Thoracic Epidural Analgesia for Chest Trauma
OVERVIEW
- rib fractures are associated with significant morbidity, especially in the elderly and especially if multiple fractures are present.
- apart from being humane, optimal analgesia may help prevent respiratory deterioration
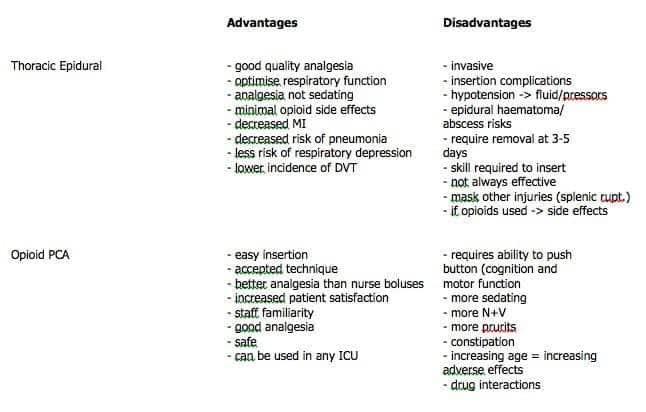
PROS AND CONS OF TEA VERSUS OPIOID PCA
CONSIDERATIONS FOR TEA
- other injuries need to be accounted for that may have implications (spinal injuries, intra-abdominal injury – though abdo pain from intra-abdo injury not likely to be totally masked by epidural local anaesthetic)
- coagulopathy is a contraindication
- epidural local anaesthetic / opiate combination at thoracic level likely to be associated with hypotension / bradycardia, needing volume and likely inotropic support
- consideration for infusion vrs bolus vrs PCEA
- other epidural analgesics – opiate alone eg fentanyl, pethidine or epidural clonidine – doses and frequency need consideration
- consider whether paravertebral is more appropriate
COMPLICATIONS OF TEA
- hypotension, bradycardia
- masking of other injuries and evolving neurological signs
- inadequate analgesia due to limited / patchy block
- increased pain in unblocked areas (relative phenomenon esp with bony injury eg shoulder
- short duration of blockade possible (usually removed at 3 days – then what?)
- epidural haematoma or abscess
- – drug side effects eg pruritis, nausea, respiratory depression
- – hypotension on mobilisation
- – respiratory muscle weakness
EVIDENCE
For thoracic epidural anesthesia/ analgesia:
- TEA for open abdominal aortic surgery reduces the duration of tracheal intubation and mechanical ventilation, as well as the incidence of MI, acute respiratory failure, GI complications and renal insufficiency (Level 1)
- High TEA used for CABG reduces postoperative pain, risk of dysrhythmias, pulmonary complications and time to extubation when compared with IV opioid analgesia (Level 1)
- Epidural local anaesthetics improve oxygenation and reduce pulmonary infections and other pulmonary complications compared with parenteral opioids (Level I)
- TEA improves bowel recovery after abdominal surgery (including colorectal surgery Level I).
- TEA extended for more than 24 hours reduces the incidence of postoperative MI (Level I)
- TEA reduces need for ventilation in patients with multiple rib fractures (Level I) and reduces incidence of pneumonia (Level II)
- Compared with TEA, continuous thoracic paravertebral analgesia results in comparable analgesia but has a better side effect profile (less urinary retention, hypotension, nausea, and vomiting) than epidural analgesia and leads to a lower incidence of postoperative pulmonary complications (Level I)
VIDEO
Thoracic epidural anesthesia by the ERS:
References and Links
CCC Pharmacology Series
Respiratory: Bosentan, Delivery of B2 Agonists in Intubated Patients, Nitric Oxide, Oxygen, Prostacyclin, Sildenafil
Cardiovascular: Adenosine, Adrenaline (Epinephrine), Amiodarone, Classification of Vasoactive drugs, Clevidipine, Digoxin, Dobutamine, Dopamine, Levosimendan, Levosimendan vs Dobutamine, Milrinone, Noradrenaline, Phenylephrine, Sodium Nitroprusside (SNiP), Sotalol, Vasopressin
Neurological: Dexmedetomidine, Ketamine, Levetiracetam, Lignocaine, Lithium, Midazolam, Physostigmine, Propofol, Sodium Valproate, Sugammadex, Thiopentone
Endocrine: Desmopressin, Glucagon Therapy, Medications and Thyroid Function
Gastrointestinal: Octreotide, Omeprazole, Ranitidine, Sucralfate, Terlipressin
Genitourinary: Furosemide, Mannitol, Spironolactone
Haematological: Activated Protein C, Alteplase, Aprotinin, Aspirin, Clopidogrel, Dipyridamole, DOACs, Factor VIIa, Heparin, LMW Heparin, Protamine, Prothrombinex, Tenecteplase, Tirofiban, Tranexamic Acid (TXA), Warfarin
Antimicrobial: Antimicrobial Dosing and Kill Characteristics, Benzylpenicillin, Ceftriaxone, Ciprofloxacin, Co-trimoxazole / Bactrim, Fluconazole, Gentamicin, Imipenem, Linezolid, Meropenem, Piperacillin-Tazobactam, Rifampicin, Vancomycin
Analgesic: Alfentanil, Celecoxib, COX II Inhibitors, Ketamine, Lignocaine, Morphine, NSAIDs, Opioids, Paracetamol (Acetaminophen), Paracetamol in Critical Illness, Tramadol
Miscellaneous: Activated Charcoal, Adverse Drug Reactions, Alkali Therapies, Drug Absorption in Critical Illness, Drug Infusion Doses, Epidural Complications, Epidural vs Opioids in Rib Fractures, Magnesium, Methylene Blue, Pharmacology and Critical Illness, PK and Obesity, PK and ECMO, Sodium Bicarbonate Use, Statins in Critical Illness, Therapeutic Drug Monitoring, Weights in Pharmacology
Toxicology: Digibind, Flumazenil, Glucagon Therapy, Intralipid, N-Acetylcysteine, Naloxone, Propofol Infusion Syndrome
- Acute pain management (ANZCA guideline 2010)
- Clemente A, Carli F. The physiological effects of thoracic epidural anesthesia and analgesia on the cardiovascular, respiratory and gastrointestinal systems. Minerva Anestesiol. 2008 Oct;74(10):549-63. PMID: 18854796.
- Freise H, Van Aken HK. Risks and benefits of thoracic epidural anaesthesia. Br J Anaesth. 2011 Dec;107(6):859-68. PMID: 22058144.
- Manion SC, Brennan TJ. Thoracic epidural analgesia and acute pain management. Anesthesiology. 2011 Jul;115(1):181-8. PMID: 21606825.
- Parris R. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Epidural analgesia/anaesthesia versus systemic intravenous opioid analgesia in the management of blunt thoracic trauma. Emerg Med J. 2007 Dec;24(12):848-9. PMC2658360.
- Scarci M, Joshi A, Attia R. In patients undergoing thoracic surgery is paravertebral block as effective as epidural analgesia for pain management? Interact Cardiovasc Thorac Surg. 2010 Jan;10(1):92-6. PMID: 19854794.
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

I would suggest that the short duration of blockade can be easily overcome by tunneling the catheter. This is something that can be routinely done. Further, if injuries are missed, it is not due to masking from an epidural if the correct dose is used. It is due to inadequate assessment. There is no evidence to suggest the rate of missed injuries in higher in patients treated with epidural. The side effects – n/v and resp depression are not actually more common in epidural patients vs those treated with opioids.