T wave
T wave Overview
The T wave is the positive deflection after each QRS complex. It represents ventricular repolarisation.
Normal T wave characteristics
- Upright in all leads except aVR and V1
- Amplitude < 5mm in limb leads, < 10mm in precordial leads (10mm males, 8mm females)
- Duration relates to QT interval
T wave abnormalities
- Peaked T waves
- Hyperacute T waves
- Inverted T waves
- Biphasic T waves
- ‘Camel Hump’ T waves
- Flattened T waves
Peaked T waves
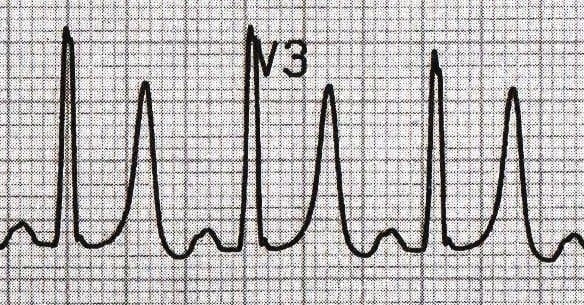
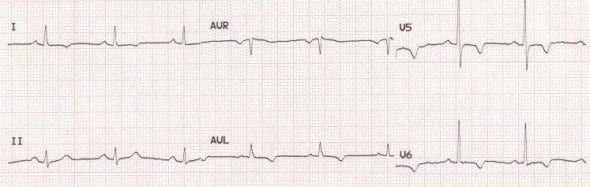
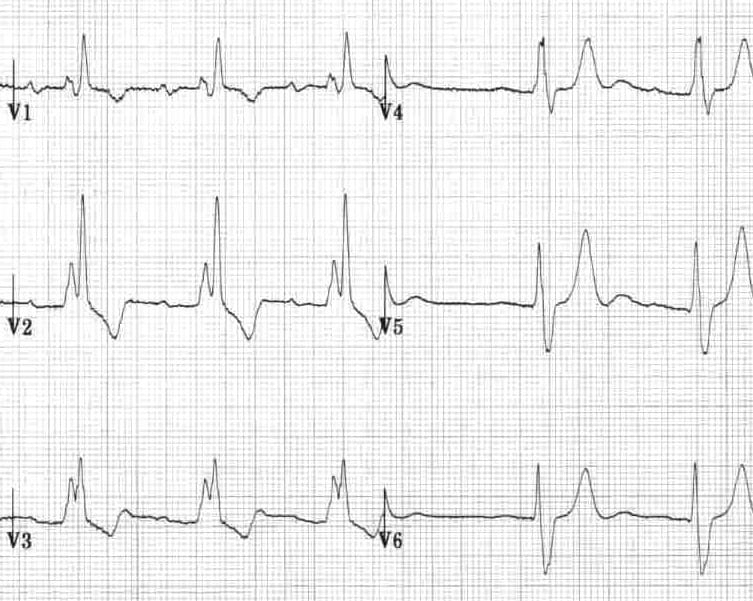
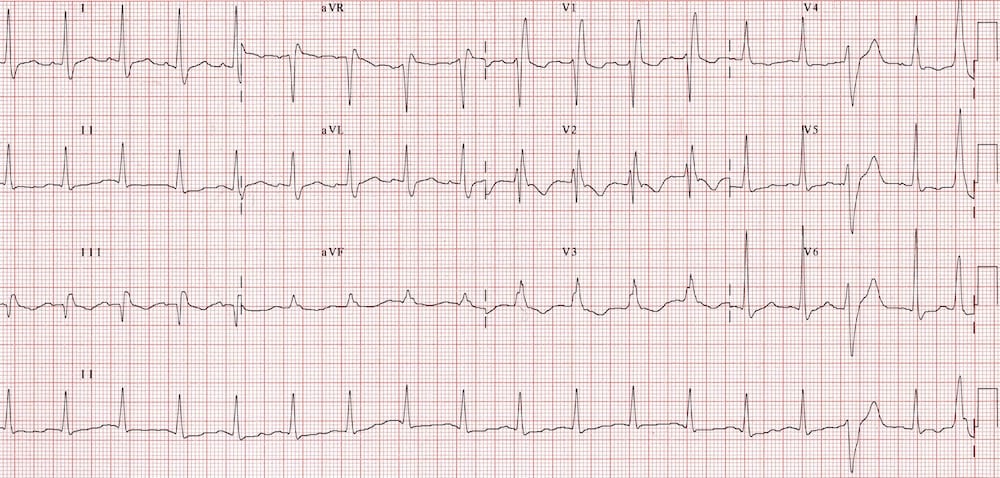
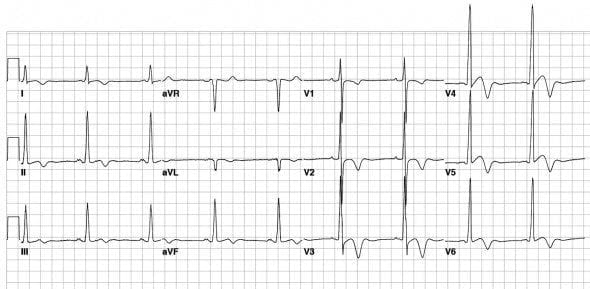
Hyperacute T waves (HATW)
Broad, asymmetrically peaked or ‘hyperacute’ T-waves (HATW) are seen in the early stages of ST-elevation MI (STEMI), and often precede the appearance of ST elevation and Q waves. Particular attention should be paid to their size in relation to the preceding QRS complex, as HATW may appear ‘normal’ in size if the preceding QRS complex is of a small amplitude.
They are also seen with Prinzmetal angina.
Loss of precordial T-wave balance
Loss of precordial T-wave balance occurs when the upright T wave is larger than that in V6. This is a type of hyperacute T wave.
- The normal T wave in V1 is inverted. An upright T wave in V1 is considered abnormal — especially if it is tall (TTV1), and especially if it is new (NTTV1).
- This finding indicates a high likelihood of coronary artery disease, and when new implies acute ischemia
Inverted T waves
Inverted T waves are seen in the following conditions:
- Normal finding in children
- Persistent juvenile T wave pattern
- Myocardial ischaemia and infarction (including Wellens Syndrome)
- Bundle branch block
- Ventricular hypertrophy (‘strain’ patterns)
- Pulmonary embolism
- Hypertrophic cardiomyopathy
- Raised intracranial pressure
** T wave inversion in lead III is a normal variant. New T-wave inversion (compared with prior ECGs) is always abnormal. Pathological T wave inversion is usually symmetrical and deep (>3mm).
Paediatric T waves
Persistent Juvenile T-wave Pattern
- T-wave inversions in the right precordial leads may persist into adulthood and are most commonly seen in young Afro-Caribbean women
- Persistent juvenile T-waves are asymmetric, shallow (<3mm) and usually limited to leads V1-3
Myocardial Ischaemia and Infarction
T-wave inversions due to myocardial ischaemia or infarction occur in contiguous leads based on the anatomical location of the area of ischaemia/infarction:
- Inferior = II, III, aVF
- Lateral = I, aVL, V5-6
- Anterior = V2-6
NOTE:
- Dynamic T-wave inversions are seen with acute myocardial ischaemia
- Fixed T-wave inversions are seen following infarction, usually in association with pathological Q waves
Bundle Branch Block
In bundle branch block, T-wave inversion is an expected finding, even in the absence of ischaemia:
- Appropriate discordance refers to the fact that abnormal depolarisation (such as in bundle branch block) should be followed by abnormal repolarisation, which appears discordant to the preceding QRS complex in the form of ST-depression and T-wave inversion
Left Bundle Branch Block
- Left bundle branch block produces T-wave inversion in the lateral leads I, aVL and V5-6
Right Bundle Branch Block (RBBB)
- Right bundle branch block produces T-wave inversion in the right precordial leads V1-3
Ventricular Hypertrophy
Left Ventricular Hypertrophy (LVH)
- Left ventricular hypertrophy (LVH) produces T-wave inversion in the lateral leads I, aVL, V5-6 (left ventricular ‘strain’ pattern), with a similar morphology to that seen in LBBB
Right Ventricular Hypertrophy (RVH)
- Right ventricular hypertrophy produces T-wave inversion in the right precordial leads V1-3 (right ventricular ‘strain’ pattern) and also the inferior leads (II, III, aVF)
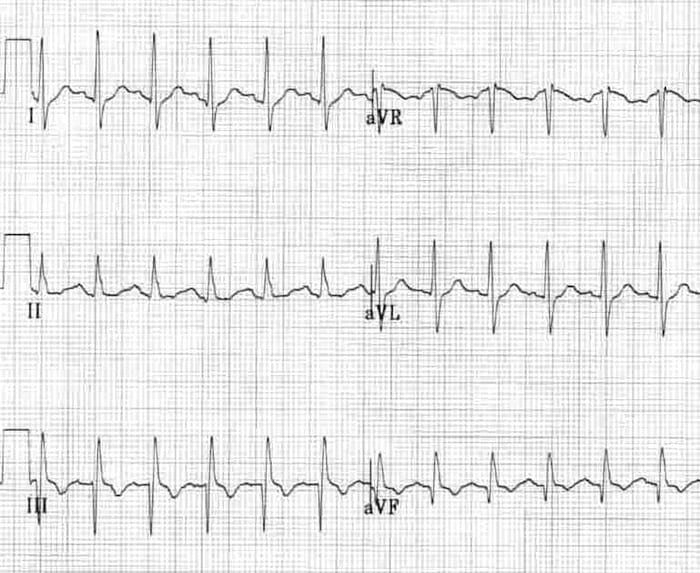
Pulmonary Embolism
- Acute right heart strain (e.g. secondary to massive pulmonary embolism) produces a similar pattern to RVH
- T-wave inversions in the right precordial (V1-3) and inferior (II, III, aVF) leads
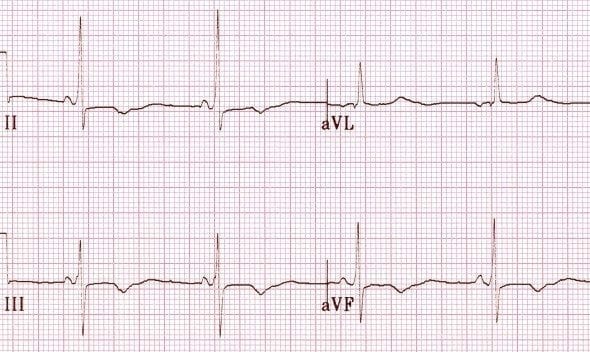
SI QIII TIII
- Pulmonary embolism may also produce T-wave inversion in lead III as part of the SI QIII TIII pattern
- S wave in lead I, Q wave in lead III, T-wave inversion in lead III
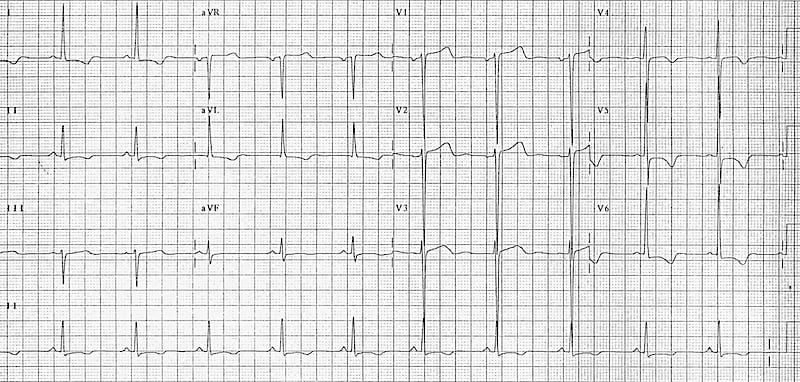
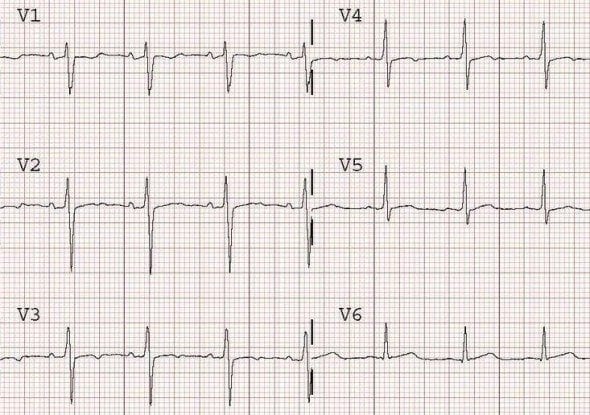
Hypertrophic Cardiomyopathy (HCM)
- Hypertrophic Cardiomyopathy is associated with deep T wave inversions in all the precordial lead
Raised intracranial pressure (ICP)
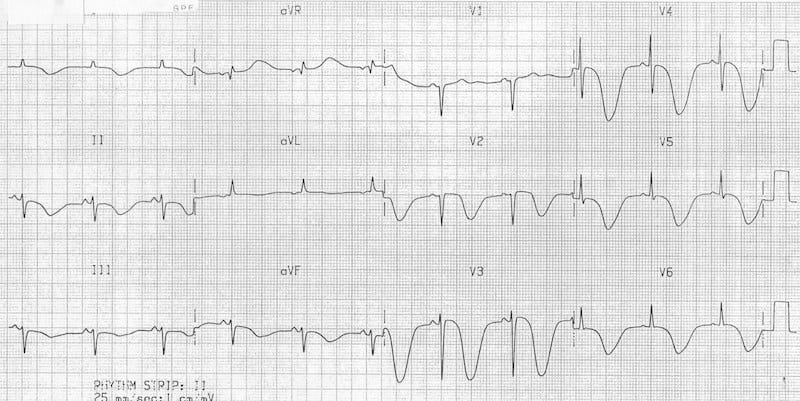
- Events causing a sudden rise in intracranial pressure (e.g. subarachnoid haemorrhage) produce widespread deep T-wave inversions with a bizarre morphology
Biphasic T waves
There are two main causes of biphasic T waves:
The two waves go in opposite directions:
Biphasic T waves due to ischaemia – T waves go UP then DOWN
Biphasic T waves due to Hypokalaemia – T waves go DOWN then UP
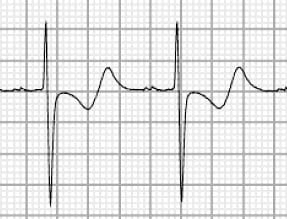
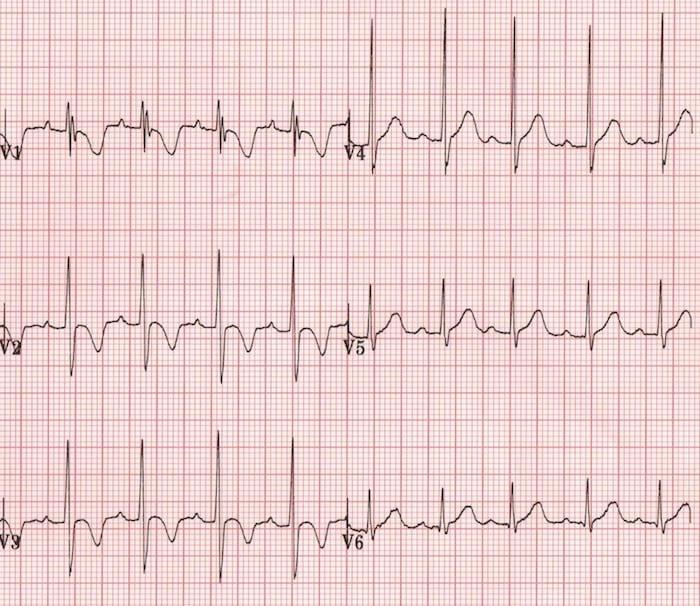
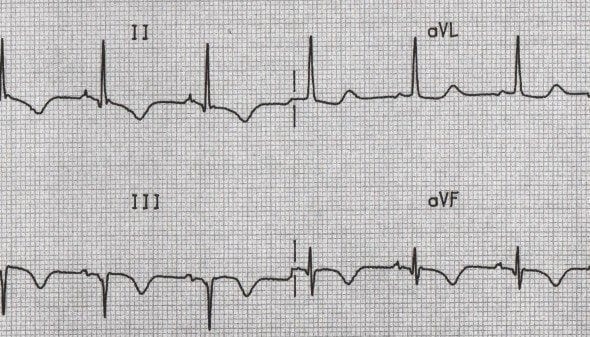
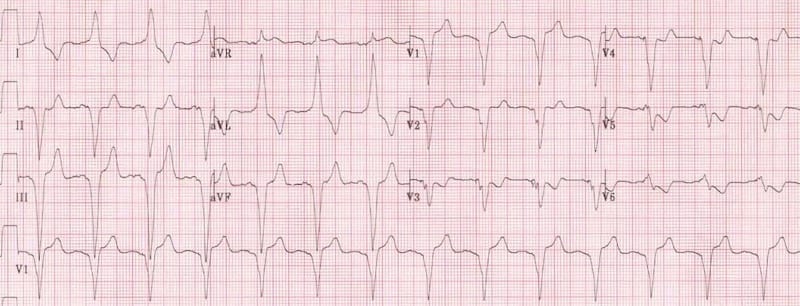
Wellens Syndrome
Wellens syndrome is a pattern of inverted or biphasic T waves in V2-3 (in patients presenting with/following ischaemic sounding chest pain) that is highly specific for critical stenosis of the left anterior descending artery.
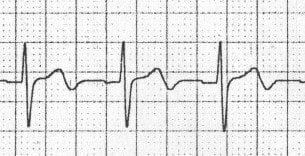
There are two patterns of T-wave abnormality in Wellens syndrome:
- Type A = Biphasic T waves with the initial deflection positive and the terminal deflection negative (25% of cases)
- Type B = T-waves are deeply and symmetrically inverted (75% of cases)
Note: The T waves evolve over time from a Type A to a Type B pattern
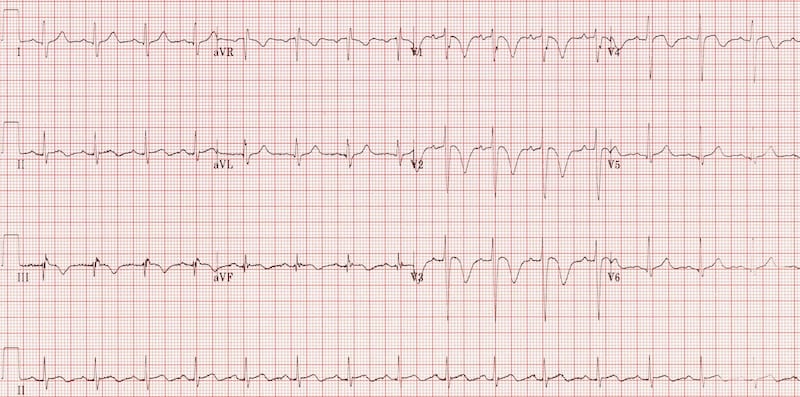
Wellens Type A
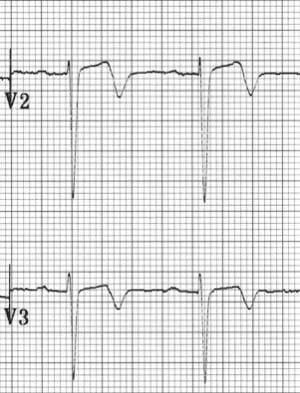
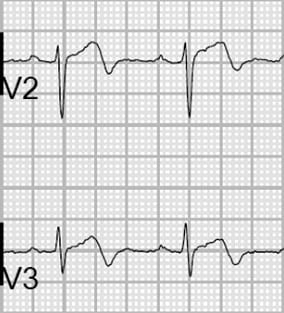
Wellens Type B

‘Camel hump’ T waves
‘Camel hump’ T waves is a term used by Amal Mattu to describe T-waves that have a double peak. There are two causes for camel hump T waves:
- Prominent U waves fused to the end of the T wave, as seen in severe hypokalaemia
- Hidden P waves embedded in the T wave, as seen in sinus tachycardia and various types of heart block
Flattened T waves
Flattened T waves are a non-specific finding, but may represent
- Ischaemia (if dynamic or in contiguous leads) or
- Electrolyte abnormality, e.g. hypokalaemia (if generalised)
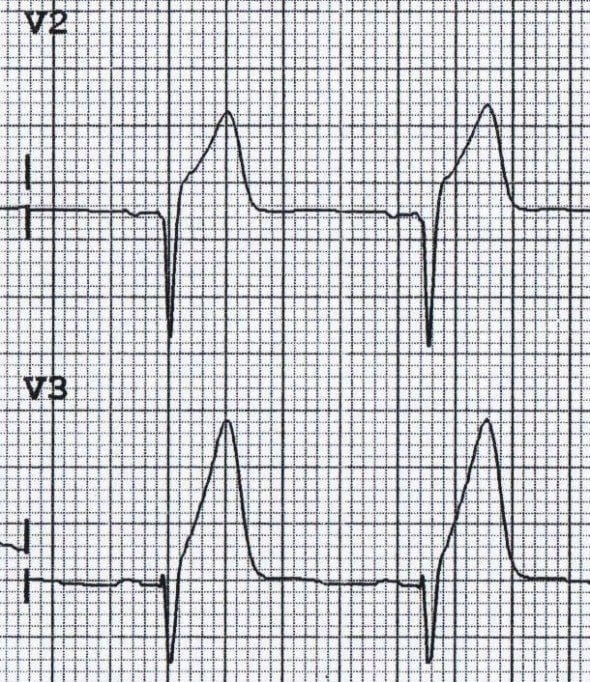
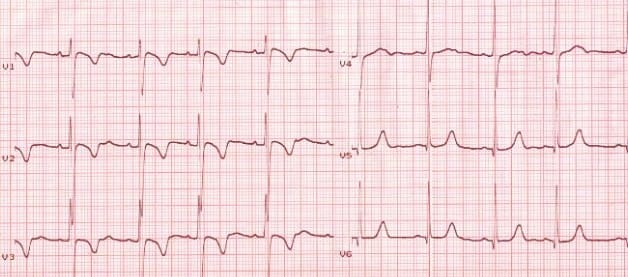
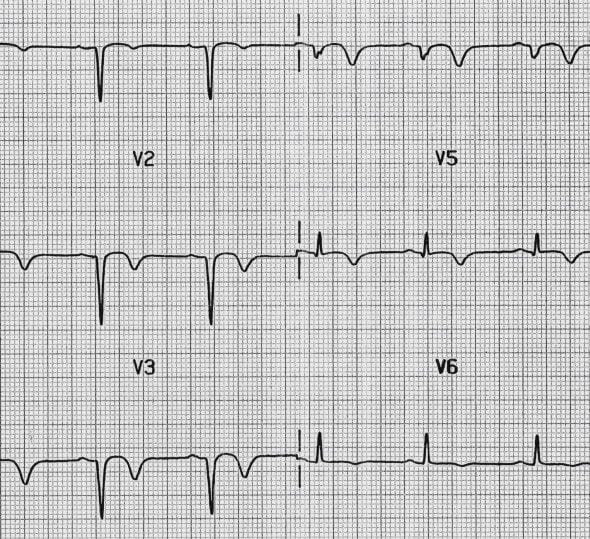
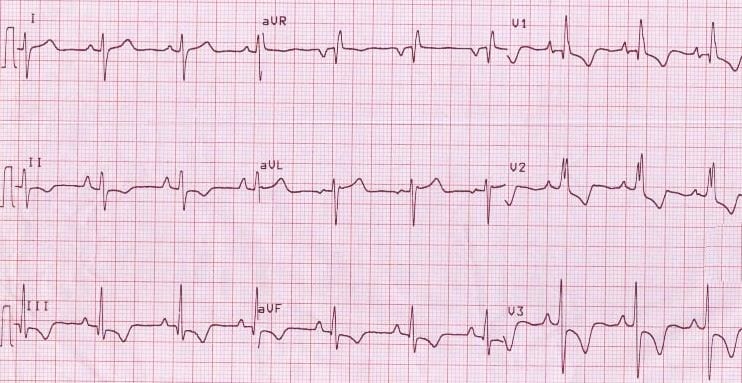
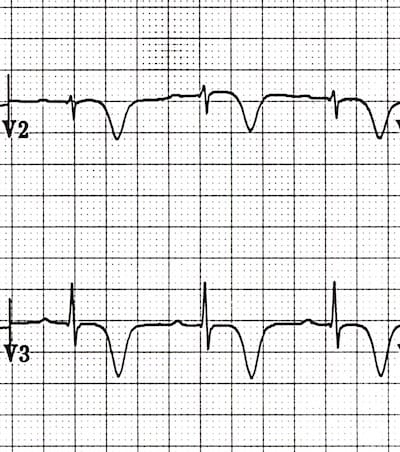
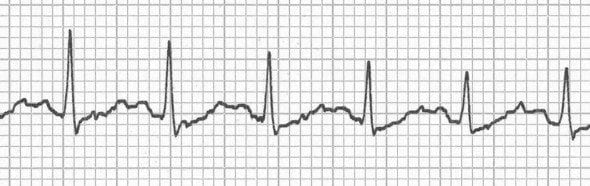
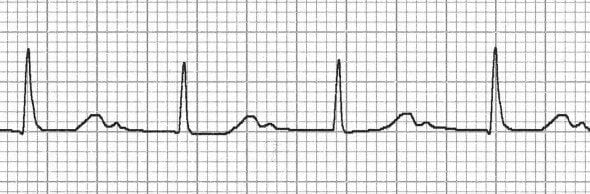
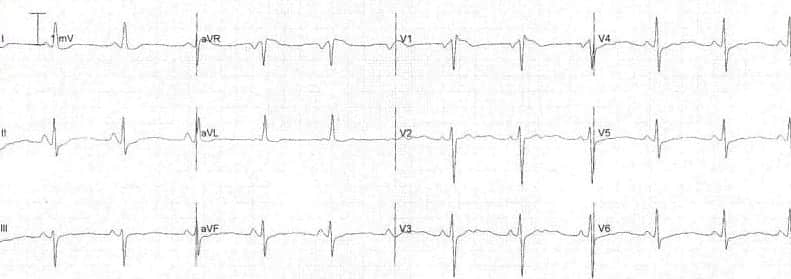
Ischaemia
Dynamic T-wave flattening due to anterior ischaemia (above). T waves return to normal once the ischaemia resolves (below).
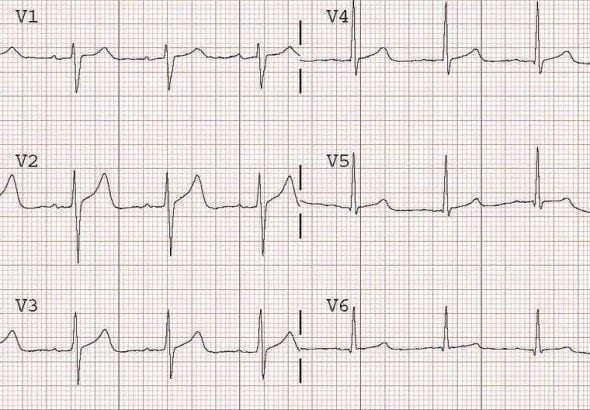
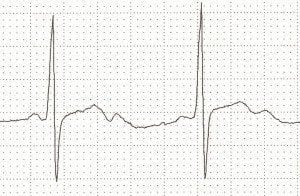
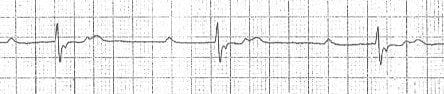
Hypokalaemia
Note global T-wave flattening in hypokalaemia associated with prominent U waves in the anterior leads (V2 and V3).
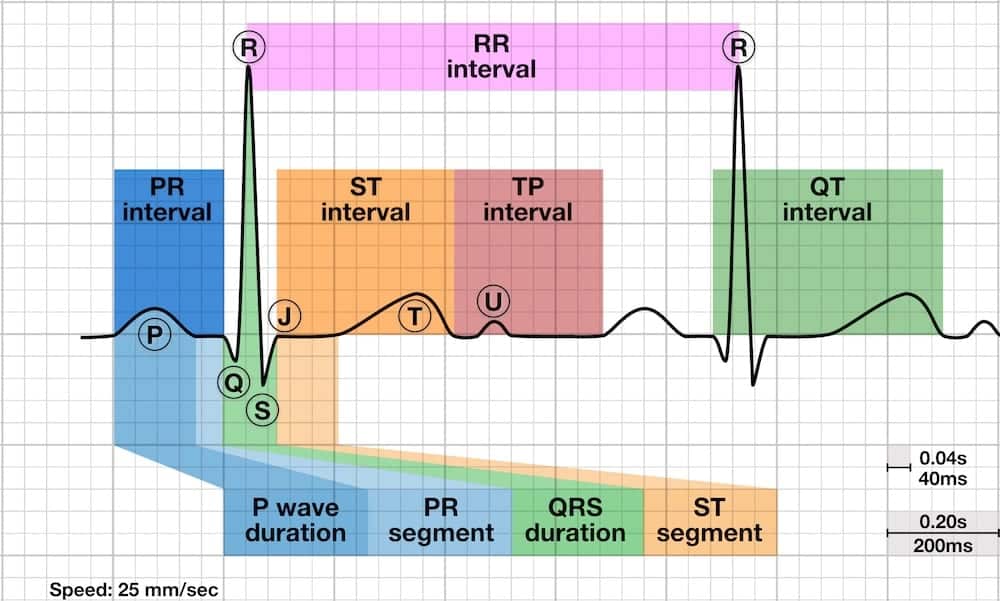
ECG Library Basics
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
Advanced Reading
- Brady WJ, Truwit JD. Critical Decisions in Emergency and Acute Care Electrocardiography
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric
- Wagner GS. Marriott’s Practical Electrocardiography 12e
- Chan TC. ECG in Emergency Medicine and Acute Care
- Rawshani A. Clinical ECG Interpretation
- Mattu A. ECG’s for the Emergency Physician
- Hampton JR. The ECG In Practice, 6e
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
