U Wave
U wave Overview
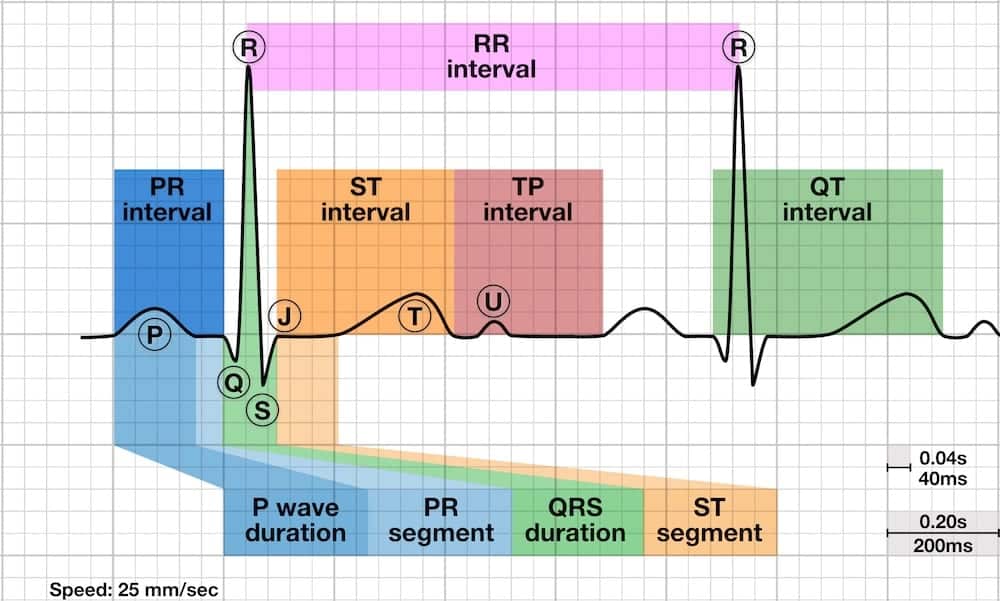
The U wave is a small (0.5 mm) deflection immediately following the T wave
- U wave is usually in the same direction as the T wave.
- U wave is best seen in leads V2 and V3.
Source of the U wave
The source of the U wave is unknown. Three common theories regarding its origin are:
- Delayed repolarisation of Purkinje fibres
- Prolonged repolarisation of mid-myocardial “M-cells”
- After-potentials resulting from mechanical forces in the ventricular wall
Features of Normal U waves
- The U wave normally goes in the same direction as the T wave
- U -wave size is inversely proportional to heart rate: the U wave grows bigger as the heart rate slows down
- U waves generally become visible when the heart rate falls below 65 bpm
- The voltage of the U wave is normally < 25% of the T-wave voltage: disproportionally large U waves are abnormal
- Maximum normal amplitude of the U wave is 1-2 mm
Abnormalities of the U wave
- Prominent U waves
- Inverted U waves
Prominent U waves
U waves are described as prominent if they are
- >1-2mm or 25% of the height of the T wave.
Causes of prominent U waves
Prominent U waves most commonly found with:
Prominent U waves may be present with:
- Hypocalcaemia
- Hypomagnesaemia
- Hypothermia
- Raised intracranial pressure
- Left ventricular hypertrophy
- Hypertrophic cardiomyopathy
Drugs associated with prominent U waves:
- Digoxin
- Phenothiazines (thioridazine)
- Class Ia antiarrhythmics (quinidine, procainamide)
- Class III antiarrhythmics (sotalol, amiodarone)
Note many of the conditions causing prominent U waves will also cause a long QT.
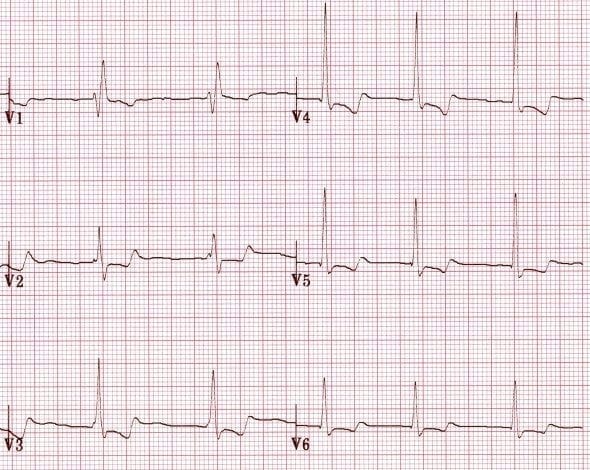
Prominent U waves due to sinus bradycardia
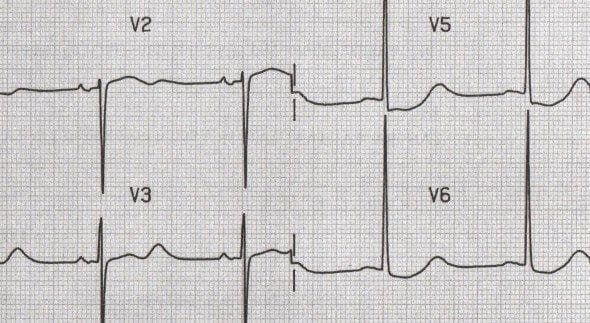
U waves associated with hypokalaemia

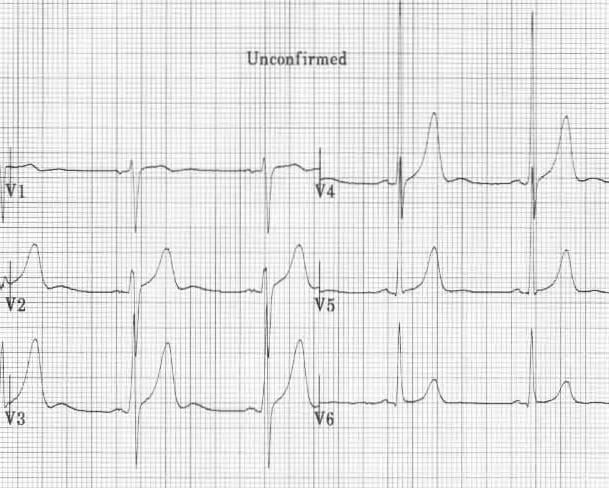
U waves associated with left ventricular hypertrophy
U waves associated with digoxin use
U waves associated with quinidine use
Inverted U waves
- U-wave inversion is abnormal (in leads with upright T waves)
- A negative U wave is highly specific for the presence of heart disease
Common causes of inverted U waves
- Coronary artery disease
- Hypertension
- Valvular heart disease
- Congenital heart disease
- Cardiomyopathy
- Hyperthyroidism
In patients presenting with chest pain, inverted U waves:
- Are a very specific sign of myocardial ischaemia
- May be the earliest marker of unstable angina and evolving myocardial infarction
- Have been shown to predict a ≥ 75% stenosis of the LAD / LMCA and the presence of left ventricular dysfunction
Unstable angina
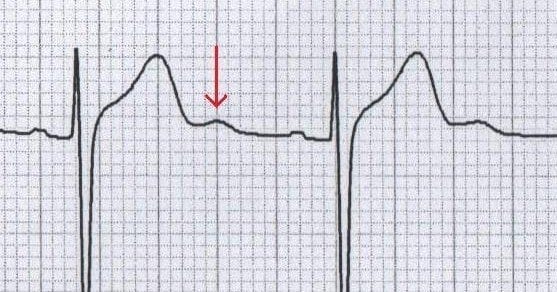
- Inverted U waves in a patient with unstable angina. Reproduced from Girish et al.
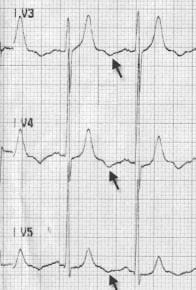
Inverted U waves in Prinzmetal angina

NSTEMI
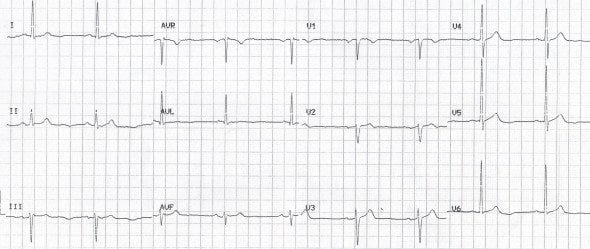
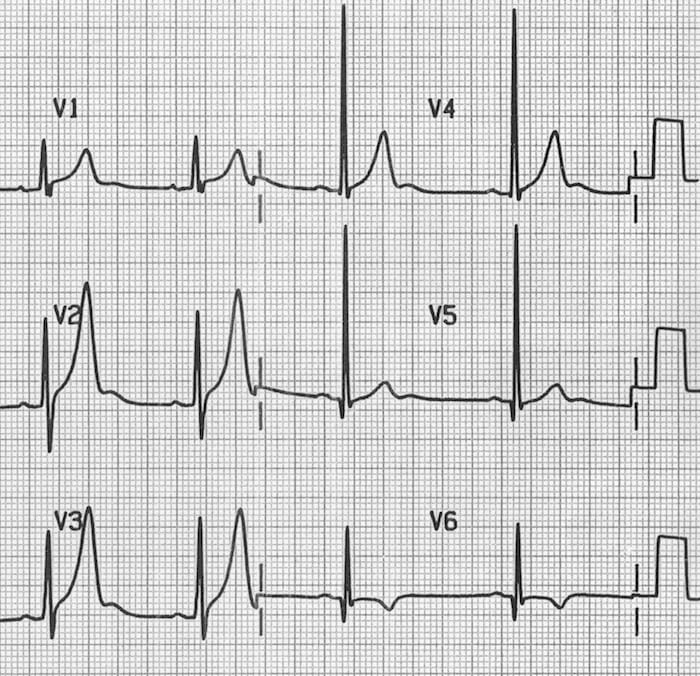
- Note the subtle U-wave inversion in the lateral leads (I, V5 and V6) in this patient with a NSTEMI; these were the only abnormal findings on his ECG.
ECG Library Basics
References
- Sovari AA, Farokhi F, Kocheril AG. Inverted U wave, a specific electrocardiographic sign of cardiac ischemia. Am J Emerg Med. 2007 Feb;25(2):235-7. PMID: 17276833
- Gerson MC, McHenry PL. Resting U wave inversion as a marker of stenosis of the left anterior descending coronary artery. Am J Med. 1980 Oct;69(4):545-50. PMID: 7424944
- Girish MP, Gupta MD, Mukhopadhyay S, Yusuf J, Sunil Roy TN, Trehan V. U wave: an important noninvasive electrocardiographic diagnostic marker. Indian Pacing Electrophysiol J. 2005 Jan 1;5(1):63-5. PMID: 16943944
- Pérez Riera AR, Ferreira C, Filho CF, Ferreira M, Meneghini A, Uchida AH, Schapachnik E, Dubner S, Zhang L. The enigmatic sixth wave of the electrocardiogram: the U wave. Cardiol J. 2008;15(5):408-21. PMID: 18810715
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
