiban, Tranexamic Acid (TXA), Warfarin
Antimicrobial: Antimicrobial Dosing and Kill Characteristics, Benzylpenicillin, Ceftriaxone, Ciprofloxacin, Co-trimoxazole / Bactrim, Fluconazole, Gentamicin, Imipenem, Linezolid, Meropenem, Piperacillin-Tazobactam, Rifampicin, Vancomycin
Analgesic: Alfentanil, Celecoxib, COX II Inhibitors, Ketamine, Lignocaine, Morphine, NSAIDs, Opioids, Paracetamol (Acetaminophen), Paracetamol in Critical Illness, Tramadol
Miscellaneous: Activated Charcoal, Adverse Drug Reactions, Alkali Therapies, Drug Absorption in Critical Illness, Drug Infusion Doses, Epidural Complications, Epidural vs Opioids in Rib Fractures, Magnesium, Methylene Blue, Pharmacology and Critical Illness, PK and Obesity, PK and ECMO, Sodium Bicarbonate Use, Statins in Critical Illness, Therapeutic Drug Monitoring, Weights in Pharmacology
Toxicology: Digibind, Flumazenil, Glucagon Therapy, Intralipid, N-Acetylcysteine, Naloxone, Propofol Infusion Syndrome
LITFL
- CCC – Everything ECMO
- CCC – ECMO troubleshooting
- CCC – Own the ECMO (presentation by Hergen Buescher, 2011)
Journal articles
- Erstad BL. Designing drug regimens for special intensive care unit populations. World journal of critical care medicine. 4(2):139-51. 2015. [pubmed]
- Mousavi S, Levcovich B, Mojtahedzadeh M. A systematic review on pharmacokinetic changes in critically ill patients: role of extracorporeal membrane oxygenation. Daru : journal of Faculty of Pharmacy, Tehran University of Medical Sciences. 19(5):312-21. 2011. [pubmed]
- Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. Journal of critical care. 27(6):741.e9-18. 2012. [pubmed]
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
